Influence of Electroacupuncture at Taichong (LR 3) and Ququan (LR 8) on Hepatic Hemodynamics
,3
1 College of Acupuncture and Tuina, Shandong University of Traditional Chinese Medicine, Jinan 250355, China
2 Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250011, China
3 Shan Qiu-hua’s Inheritance Studio of National Famous Traditional Chinese Medicine Experts, Jinan 250011, China
4 Yucheng People’s Hospital, Yucheng 251200, China
CLINICAL STUDY
Influence of Electroacupuncture at Taichong (LR 3) and Ququan (LR 8) on Hepatic Hemodynamics
Cui Hua-feng1,2,3, Han Gui-yin4, Li Dong2, Liu Jing4, Shan Qiu-hua2,3
1 College of Acupuncture and Tuina, Shandong University of Traditional Chinese Medicine, Jinan 250355, China
2 Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250011, China
3 Shan Qiu-hua’s Inheritance Studio of National Famous Traditional Chinese Medicine Experts, Jinan 250011, China
4 Yucheng People’s Hospital, Yucheng 251200, China
Author: Cui Hua-feng, grade 2012 doctor degree candidate of Shandong University of Traditional Chinese Medicine, attending physician.
E-mail: cuihuafeng@139.com
Objective: To observe the influence of electroacupuncture (EA) at Taichong (LR 3) and Ququan (LR 8) on hepatic hemodynamics in the patients with chronic hepatic diseases.
Methods: Sixty cases with chronic hepatic diseases were randomly divided into a Taichong (LR 3) group and a Ququan (LR 8) group, 30 cases in each group, and were respectively treated with electroacupuncture at Taichong (LR 3) and Ququan (LR 8). The blood flow results of the hepatic artery and portal vein by color ultrasonic test were used as the objective indexes, to compare and observe the hemodynamics changes of the hepatic artery and portal vein in the patients before and after EA.
Results: After EA, in Taichong (LR 3) group, the average velocity, the lowest velocity, resistance indexes and the highest velocity of blood flow of the hepatic artery, and the highest velocity, average velocity of blood flow of the portal vein, blood flow volume of the portal vein (PVBF), total blood flow volume of the liver (TLBF), and Doppler blood perfusion indexes of the hepatic artery (DPI) were all statistically different from those before intervention (allP<0.05). In Ququan (LR 8)group, the highest velocity, average velocity, lowest velocity and resistance indexes of blood flow of the hepatic artery, and the highest velocity and average velocity of blood flow of the portal vein, and PVBF were significantly different from those before intervention (P<0.05). The TLBF and DPI were significantly different from those before intervention (P<0.01). All various indexes were not statistically different between the two groups.
Conclusion: EA at Taichong (LR 3) and Ququan (LR 8) can speed up blood flow velocity of the portal vein, increase PVBF, increase the TLBF, increase the resistance indexes of the hepatic artery, decrease the blood flow velocity of the hepatic artery, and decrease DPI in the liver.
Point, Taichong (LR 3); Point, Ququan (LR 8); Electroacupuncture;Acupuncture Therapy; Liver; Hemodynamics
Yuan-Primary points are located at the places where Yuan-Primary qi of Zang-fu organs go through and stay. He-Sea points have the effects to dredge the meridians and circulate qi and blood. In traditional Chinese medicine, the liver stores blood and regulate blood volume. The average velocity of blood flow and the diameter of the hepatic artery and portal vein can be recorded by the vascular ultrasonic technology, so as to observe blood flow volume of the main blood vessels in the liver. In recent years, we observed the influence of electroacupuncture (EA) at Taichong (LR 3) and Ququan (LR 8) on hepatic hemodynamics of patients with chronic hepatic diseases. Now, the report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
By referring to the diagnostic criteria of chronic hepatitis and hepatic cirrhosis inPreventive and Therapeutic Protocols for Viral Hepatitisjointly revised by Society of Infectious Diseases, and Society of Hepatology of Chinese Medical Association in September of 2000[1].
1.2 Inclusion criteria
In conformity with the above diagnostic criteria of chronic hepatitis, hepatic fibrosis and compensatory hepatic cirrhosis; no administration of any vasoactive drugs in 24 h and fasting for 12 h before the trial; no severe cardiocerebrovascular diseases, and hematopoietic and endocrine diseases in laboratory examinations, all signed informed consent.
1.3 Exclusion criteria
Patients with primary and secondary liver cancer, hepatic hemangioma, thrombosis of the portal vein, hepatic fatty tumor, liver tuberculosis and relevant diseases that affect blood flow of the hepatic artery and portal vein; with the age below 18 or above 65 years old.
1.4 Statistical methods
The statistic management was processed by the SPSS 13.0 version statistical software. The counting data were expressed as mean ± standard deviationFor information complying with the normality and homogeneity of variance, the data before and after EA in each group were calculated with the pairedt-test. For information not complying with the normality and homogeneity of variance, the rank sum test was adopted.
1.5 General data
In this study, totally 60 cases with chronic hepatitis, including outpatients and inpatients were enrolled. The patients were randomly divided into a Taichong (LR 3) group (n=30) and a Ququan (LR 8) group (n=30) according to the random number table.
By the run test, the samples complied with the randomized grouping. The differences in the gender, age, duration, and pathological information between the two groups were not statistically significant (Table 1), indicating that the two groups were comparable. During the observation, two cases quitted the trial themselves, and one case was terminated because of faint during acupuncture treatment in Taichong (LR 3) group, with no hemodynamics indexes obtained. The above three cases were counted as dropped-out cases.
Please see Figure 1 for the clinical flow chart of the patients in the two groups.
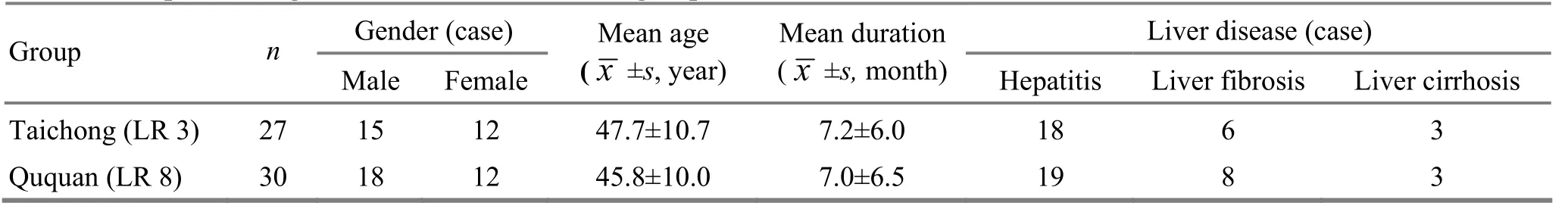
Table 1. Comparison of general data between the two groups
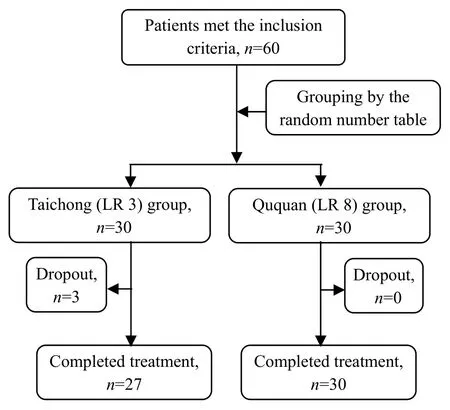
Figure 1. Clinical flow chart of the two groups
2 Research Methods
2.1 Instruments
EnVisor HD color ultrasound diagnostic equipment manufactured by Philips Company and Great Wall KWD-808 I pulse EA apparatus manufactured by Changzhou Wujin Great Wall Medical Equipments Co. Ltd. were used.
2.2 Grouping management
2.2.1 Taichong (LR 3) group
First-time ultrasound B operation: With the patient in the supine position, the ultrasound examination was operated with the probe at frequency of 2.5 MHz to repeatedly detect till clear trunk of the portal vein and hepatic artery and blood flow signals appeared, with the included angle between sound speed and blood flow direction within 60°. The sample volume was adjusted to be able to surround the blood vesselsfor obtaining the blood flow signals of time-space domain, so as to record the relevant test indexes.
Operation: Acupuncture was given after fiveminute rest following ultrasound B examination. After the patient took a sitting position, the skin of the points was cleaned with 75% alcohol cotton. Filiform needle brand Hwato of 0.30 mm in diameter and 40 mm in length was inserted into Taichong (LR 3) perpendicularly for 0.8-1.0 cun and manipulated with even lifting-thrusting and twisting technique. After the arrival of the needling sensation, brand Great Wall KWD-808 I pulse EA apparatus was connected, and Taichong (LR 3) was linked with the negative electrode of EA apparatus (effective electrode), on the Liver Meridian, the site 1 cun above Taichong (LR 3) was connected with the positive electrode (ineffective electrode). After the ineffective electrode was disinfected with 75% alcohol cotton, the magnetic electrode of pulse EA apparatus as the conductive electrode of an ineffective electrode was covered with medical tape to fix the ineffective electrode and stimulated with direct current, sparsedense wave, at frequency of 2 Hz/100 Hz, with the stimulating intensity within the patient’s tolerance, continuously for 25 min.
Second-time ultrasound B operation: The needles were taken out after continuous stimulation for 25 min. The ultrasound examination was done immediately by the method before acupuncture, to record the relevant indexes.
2.2.2 Ququan (LR 8) group
First-time ultrasound B operation: As same as the Taichong (LR 3) group.
Operation: Ququan (LR 8) was connected with the negative electrode of EA apparatus (effective electrode). On the Liver Meridian, the site 1 cun above Ququan (LR 8) was connected with the positive electrode (ineffective electrode). The parameters of EA apparatus and the stimulating time were as same as those in Taichong (LR 3) group.
Second-time ultrasound B operation: As same as the Tachong (LR 3) group.
3 Results Observation
3.1 Observed indexes
3.1.1 Hepatic artery
The highest blood flow velocity (Vmax, cm/s), the lowest blood flow velocity (Vmin, cm/s), the average blood flow velocity (Vmean, cm/s), blood vessel diameter (D, cm), pulse index of the hepatic artery (PI), resistance index of the hepatic artery (RI)=(Vmax- Vmin) ÷ Vmax.
3.1.2 Portal vein
The highest blood flow velocity (Vmax, cm/s), average blood flow velocity (Vmean, cm/s), and the blood vessel diameter (D, cm).
3.1.3 Sectional area of relevant blood vessels and others
The sectional area of the relevant blood vessels was calculated (A)=π×(D÷2)2, and the blood flow volume of the relevant blood vessels was A×Vmean× 60 (mL/min), so as to calculate the following research indexes: blood flow volume of the hepatic artery (HABF, mL/min), blood flow volume of the portal vein (PVBF, mL/min), total blood flow volume of the liver (TLBF, mL/min)=HABF+PVBF, Doppler blood perfusion index of the hepatic artery (DPI)=HABF÷ TLBF.
The average value of the two breathing cycles was taken as blood flow index of the portal vein, and the average value of the five cardiac cycles was taken as blood flow index of the hepatic artery, to record the relevant observed indexes.
3.2 Research results
3.2.1 Change of blood flow of hepatic artery before and after EA (Table 2)
In comparison of before and after intervention, in Taichong (LR 3) group, blood flow indexes of the hepatic artery, such as Vmean, Vminand RI were significantly different (P<0.05), and Vmax, D, HABF and were not significantly different (P>0.05), indicating that after EA at Taichong (LR 3) in the patients with chronic hepatic diseases, blood flow velocity decreased remarkably and resistance index increased remarkably, but there was no obvious change in blood flow volume, interior diameter and pulse index of the hepatic artery.
In comparison of before and after intervention, in Ququan (LR 8) group, the blood flow indexes of the hepatic artery, such as Vmean, Vminand RI were significantly different (P<0.05), and D, HABF, and PI not significantly different (P>0.05), indicating that after EA at Ququan (LR 8) in the patients with chronic hepatic diseases, blood flow velocity decreased remarkably and resistance index increased remarkably, but there was no obvious change in blood flow volume, interior diameter and pulse index of the hepatic artery.
3.2.2 Change of blood flow of portal vein before and after EA (Table 3)
In Taichong group, in comparison with before EA, blood flow indexes of the portal vein, such as Vmax, Vmeanand PVBF were significantly different (P<0.05), and the interior diameter of the portal vein was not significantly different (P>0.05) after EA, indicatingthat after EA at Taichong (LR 3) in the patients with chronic hepatic diseases, blood flow velocity and PVBF increased remarkably, but there was no obvious change in the interior diameter of the portal vein.
In Ququan (LR 8) group, in comparison with before EA, blood flow indexes of the portal vein, such as Vmax, Vmeanand PVBF were significantly different (P<0.05), the change PVBF was very significantly different in particular (P<0.01), and the interior diameter of the portal vein was not significantly different (P>0.05) after EA, indicating that after EA at Ququan (LR 8) in the patients with chronic hepatic diseases, blood flow velocity and PVBF increased remarkably, but there was no obvious change in the interior diameter of the portal vein.
3.2.3 Change of TLBF and DPI before and after EA (Table 4)
After EA at Taichong (LR 3) and Ququan (LR 8) in the patients with chronic hepatic diseases, TLBF remarkably increased, and the portion of blood flow of the hepatic artery in the TLBF decreased significantly.
Table 2. Change of blood flow of hepatic artery before and after EA between the two groups
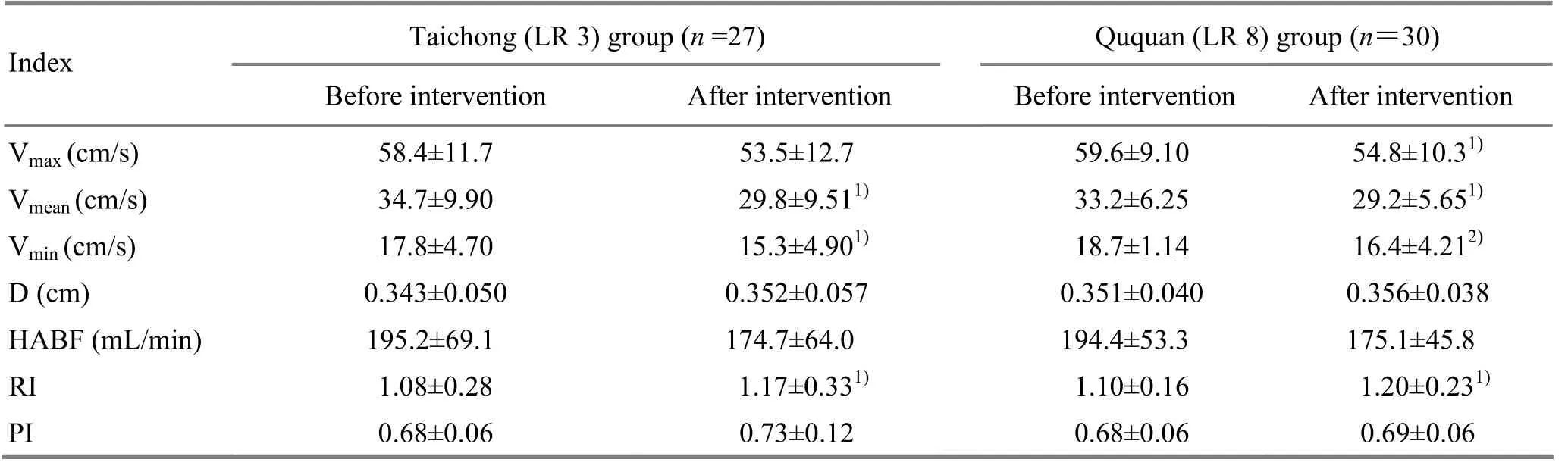
Table 2. Change of blood flow of hepatic artery before and after EA between the two groups
Note: Compared with the same group before intervention, 1) P<0.05,2) P<0.01
?
Table 3. Change of blood flow of portal vein before and after EA between the two groups
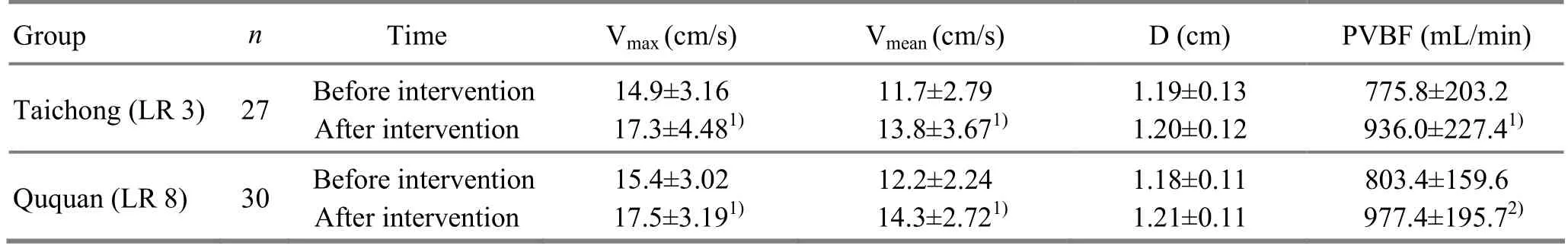
Table 3. Change of blood flow of portal vein before and after EA between the two groups
Note: Compared with the same group before intervation, 1) P<0.05,2) P<0.01
?
Table 4. Changes of TLBF and DPI
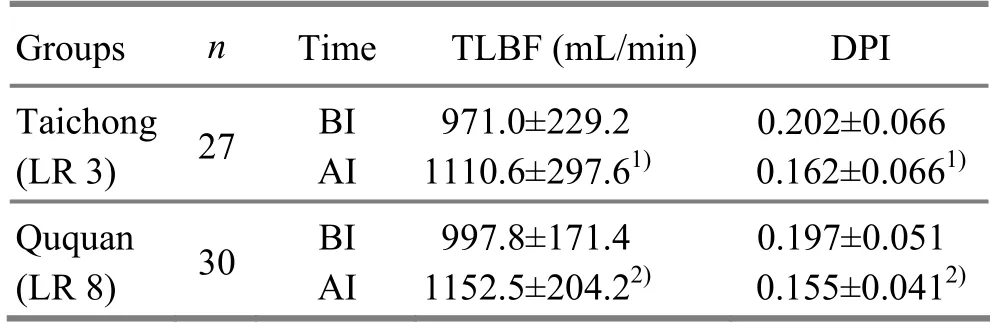
Table 4. Changes of TLBF and DPI
Note: BI=Before intervention; AI=After intervention; compared with the same group before intervention, 1) P<0.05, 2) P<0.01
?
3.3 Analysis of research results
The results from this study showed that the regulatory effects of the hepatic blood flow were not statistically different between the Taichong (LR 3) group and Ququan (LR 8) group, indicating that in improvement of the hepatic blood supply, two points have similar effects, both can increase the PVBF and the TLBF, and the blood flow volume of the hepatic artery slightly decreases due to the buffering effect of the hepatic artery, so as to cause the decrease of DPI.
4 Discussion
Qi of five Zang organs flows into Yuan-Primary points. Yuan-Primary points can reflect the pathological changes of the relevant Zang-fu organs and also can be used to treat these pathological changes. When pathological changes occur in Zang-fu organs, the corresponding Yuan-Primary points can be selected for EA treatment, so as to dredge the meridians, regulate and harmonize qi and blood, and hence restore the functions of Zang-fu organs.
Five Shu-Transmitting points are the commonly used points in clinic, listed in turns by the order of Jing-Well, Xing-Spring, Shu-Stream, Jing-River, and He-Sea points from the terminals of the four limbs to the elbow and knee, and have the effects to dredge the meridians and circulate qi and blood to nourish the whole body. He-Sea points in the five Shu-Transmitting points have the effects to treat the pathological changes induced by adverse flow of qi and problems of Zang-fu organs. As a He-Sea point, Ququan (LR 8) can be used to dredge and regulate qi and blood of the Liver Meridian.
The function of the liver in storing blood means that the liver has the dual effects to store blood and regulate blood volume. The liver has the dual blood supply: the hepatic artery and portal vein. The hepatic artery comes from the abdominal artery and the portal vein collects the venous blood from the digestive tract, spleen and pancreas. Normally, 70%-80% blood supply of the liver comes from the portal vein, only 20%-30% from the hepatic artery. But, oxygen volume supplying to the liver is exactly contrary, and the functions to transport the nutrients and metabolites are mainly realized by the portal vein. The mutual regulatory function exists between the hepatic artery and portal vein. The changes take place in the hemodynamics of the hepatic artery and portal vein in patients with chronic hepatic diseases. The diameters of the blood vessels in the venous system are enlarged in liver cirrhosis than in chronic hepatitis, and blood flow velocity slows down and congestion index is elevated, and blood flow volume increases more obviously in the patients with grade B liver cirrhosis than in the patient with chronic hepatitis[2].
Acupuncture can alleviate pain and regulate the body movement, functions of the internal organs, endocrine activities and immune reaction. The acupuncture effects depend on the completeness of the reflex arc. The reflex center of acupuncture is very complicated and should be multi-polar, including almost all cerebral structures from the spinal cord, limbic system and cerebral cortex. Judging from the angle of the neurophysiology, the needling signals of the points and afferent impulses from the internal organs can converge in the spinal ganglia and various levels of the centers from the spinal cord to the cerebral cortex, and the existence of the convergence neurons is one of the important factors for appearance of acupuncture effect. Jin GY, et al[3]speculated that under the control of the central nervous system, the reflex effect in the medial region of the leg and foot is overlapped with the reflex effect of the liver. This region is mainly distributed along the Liver Meridian and also is spread to the Spleen Meridian and Kidney Meridian, including Ququan (LR 8), Zhongdu (LR 6), Ligou (LR 5), Zhongfeng (LR 4),Taichong (LR 3), Yinlingquan (SP 9), Sanyinjiao (SP 6), Shangqiu (SP 5), Taixi (KI 3), Rangu (KI 2) and Ganyanxue (Extra) (1-2 cun above the medial malleolus). The best points for hepatic diseases should be located in the reflex zone of the liver. Tao Z, et al[4]observed by HRP technology that afferent nerves of Taichong (LR 3) and Qimen (LR 14) and the afferent nerve of the liver are intersected and overlapped in two ways in 2-4 spinal segments. This might be the foundation of EA at Taichong (LR 3) and Qimen (LR 14) for hepatic diseases. At the same time, it can be used to explain the relevant mechanism of these reflex zones with the liver.
In this study, both Taichong (LR 3) and Ququan (LR 8) are located in the reflex zone of the liver. The nervous reflex arc is overlapped with the nervous reflex arc of the liver. By the consistent nerve conduction, EA at the two points can cause the nervous humoral response of the liver, and cause the change in blood flow stats of the liver. The vasomotor nerves can cause contraction and dilation of the vascular smooth muscle, and the nerve stimulation can be used as an initiating factor to cause the endocrine changes in the liver. The joint effect of the two can regulate blood flow in the liver.
EA can stimulate the release of catecholamines and improve microcirculation inside the body, and adjust the systolic and diastolic status of the blood vessels in the whole body by the autonomic nervous system, and increase blood supply to important organs including the liver[5-6]. EA can promote local blood circulation, improve tissue nutrition, and can also stimulate the parasympathetic nerves, improve blood circulation of the liver and promote the restoration of the damaged liver cells, thus playing a good role in the comprehensive treatment of chronic liver diseases[7].
Some scholars believe that acupuncture can increase blood flow volume of the hepatic artery[8-10]. In this study, EA at Taichong (LR 3) and Ququan (LR 8) causes the changes in the hemodynamics of the hepatic artery and portal vein, increases the velocity of blood flow in the portal vein and increases PVBF. While the total blood flow volume increases in the liver, due to a dynamic balance between the hepatic artery and portal vein, blood flow volume comparatively decreases in the hepatic artery, and Doppler blood perfusion indexes decrease in the hepatic artery. The portal vein is the nourishing blood vessels of the liver. Therefore, with the increase of blood flow volume in the portal vein, the liver will better supplied with the nutrient substances, to promote the repair of the liver cells. The differences between our research results and the research results of some scholars need to be further investigated.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by 3 Shan Qiu-hua’s Inheritance Studio of National Famous Traditional Chinese Medicine Experts.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
[1] Society of Infectious Diseases, Society of Hepatology of Chinese Medical Association. Preventive and therapeutic program for viral hepatitis. Zhonghua Chuanranbing Zazhi, 2001, 19(1): 56-62.
[2] Lu J. Color Doppler ultrasound study on portal vein blood in patients with liver cirrhosis. Jilin Yixue, 2012, 33(36): 7852-7853.
[3] Jin GY, Xiang JJ. Clinical Acupuncture Reflexology. Beijing: Beijing Science and Technology Publishers, 2004: 324.
[4] Tao Z, Li R. The segmental distribution of afferent neurons of liver, and ‘Qimen’ point, ‘Taichong’ point in the spinal ganglion. Zhenci Yanjiu, 1993, 18(3): 228-231.
[5] Li ZT, Yang WN, Xie JP, Zhao YF, Li SJ. Effects of electroacupuncture at different points on mesenteric microcirculation and the VIP content of different viscera in COPD rats. Shanghai Zhenjiu Zazhi, 2013, 32(7): 604-607.
[6] Guan X, Wu HG, Ma XP, Min YJ, Zhao TP, Shi Z, Tan LY. Experimental research of electroacupuncture on ERK phosphorylation in rats of hepatofibrosis. J Acupunct Tuina Sci, 2009, 7(5): 270-273.
[7] Chi XY. Practical Handbook of Electroacupuncture. Beijing: Chinese Science and Technology Publishers, 1991: 130.
[8] Zhang YM, Zhang Q, Xu JN, Li J. Combined acupuncture and medication for treating fatty liver disease. Shanghai Zhenjiu Zazhi, 2011, 30(5): 291-292.
[9] Sai XY, Wang YQ, Duan L. Influence of acupuncture to blood flow of hepatic artery. Zhongguo Zhenjiu, 2000, 20(5): 307-308.
[10] Min YJ, Ma XP, Zhao TP, Wu HG, Shi Z, Yang S, Tan LY, Zhao CY. Effects of electroacupuncture on expressions of collagen type Ⅰtype Ⅲ mRNA in rats of hepatic fibrosis. Shanghai Zhenjiu Zazhi, 2008, 27(8): 43-45.
Translator:Huang Guo-qi
R246.1
: A
Date:December 20, 2013
 Journal of Acupuncture and Tuina Science2014年3期
Journal of Acupuncture and Tuina Science2014年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Observation on Clinical Effects of Tuina plus Hot Compress for Infantile Diarrhea Due to Spleen-kidney Yang Deficiency
- Clinical Study on Point Application Using Chinese Herbal Medicine for Pediatric Chronic Cough
- Therapeutic Effect Observation on Combining Electroacupuncture and Tuina for Migraine
- Therapeutic Efficacy Observation on Combined Taijiquan and Auricular Point Sticking for Perimenopausal Insomnia
- Clinical Study on Fu’s Subcutaneous Needling with Laser for Postherpetic Neuralgia
- Therapeutic Efficacy of Tuina in Treating 48 Cases with Knee Osteoarthritis
