Clinical Study on Point Application Using Chinese Herbal Medicine for Pediatric Chronic Cough
Department of Pediatrics, Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
CLINICAL STUDY
Clinical Study on Point Application Using Chinese Herbal Medicine for Pediatric Chronic Cough
Shen Jian, Zong Nan-wei, Zhu Sheng-guo, Zhao Jun, Gu Ming-da, Zhou Jun-hui
Department of Pediatrics, Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
Author: Shen Jian, M.D., attending physician
Objective: To observe the clinical effect of point application using Chinese herbal medicine for chronic cough in children.
Methods: A total of 200 children with chronic cough were randomly allocated into an observation group and a control group, 100 cases in each group. Conventional Western medication was used for cases in the control group, whereas conventional Western medication plus point application using Chinese herbal medicine were used for cases in the observation group. Changes of indexes including eosinophils (EOS), peak expiratory flow (PEF) and forced expiratory volume in one second (FEV1) were observed before and after treatment. In addition, the clinical effects were compared between the two groups.
Results: After treatment,coughs in children were alleviated in both groups; however, it took a shorter period of time for cough alleviation in the observation group than that in the control group (P<0.01). On the 28th day of treatment, the EOS, PEF and FEV1were improved in both groups (P<0.01), and the improvements were more significant in the observation group (P<0.05). Additionally, the frequencies of cough variant asthma attacks were decreased in both groups, but a better effect in the observation group than the control group.
Conclusion: Complementary point application using Chinese herbal medicine could substantially improve the clinical effect, alleviate coughs and benefit lung functions.
Cough; Asthma; Acupoint Therapy; Point Application Therapy; Children
Chronic cough is one of the common respiratory system problems in children and can be a symptom of many conditions. It is often caused by multiple factors and can last a long period of time. As an important bodily defense mechanism, cough helps to clear secretions and foreign bodies of the airway and thus stop respiratory infection from spreading. However incorrect or delayed treatment of cough can affect the children’s normal life, growth and development. On top of conventional Western medication, we’ve combined point application using Chinese herbal medicine and observed the clinical effect. The results are now summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnosis can be made according to the 2008Diagnosis and Treatment Guidelines for Pediatric Chronic Cough(Trial)[1]: cough lastingover 4 weeks; excluding specific cough due to pulmonary tuberculosis and normal findings in chest X-ray examination.
Cough due to phlegm-heat in Chinese medicine can be diagnosed according to theIntegrated Traditional Chinese and Western Medicine Expert Consensus on Diagnosis and Treatment of Pediatric Cough[2]: cough with sticky phlegm, sweating, and a red tongue with thin yellow coating or slightly greasy coating.
1.2 Inclusion criteria
Those who met the aforementioned diagnostic criteria; aged between 5 and 14 years old; having an allergic constitution or allergic history; and parents of the children were willing to participate in this trial and sign the informed consent.
1.3 Exclusion criteria
Those with complications of severe malnutrition, rickets, primary conditions of heart, liver, kidney and hematopoietic systems or consumptive diseases;having primary immunodeficiency disease or pulmonary hypoplasia; psychogenic cough; those with a long-term use of glucocorticoids, antibiotics and immunosuppressive agents; allergic to above formula ingredients; those who failed to cooperate; and those who tend to be lost to follow-up.
1.4 Rejection and termination criteria
Those who were included in violation of the inclusion criteria; those who failed to follow the treatment protocol; drop-out or loss of follow-up;those with incomplete material affecting efficacy evaluation; those with deteriorated conditions or severe complications and were terminated by researchers; those having severe adverse reactions;and those who were unwilling or unlikely to continue with the clinical observation and therefore quitted or terminated from the trial.
1.5 Statistical method
The Microsoft Excel, SPSS 17.0 version statistical software and superiority test method were used. The measurement data were expressed asPairedt-test was used for intra-group comparison in normal distribution, groupt-test for inter-group comparison, rank sum test for intra-group comparison in abnormal distribution and Chi-square test for numeration data.
1.6 General data
This study adopted randomized controlled clinical trial design. A total of 200 cases from the Outpatient Department of Pediatrics, Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine between May 2012 and October 2012 were randomly allocated into an observation group and a control group, 100 cases in each group. Of 100 cases in the observation group, 37 had upper airway cough syndrome, 50 had cough-variant asthma, 11 had infection-related cough and 2 had other conditions. Of 100 cases in the control group, 36 had upper airway cough syndrome, 51 had cough-variant asthma, 11 had infection-related cough and 2 had other conditions. There were no rejection or drop-out cases in the two groups. The one-year follow-up on cough-variant asthma cases in the two groups had 1 case in the control group dropped out.
Parents of all children signed the informed consent. There were no statistically significant differences in age, gender, duration and disease nature between two groups (P>0.05), indicating that the two groups were comparable (Table 1).
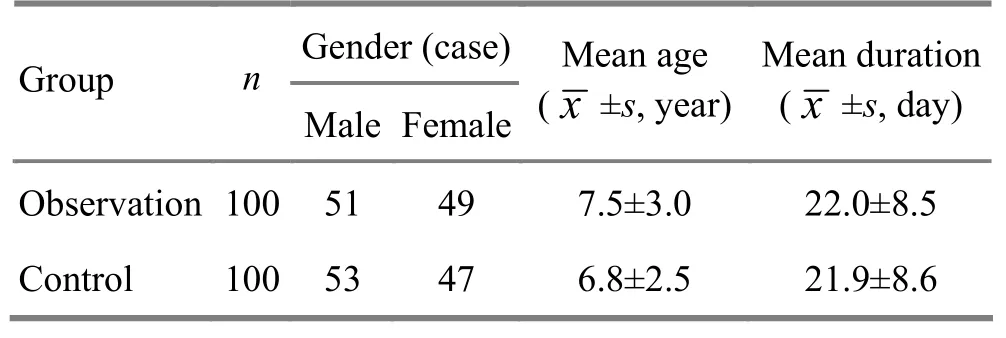
Table 1. Between-group comparison on general materials
2 Treatment Methods
2.1 Observation group
2.1.1 Conventional Western medication
Anti-inflammatory, anti-anaphylaxis and spasmolytic medications were employed, along with sensitivity antibiotics for infection.
2.1.2 Point application therapy
Ingredients of Chinese herbal formula: Coughrelieving formula [powder ofBing Pian(Borneolum Syntheticum),Wu Wei Zi(Fructus Schisandrae Chinensis) andBai Zhi(Radix Angelicae Dahuricae) by the ratio of 1:6:6] and phlegm-resolving formula [powder ofDing Xiang(Flos Caryophylli),Rou Gui(Cortex Cinnamomi),Wu Bei Zi(Galla Chinensis) andWu Wei Zi(Fructus Schisandrae Chinensis) by the ratio of 1:4:4:4]. The formula was provided by Chinese Herbal Preparation Room, Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine.
Points: Tiantu (CV 22) and Dazhui (GV 14).
Method: Apply 0.5 g of cough-relieving formula to Tiantu (CV 22) and 0.5 g of phlegm-resolving formula to Dazhui (GV 14), cover the powder with dressings. The point application was done once a day, 6 h for each time and 3 d for a small course of treatment. There was a 4-day interval after 3 d. Four weeks made up a course of treatment.
2.2 Control group
Children in the control group were treated with the same conventional Western medication as the observation group.
3 Therapeutic Efficacy Observation
3.1 Observation indexes
3.1.1 Signs and symptoms
Using the self-made traditional Chinese medicine symptom scale, clinical signs and symptoms such as cough and phlegm expectoration were observed and recorded before and after treatment.
3.1.2 Eosinophils (EOS), peak expiratory flow (PEF) and forced expiratory volume in one second (FEV1)
EOS, PEF and FEV1were observed before and after treatment. EOS value was obtained by routine blood test and PEF and FEV1by PiKO-1.
3.1.3 The childhood asthma control test (CACT) scale
The CACT scores were observed before and after treatment. Since asthma patients in this group were aged between 4 and 11 and therefore suitable for understanding how asthma was controlled and managed. The score ≤19 indicates poorly controlled asthma; the score ≥20 indicates that asthma is under control.
3.2 Criteria for therapeutic efficacy
This criterion is made according to the 2008Diagnosis and Treatment Guidelines for ChronicPediatric Cough(Trial)[1]andGuiding Principles for Clinical Study of New Chinese Medicines[3]. The Nimodipine method was used to calculate decrease rate of symptom scores.
The decrease rate of symptom score = (Before treatment score — After treatment score) ÷ Before treatment score × 100%.
Clinical control: Almost absence of signs and symptoms, decrease rate of symptom score is ≥95%.
Marked effect: Significant improvement of signs and symptoms, decrease rate of symptom score is between 70% and 94%.
Improvement: Alleviated but unstable recurrent signs and symptoms, decrease rate of symptom score is between 30% and 69%.
Failure: The decrease rate of symptom score is less than 30%.
3.3 Results
3.3.1 Between-group comparison on clinical effects
After 28 d of treatment, there were between-group significant differences in recovery rate and total effective rate (P<0.05) and a better effect in the observation group than that in the control group (Table 2).
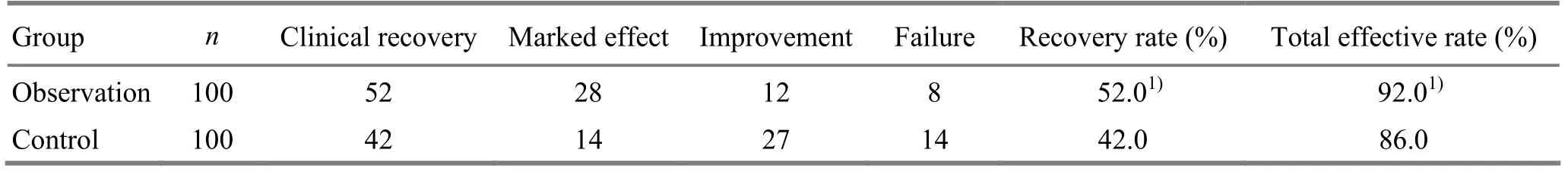
Table 2. Between-group comparison on clinical effects (case)
3.3.2 Between-group comparison on lung functions
After treatment, the FEV1and PEF (% predicted value) in both groups were significantly improved (P<0.01), along with a better effect in the observation group than that in the control group (P<0.05), (Table 3).
3.3.3 Between-group comparison on cough disappearance time
The cough disappearance time in the observation group was (5.2±2.8) d, versus (8.5±1.2) d in the control group, showing a statistically significant difference (P<0.01).
3.3.4 Between-group comparison on annual asthma attacks
The 1-year follow-up on children with coughvariant asthma in two groups (1 case dropped out in the control group) has shown that the annual asthma attacks, EOS and CACT scores in both groups were significantly decreased (P<0.01) after treatment, along with a better result in the observation group than that in the control group (P<0.05), (Table 4).
Table 3. Between-group comparison on lung function indexes before and after treatment (% predicted value)
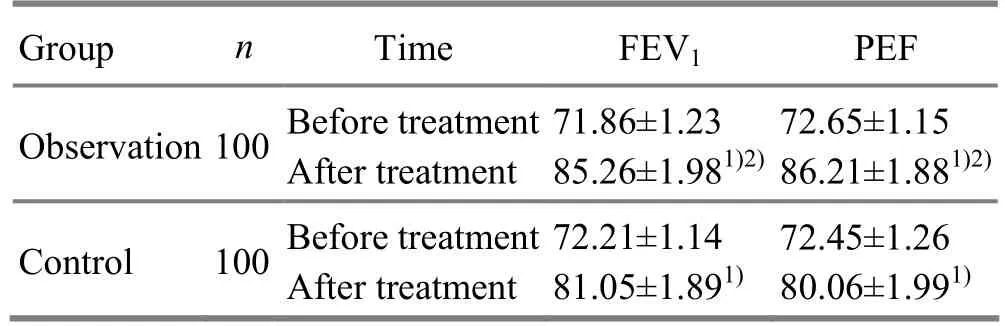
Table 3. Between-group comparison on lung function indexes before and after treatment (% predicted value)
Note: Intra-group comparison between before and after treatment, 1) P<0.01; inter-group comparison after treatment, 2) P<0.05
3.3.5 Adverse reactions
Due to tender skin of children and long-time sticking, 3 patients in the observation group experienced local skin redness or mild itch and 1 patient had mild skin ulceration, which were alleviated 2 d later after local cleaning and application of Iodophors or Fluocinolone Acetonide.
Table 4. Between-group comparison on frequency of annual asthma attacks, EOS and CACT changes
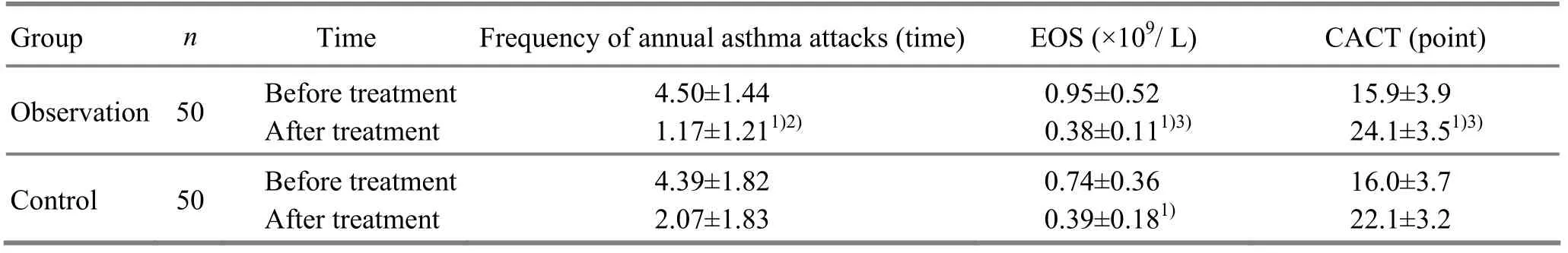
Table 4. Between-group comparison on frequency of annual asthma attacks, EOS and CACT changes
Note: Intra-group comparison between before and after treatment, 1) P<0.01; inter-group comparison after treatment, 2) P<0.01, 3) P<0.05
?
4 Discussion
Chronic cough is one of the most common respiratory tract diseases in childhood. Yang SL et al described pulse conditions and causative factors of cough[4]. Cough is a common chief complaint of numerous diseases. Chronic cough in children can be caused by multiple factors. In addition to chronic rhinitis, chronic bronchitis, cough following upper respiratory tract infection, cough-variant asthma and gastroesophageal reflux (GER), other conditions may include atopic cough, episodic respiratory symptoms without asthma and eosinophilic bronchitis.
Chronic airway inflammation can lead to hyperreactivity; the inflammation persists even during remission. Left untreated, many children with recurrent or persistent may eventually develop adult asthma. EOS infiltration in airway inflammation is pathophysiologically distinctive from other inflammations and known as an indicative marker of asthma inflammation[5]. FEV1is considered the best index for assessment of airway obstruction severity. PEF is a key index for airway resistance. Considering different PEF values from different peak expiratory flow meters, we’ve adopted % predicted value (measured PEF value/previous self-measured optimal PEF value). As a simple way to evaluate the lung function, the CACT is easy to operate and highly reliable.
In traditional Chinese medicine, recurrent respiratory tract inflection occurs as a result of fierce struggle between healthy qi and pathogenic factors. Point application using Chinese herbal medicine has been extensively used in the treatment of respiratory system diseases[6-10]. Tiantu (CV 22) is located in the depression at the center of suprasternal notch;stimulating this point can relieve qi stagnation, alleviate cough and resolve phlegm. Dazhui (GV 14) is a crossing point between the Governor Vessel and three yang meridians; stimulating this point can resolve phlegm and stasis, regulate meridian qi, activate yang qi of the lung and spleen and strengthen lung and Wei-defensive qi[11]. In addition, pungent, fragrant and phlegm-resolving herbs were combined to further consolidate the effect of warming yang, activating qi and boosting the immune system. The study has suggested that conventional Western medication plus point application using Chinese herbal medicine works well for chronic cough in children. It can significantly reduce asthma episodes, improve EOS, FEV1, PEF and CACT scores and benefit the immune function. This can further promote healthy maturity of immune organs, reduce respiratory tract infection and airway hyper-reactivity and thus prevent and treat asthma. This easy-tooperate, safe and low-cost method causes few or no side effects and deserves more extensive use in the future.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by Xu’s Pediatric Clinical Experience Inheritance Base (No. ZYSNXD-CC-HPGCJD-005); Emerging Frontier Technology Joint Research Program of Shanghai Municipal Hospitals (No. SHDC12012410); Domestic Visiting Scholar Program for Young Teachers at Shanghai Colleges and Universities; Tang Wei-yong Work Room of Shanghai Three-year Action Plan of Traditional Chinese Medicine (No. ZYSNXD-CC-MZY001); Cheng Jia-zheng Work Room of Three-year Action Plan of Traditional Chinese Medicine (No. ZYSNXD-CC-MZY002); and the Third Group Construction Project of Clinical Advantages Specialized Subject of Traditional Chinese Medicine in Shanghai (No. ZYSNXD-YL-YSZK006).
Statement of Informed Consent
Informed consent was obtained from all individual participants’ parents included in this study.
[1] Task force on respiratory disease, Chinese Society of Pediatrics, Editorial Committee of Chinese Journal of Pediatrics. Diagnosis and treatment guidelines for chronic pediatric cough (trial). Zhonghua Erke Zazhi, 2008, 46(2): 104-107.
[2] Lu Q, Wang XF, Chen HZ, Hong JG, Hu YJ, Lu YX, Ma R, Shang YX, Wang LY, Wang SM, Xu RQ. Integrated traditional Chinese and Western medicine expert consensus on diagnosis and treatment of pediatric cough. Zhongguo Shiyong Erke Zazhi, 2010, 25(6): 439-443.
[3] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 2002: 57.
[4] Yang SL, Ma FL, Nie J, Qin Q, Qiao L, Zhang JY, Zhang M. Analysis on diagnosis and treatment rules of cough in theYi Xue Zheng Zhi Ze Yao. Henan Zhongyi, 2013, 33(6): 872-873.
[5] Busse WW, Calhoun WF, Sedgwick JD. Mechanism of airway inflammation in asthma. Am Rev Respir Dis, 1993, 147(6 Pt 2): 20-24.
[6] Li LP. Clinical observation on acupoint application in preventing and treating bronchial asthma. Shanghai Zhenjiu Zazhi, 2013, 32(2): 96-97.
[7] Xu SW, Zhang BM, Zhou JM, Hu ZH, Pan CA, Wang Y, Shou Y, Yang Y, Liu MM. Clinical observation on acupuncture plus acupoint sticking for bronchial asthma in remissive state. J Acupunct Tuina Sci, 2013, 11(5): 326-330.
[8] Jiang WQ, Lou WS, Zhang YJ, Zhu FJ, Chen YB. Therapeutic observation on acupoint sticking therapy plus pricking Sifeng (EX-UE 10) for recurrent respiratory infection in children. Shanghai Zhenjiu Zazhi, 2013, 32(9): 740-741.
[9] Tong Q, Liang YP, Zheng ZT. Influence of acupoint application therapy on biochemical indexes of asthma patients in remission period. J Acupunct Tuina Sci, 2010, 8(3): 184-188.
[10] Sun J, Wang Y. Concurrent supplementation of antipathogenic qi and removal of pathogenic factors for prevention of pediatric recurrent respiratory tract infection. Zhongguo Zhongyiyao Xiandai Yuancheng Jiaoyu, 2013, 11(4): 97-98.
[11] Huang QF, Liu LG, Gu J, Wu HG. Analysis of the characteristics of moxibustion treatment for cough. Shanghai Zhenjiu Zazhi, 2010, 29(8): 483-485.
Translator:Han Chou-ping
Zhu Shengguo, chief physician.
E-mail: shuguangerke@126.com
R246.4
: A
Date:February 25, 2014
 Journal of Acupuncture and Tuina Science2014年3期
Journal of Acupuncture and Tuina Science2014年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Observation on Clinical Effects of Tuina plus Hot Compress for Infantile Diarrhea Due to Spleen-kidney Yang Deficiency
- Clinical Study on Fu’s Subcutaneous Needling with Laser for Postherpetic Neuralgia
- Therapeutic Effect Observation on Combining Electroacupuncture and Tuina for Migraine
- Therapeutic Efficacy Observation on Combined Taijiquan and Auricular Point Sticking for Perimenopausal Insomnia
- Blood Perfusion Effect of Acupuncture on Acute Facial Paralysis Observed by Laser Speckle Technique
- Therapeutic Efficacy of Tuina in Treating 48 Cases with Knee Osteoarthritis
