Effect of Relaxing Needling plus Rehabilitation Training on Post-stroke Upper Limb Dysfunction
1 The Second School of Clinical Medicine, Nanjing University of Chinese Medicine, Nanjing 210000, China
2 Department of Acupuncture, Suzhou Hospital of Traditional Chinese Medicine, Suzhou 215000, China
SPECIAL TOPIC STUDY
Effect of Relaxing Needling plus Rehabilitation Training on Post-stroke Upper Limb Dysfunction
Yao Wen-juan1, Ouyang Ba-si2
1 The Second School of Clinical Medicine, Nanjing University of Chinese Medicine, Nanjing 210000, China
2 Department of Acupuncture, Suzhou Hospital of Traditional Chinese Medicine, Suzhou 215000, China
Author: Yao Wen-juan, seven-year postgraduate candidate.
E-mail: 512847193@qq.com
Objective: To observe the effect of relaxing needling plus rehabilitation training on post-stroke upper limb dysfunction.
Methods: Sixty-eight eligible subjects with post-stoke upper limb dysfunction were randomized into 2 groups by the random number table, 34 in each group, to respectively receive relaxing needling method or ordinary needling method in addition to rehabilitation training for 2 months. Fugl-Meyer assessment of upper limb motor function, neurological defect score, and clinical efficacies were observed and compared.
Results: The two groups both showed effects. The total effective rate in the relaxing needling group was 93.8% versus 84.9% in the ordinary needling group, and the difference was statistically significant (P<0.05). The relaxing needling group was better than the ordinary needling group in improving the motor function of upper limb and neurological defect (P<0.05).
Conclusion: Relaxing needlingplus rehabilitation training can significantly improve the post-stroke motor dysfunction of upper limb, better than ordinary needling plus rehabilitation training.
Acupuncture Therapy; Needling Methods; Stroke; Complications; Upper Extremity; Rehabilitation
As one of the three leading causes of death, stroke has comparatively high incidence, mortality, and disability rates. It’s reported that 60%-80% of the survivors suffer from disability of varying degrees (majorly it’s dysfunction, of which, motor dysfunction ranks the top)[1], especially the dysfunction of limbs, which usually has a poor prognosis. During the rehabilitation, the functional training is comparatively focused on the lower limb, while the training for the upper limb is often neglected. Acupuncture therapy has its unique advantages in treating stroke, and has achieved certain progress when combined with modern rehabilitation[2-5]. We adopted relaxing needling plus rehabilitation training in treating post-stroke upper limb dysfunction, and compared it with ordinary needling plus rehabilitation training. The results are reported as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of traditional Chinese medicine (TCM)
It’s referring to theStandard for Diagnosis and Therapeutic Effect Evaluation of Strokemade by the Collaborative Group of Acute Encephalopathy of State Administration of TCM[6].
1.1.2 Diagnostic criteria of Western medicine
It’s referring to the diagnostic criteria of stroke in theKey Diagnostic Points for Cerebrovascular Diseasesby the Fourth Chinese Cerebrovascular Diseases Conference in 1995[7].
1.2 Inclusion criteria
Conforming to the above diagnostic criteria;cerebral infarction or hemorrhage of internal carotid artery, confirmed by head CT scan or MRI examination; initial attack, otherwise without neurological dysfunction caused by previous attacks;disease duration 1-12 months; age 40-75 years;Glasgow coma scale (GCS) ≥8, clear consciousness, stable vital signs; stage Ⅲ or higher according to the Brunstrom stage; informed of the study and willing to participate, and having signed the informed consent form.
1.3 Exclusion criteria
Failure to finish the present treatment protocol or having accepted the excluded treatments; with severe dysfunctions of heart, lung, liver, or kidney;exaggerated condition; disturbance of consciousness;severe aphasia or cognitive impairment that will influence the investigation; acupuncture contraindications.
1.4 Statistical analysis
The SPSS 17.0 was adopted for statistical analysis. The measurement data were expressed asand the inter-group and intra-group comparisons were processed by usingt-test; the enumeration data were managed by using Chi-square test, and the ranked data were by rank sum test.P<0.05 was considered to have a statistically significant difference.
1.5 General data
Sixty-eight eligible subjects with post-stroke upper limb dysfunction were collected from the Outpatient Department of Acupuncture, Suzhou Hospital of TCM from April 2012 to August 2013. They were randomly divided into a relaxing needling group and an ordinary needling group by the random number table, 34 in each group. There were no significant differences in comparing the general data between the two groups (P>0.05), indicating the comparability (Table 1).
During the study, 3 cases dropped out, 2 from the relaxing needling group and 1 from the ordinary needling group. The intervention procedures are shown in Figure 1.
2 Treatment Methods
2.1 Relaxing needling group
2.1.1 Rehabilitation training
The nerve facilitation techniques were majorly adopted, e.g. Bobath, Brunstrom approach, Rood, and proprioceptive neuromuscular facilitation (PNF).
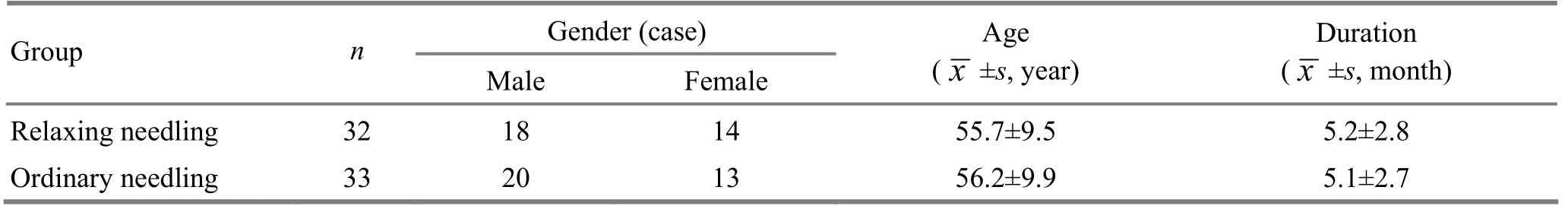
Table 1. Comparison of general data
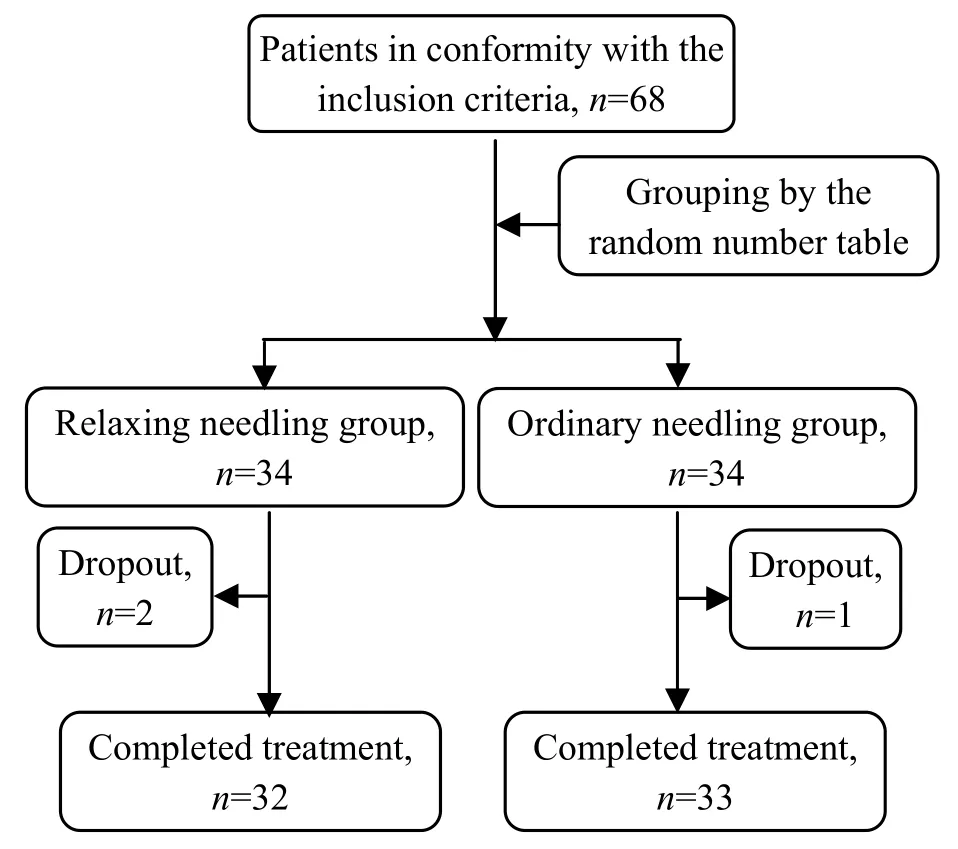
Figure 1. Intervention procedure
The training contents: Hand and foot orthotic devices to keep the wrist, elbow, and shoulder at the right functional positions; passive movements to maintain the movement ranges of the joints;autonomic movements of shoulder, elbow, and wrist;flexion of fingers, digital apposition and abduction of thumb. The training lasted 40 min each time, once every day, 6 times a week, and successive 1-month treatments as a course. Two treatment courses were observed.
2.1.2 Relaxing needling
Major points: Jianyu (LI 15), Quchi (LI 11), Hegu (LI 4), Baihui (GV 20), Fengchi (GB 20), Fengfu (GV 16), and Shenting (GV 24).
Adjunct points: Jianqian (Extra), Jianzhen (SI 9), Shousanli (LI 10), Neiguan (PC 6), Yangchi (TE 4), and Yemen (TE 2).
Operation: Each time, 3-5 points were chosen from the major point group and adjunct point group respectively. After standard sterilization, filiform needles of 0.30 mm in diameter and 40 mm in length were chosen for treatment. When needling qi was obtained, the major points were manipulated by relaxing needling method. During needle-retain, electroacupuncture was applied to 2 pairs of points, one pair from the upper limb and one pair on the head, with 5 Hz, continuous wave, moderate stimulation within the patient’s tolerance. The needles were retained for 30 min. The treatment was given once every other day, 3 times a week, 1-month treatments as a course, for 2 courses in total.
2.2 Ordinary needling
For the patients in the ordinary needling group, the ordinary needling method was used in addition to the same rehabilitation training.
Major points: Same as that in the relaxing needling group.
Adjunct points: Same as that in the relaxing needling group.
Method: The needles were of the same size as that in the relaxing needling group. When needling qi was obtained, even reinforcing-reducing manipulations were applied. The parameters of electroacupuncture adopted were also as same as that in the relaxing needling group.
3 Observation on Therapeutic Efficacy
3.1 Observation indexes
3.1.1 Evaluation of upper-limb motor function
The Fugl-Meyer assessment (FMA)[8]was used for the evaluation of upper limb motor function before and after treatment. This scale is used to estimate the reflexes of upper limb, synergic and separate movements of flexor and extensor muscles, flexion and extension of fingers, etc., 33 items in total, 0-2 score for each item. In absence of function scores 0, partial function scores 1, presence of reflex or improvement scores 2. Therefore, it will score 66 at maximum on FMA, the higher the score, the better the motor function.
3.1.2 Neurological function defect scale (NFDS)
The evaluation method brought up by the Fourth Chinese Cerebrovascular Diseases Conference was adopted[9]: the minimum score 0 standing for normal neurological function, and the maximum score 45 for severe defect.
Reduction rate of NFDS score = [(Pre-treatment NFDS score-Post-treatment NFDS score)÷ Pre-treatment NFDS score] ×100%.
3.2 Criteria of therapeutic efficacy
The therapeutic efficacy was determined by the reduction rate of NFDS score.
Recovery: The reduction rate of NFDS score was 91%-100%.
Marked improvement: The reduction rate of NFDS score was 46%-90%.
Improvement: The reduction rate of NFDS score was 18%-45%.
Invalid: The reduction rate of NFDS score was<18%.
3.3 Treatment result
3.3.1 Comparison of FMA and NFDS
After 2-month treatments, the upper limb function and NFDS were significantly improved in both groups (P<0.01). The improvements in the relaxing needling group were more significant than that in the ordinary needling group (P<0.05), (Table 2).
3.3.2 Comparison of therapeutic efficacy
According to Mann-WhitneyUtest, there was a significant difference in comparing the therapeutic efficacy between the two groups (P<0.05), and the relaxing needling group was superior to the ordinary needling group (Table 3).
Table 2. Comparison of FMA and NFDS scores (score)
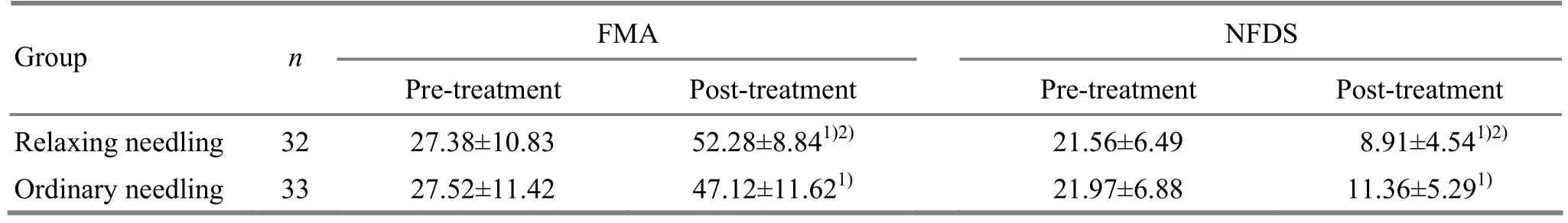
Table 2. Comparison of FMA and NFDS scores (score)
Note: Intra-group comparison, 1) P<0.01; compared with the ordinary needling group after treatment, 2) P<0.05
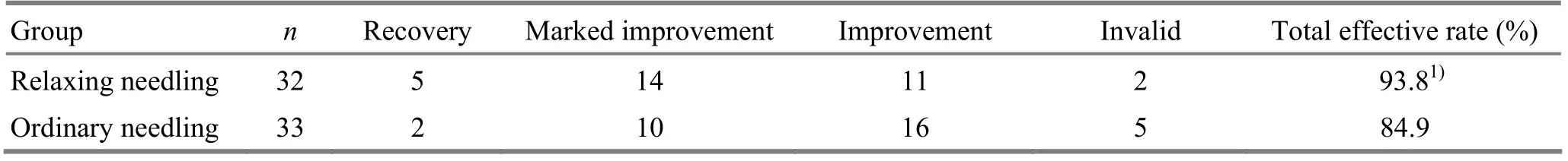
Table 3. Comparison of clinical efficacy (case)
4 Discussion
The epidemiological investigation shows that the incidence of stroke has been increasing in China. With the development of modern medicine, and the improvement of diagnosis and emergency medicine, the mortality rate of stroke has markedly decreased. However, it’s reported that 80% of the survivors suffer from various dysfunctions. As the rehabilitation science grows rapidly, the rehabilitation for stroke has become one of the focuses in this field. Although the ancient acupuncture-moxibustion therapy and modern rehabilitation science originated from different times and various countries, they relate with and complement each other, and thus are popularly used in clinic for stroke and have achieved content results[10]. It’s suggested that acupuncturemoxibustion plus rehabilitation training can reduce the damage of neurons induced by ischemia, protect and rehabilitate the neurons. It can also promote the motor function and activities of daily living (ADL), improve the therapeutic efficacy and reduce complications. The total effective rate of this comprehensive treatment approached 94.7%, better than rehabilitation and medication used independently[11].
Relaxing needling originated fromLing Shu(Spiritual Pivot). As one of the twelve needling methods, relaxing needling is used for spasms and pains of muscles and tendons. It’s to perpendicularly puncture needles nearby the spastic muscles or tendons followed by lifting-thrusting manipulations forward or backward, for unblocking the meridians and collaterals, and relieve spasticity. It’s similar to the multi-directional point-toward-point needling method in the modern time. Relaxing needling is featured by wide range of stimulation and efficient action, which allow it to promote the flow of qi and blood in meridians and collaterals, regulate the circulation of the affected limb, reduce pain, and help the recovery of limb function in a better way.
The current study shows that the limb function and neurological defect were improved significantly after 2-month treatments in both groups (P<0.01), and the improvements in the relaxing needling group were more significant (P<0.05). By adopting the randomized-controlled study method, this study was to evaluate the efficacy of relaxing needling plus rehabilitation training in treating post-stroke upper limb dysfunction, for promoting the recovery and providing a new and effective method to the rehabilitation of post-stroke upper limb dysfunction based on a systematic, organized, and scientific summary. To our knowledge, there were no similar research reported yet, hence the present study can explore a new field for stroke rehabilitation.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by Scientific Project of Jiangsu Traditional Chinese Medicine Bureau (No. LZ1150).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
[1] Wu LJ, Li SB, Chen YF. Research progress of acupuncture in treating post-stroke sequelae in recent 10 years. Zhenjiu Linchuang Zazhi, 2008, 24(5): 45-47.
[2] Ni HH, Cui X, Hu YS, Wu Y, Huang DQ, Qu PY, Wang J, Wu J, Shi JC. Observations on the efficacy of acupuncture at points Shixuan (EX-UE 11) and Xiaohai (SI 8) plus functional training in treating post-stroke hand dysfunction. Shanghai Zhenjiu Zazhi, 2012, 31(5): 9-11.
[3] Tong X, Liu DD, Wei Y, Kou JY, Yang TS, Qiao LD. Effect observation on point-through-point needling combined with tuina for post-stroke shoulder-hand syndrome. J Acupunct Tuina Sci, 2012, 10(2): 104-108.
[4] Wang XJ, Liu Q, Lin CR, Guo JK. Observations on the efficacy of combined scalp and body acupuncture in treating post-stroke upper limb spasticity. Shanghai Zhenjiu Zazhi, 2013, 32(8): 630-632.
[5] Qiu YL. Clinical observation on scalp acupuncture combined with rehabilitation training for hemiplegia after stroke. J Acupunct Tuina Sci, 2013, 11(4): 226-229.
[6] Collaborative Group of Acute Encephalopathy of State Administration of Traditional Chinese Medicine. Standard for diagnosis and therapeutic effect evaluation of stroke (trial). Beijing Zhongyiyao Daxue Xuebao, 1996, 19(1): 55-56.
[7] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379-380.
[8] Wang YL, Guo TC. Function Evaluation of Rehabilitation. Beijing: People’s Medical Publishing House, 2008: 457-460.
[9] Chinese Society of Psychiatry. Clinical neurologic deficient severity scoring standard in stroke patients. Zhonghua Shenjingke Zazhi, 1996, 29(6): 381-383.
[10] Tang Q, Zhang HM, Wang Y, Li J. Progress in the study on treatment of cerebral apoplexy with acupuncture combined with rehabilitation method. Zhenci Yanjiu, 2002, 27(4): 302-307.
[11] Tang Q. Combination of scalp cluster acupuncture and rehabilitation. Zhongguo Kangfu Lilun Yu Shijian, 2011, 17(4): 301-303.
Translator:Hong Jue
R246.6
: A
Date:March 5, 2014
 Journal of Acupuncture and Tuina Science2014年3期
Journal of Acupuncture and Tuina Science2014年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Observation on Clinical Effects of Tuina plus Hot Compress for Infantile Diarrhea Due to Spleen-kidney Yang Deficiency
- Clinical Study on Point Application Using Chinese Herbal Medicine for Pediatric Chronic Cough
- Therapeutic Effect Observation on Combining Electroacupuncture and Tuina for Migraine
- Therapeutic Efficacy Observation on Combined Taijiquan and Auricular Point Sticking for Perimenopausal Insomnia
- Clinical Study on Fu’s Subcutaneous Needling with Laser for Postherpetic Neuralgia
- Therapeutic Efficacy of Tuina in Treating 48 Cases with Knee Osteoarthritis
