Clinical Study on Acupuncture plus Medication for Chronic Atrophic Gastritis Due to Spleen-stomach Deficiency
Zhang Rong1, Wu Yao-chi, Sun Yi-jun
1 Jinyang Community Health Service Center of Pudong New District, Shanghai 200136, China
2 Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Shanghai 200233, China
SPECIAL TOPIC STUDY
Clinical Study on Acupuncture plus Medication for Chronic Atrophic Gastritis Due to Spleen-stomach Deficiency
Zhang Rong1, Wu Yao-chi2, Sun Yi-jun2
1 Jinyang Community Health Service Center of Pudong New District, Shanghai 200136, China
2 Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Shanghai 200233, China
Author: Zhang Rong, associate chief physician
Objective: To observe the clinical efficacy of combining acupuncture and medication in treating chronic atrophic gastritis (CAG) due to spleen-stomach deficiency.
Methods: Totally 176 patients with CAG were randomized into two groups by the random number table. The 91 subjects in the treatment group were intervened by acupuncture and oral Chinese patent medication; the other 85 subjects were by oral Chinese patent medication alone. The clinical efficacies were compared at the end of intervention.
Results: After a treatment course, the total effective rate was 87.9% in the treatment group versus 75.3% in the control group; according to the gastroscopy and pathological biopsy examinations, the total effective rate was 85.7% in the treatment group versus 74.1% in the control group. There were significant differences in comparing the clinical efficacy, gastroscopy and pathological examinations between the two groups (P<0.05).
Conclusion: Combining acupuncture and medication can produce a better therapeutic efficacy than medication alone in treating CAG due to spleen-stomach deficiency.
Acupuncture Medication Combined; Acupuncture Therapy; Gastritis, Atrophic; Spleen-stomach Weakness; Epigastric Pain
Atrophic gastritis is a common type of chronic gastritis, manifested as fullness in stomach, accompanied by loss of appetite, distension after meals, belching, diarrhea, and even pain and a burning sensation in stomach, lassitude, anemia, and loss of weight[1]. It falls under the scope of stomachache in traditional Chinese medicine. If poorly controlled, it may lead to gastric ulcer or cancer[2]. We have adopted acupuncture plus medication in treating chronic atrophic gastritis (CAG) due to spleenstomach deficiency, and the report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
It referred to the diagnostic criteria of CAG from theGuiding Principles for Clinical Study of New Chinese Medicines[3]and the diagnostic criteria of stomachache due to cold deficiency in spleen and stomach from theShanghai Diagnostic and Therapeutic Guidelines of Traditional Chinese Medicine[4].
Pain in stomach area, with fullness or distension, belching, acid regurgitation, gastric upset, nausea and vomiting; the flare often related to emotional disturbance, improper diet, fatigue, or contracting cold; by barium X-ray examination, gastroscopy and biopsy, mucosal inflammation or ulcer can be found in stomach or duodenum; the pain was severer on empty stomach but relieved by taking food, heat and pressing, with water brash, lassitude, cold extremities, and diarrhea. The tongue was pale and pulse was deep and thin.
1.2 Inclusion criteria
Conforming to the above diagnostic criteria; the diagnosis was confirmed by examinations within a month before the study started; age ranged 35-65 years old; informed of the study and having signed the informed consent form.
1.3 Exclusion criteria
Complications such as peptic ulcer, severe atypical hyperplasia of gastric mucosa or malignant degeneration; severe diseases of heart, brain, liver, kidney, or hematopoietic system, or psychosis; pregnant women or those who were ready to be pregnant or those in lactation period; allergic constitution or those who were sensitive to multiple drugs.
1.4 Statistical method
The SPSS 19.0 version statistical software was used for data analysis. The measurement data were expressed by mean ± standard deviationThe intra-group comparisons were conducted by using One-way ANOVA, while the inter-group paired comparisons were by the least significant difference (LSD) test and Dunnettt-test.P<0.05 indicated a statistical significance.
1.5 General data
Totally 176 were included from the outpatient. By grading of the gastric mucosa according to gastroscopy, there were 97 of mild degree (manifested as red and white, majorly white, vascular network visible, topical lesions); 73 of moderate degree (manifested as red and white, majorly white, vascular network is obvious, diffuse lesions, flattened and shallower duplicatures; type B atrophy ranging from the antrum to the angle of stomach); 6 of severe degree (besides the above manifestations, granulated mucosa or node-like hyperplasia also present; type-B atrophy involving the middle and upper part of the stomach)[5]. The 176 subjects were divided into a treatment group of 91 cases and a control group of 85 cases by the random number table. There were no significant differences in comparing the gender, age, disease duration and severity between the two groups (P>0.05), indicating the comparability (Table 1).

Table 1. Comparison of general data
2 Treatment Methods
2.1 Treatment group
2.1.1 Chinese patent medication
The patent Chinese medicationXiang Sha Liu Jun Zipill was selected, 6 g each time, twice a day, after dinner, taken with warm water, 2 months as a treatment course.
2.1.2 Acupuncture
Acupoints: Zhongwan (CV 12) and bilateral Zusanli (ST 36).
Operation: After standard sterilization of the skin, needles were inserted perpendicularly by approximately 1.2 cun. TheYang Zhong Yin Yin(yin hidden in yang) manipulation was performed when qi sensation was obtained: the needle was inserted by half depth (about 0.6 cun) first, followed by strong and quick thrusting plus gentle and slow lifting of the needle. The manipulation was repeated 9 times (a yang number) till a hot sensation was produced beneath the needle. Afterwards, the needle was inserted deeper till the required depth (1.2 cun), followed by strong and quick lifting plus gentle and slow thrusting of the needle; the manipulation was repeated 6 times (a yin number) till cool sensation was produced. Then, the needle was withdrawn to 1/3 of the depth. The needles were retained for 20 min, and theYang Zhong Yin Yin(yin hidden in yang) manipulation was performed once every 5 min during the retaining. The treatment was given once every other day, 30 sessions as a treatment course.
2.2 Control group
The control group only took the same patent Chinese medication as ordered in the treatment group, with same usage and treatment course.
3 Therapeutic Observation
3.1 Criteria of therapeutic efficacy
It referred to the criteria of therapeutic efficacy for CAG from theGuiding Principles for Clinical Study of New Chinese Medicines[3]and the criteria of therapeutic efficacy for stomachache from theShanghai Diagnostic and Therapeutic Guidelines of Traditional Chinese Medicine[4].
3.1.1 Therapeutic criteria of gastroscopy and biopsy
Recovery: Chronic gastric mucosal inflammation was improved approaching mild degree, and the atrophic glands, metaplasia of intestinal epithelium, and the atypical hyperplasia became normalized or disappeared according to biopsy.
Marked effect: Chronic gastric mucosal inflammation was improved, and the atrophic glands, metaplasia of intestinal epithelium, and the atypical hyperplasia became normalized or reduced by 2 levels according to biopsy.
Effective: Gastric mucosal lesions were reduced by over 1/2, and the chronic inflammation was improved by over 1 degree, and the atrophic glands, metaplasia of intestinal epithelium, and the atypical hyperplasia were also improved according to biopsy.
Invalid: Failure to reach the above criteria of efficacy, or condition became deteriorated.
3.1.2 Criteria of clinical efficacy
Recovery: The symptoms and signs were gone and the gastroscopy results approached the recovery standard.
Marked effect: Major symptoms and signs were gone, and the gastroscopy results approached the standard of marked effect.
Effective: Major symptoms and signs were improved, and the gastroscopy results approached the effective standard.
Invalid: Major symptoms and signs were not improved, and the gastroscopy results failed to approach the effective standard or even showed deterioration.
3.2 Results
3.2.1 Comparison of gastroscopy and biopsy
According to the gastroscopy and biopsy results, the total effective rate was 85.7% in the treatment group versus 74.1% in the control group, and the difference was statistically significant (P<0.05), (Table 2).
3.2.2 Comparison of clinical efficacy
In comparing the clinical efficacy, after a treatment course, the total effective rate was 87.9% in the treatment group versus 75.3% in the control group, and the difference was statistically significant
(P<0.05), (Table 3).

Table 2. Comparison of gastroscopy and pathological tests (case)
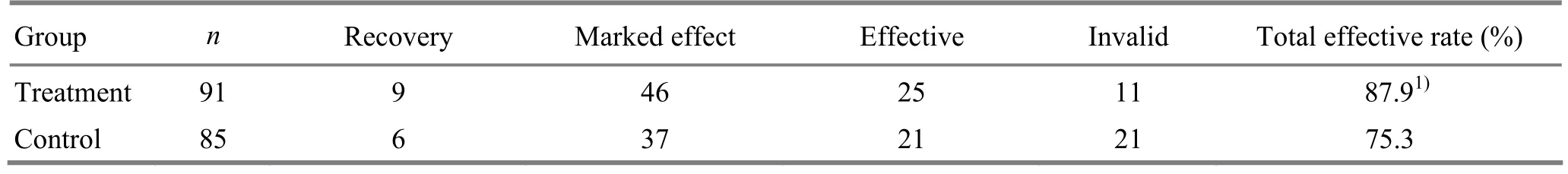
Table 3. Comparison of therapeutic efficacy (case)
4 Discussion
CAG affects stomach, majorly manifested as fullness or pain in stomach area, thus falling under the scopes of stomach fullness or stomachache in traditional Chinese medicine. Stomach fullness is usually led by chronic stomach disease leading to spleen-stomach qi deficiency and malnutrition of stomach collaterals. Spleen is the postnatal foundation, and stomach is in charge of digesting food and water. The spleen and stomach work constantly to nurture the body, but the long-term work also consumes the two organs. Therefore, deficiency of the spleen and stomach is indeed the basic factor in stomach fullness. Dysfunction of the spleen and stomach in transporting and transforming and disorder of qi activity in ascending and descending will lead to qi stagnation, phlegm and dampness, depressed heat, and blood stasis, and these pathogenic products are blocked in stomach. Therefore, CAG is deficient in the basic and excessive in the superficial.
According to syndrome differentiation of traditional Chinese medicine, CAG is classified intoliver-stomach disharmony, dampness and heat in spleen-stomach, spleen-stomach deficiency, and stomach-yin deficiency. Distention and fullness in stomach, poor appetite, lassitude, diarrhea, a pale tongue body with white coating, and deep and thin pulse are manifestations of CAG of spleen-stomach deficiency type[6].
Xiang Sha Liu Jun Zipill is composed ofRen Shen(Radix Genseng),Bai Zhu(Rhizoma Atractlodis Macrocephalae),Fu Ling(Poria),Gan Cao(Radix Glycyrrhizae),Chen Pi(Pericarpium Citri Reticulatae),Ban Xia(Rhizoma Pinelliae),Mu Xiang(Radix Aucklandiae), andSha Ren(Fructus Amomi). It works for spleen-stomach qi deficiency, phlegm, vomiting and distension, loss of appetite, loss of weight and lassitude, and swelling due to qi deficiency[7]. The indications are mostly due to spleen-stomach deficiency and dysfunction in transporting and transforming. In this formula, the sovereign and minister drugs, i.e.Ren Shen(Radix Genseng) andBai Zhu(Rhizoma Atractlodis Macrocephalae), can tonify spleen qi, nourish stomach and eliminate dampness; the assistant and guiding drugs, i.e.Fu Ling(Poria),Gan Cao(Radix Glycyrrhizae), can relieve dampness and invigorate spleen, help transporting and reinforce the middle, as well as harmonize other drugs.Chen Pi(Pericarpium Citri Reticulatae) is added to descend the reverse lung-qi;Ban Xia(Rhizoma Pinelliae) is to relieve spleen dampness;Mu Xiang(Radix Aucklandiae) for unblocking qi stagnation in the triple energizers;Sha Ren(Fructus Amomi) for helping the flow of the primary qi of spleen and kidney. With the assistant drugs, the function of the sovereign drug is strengthened; under the direction of the sovereign drug, the assistant drugs can better boost the primary qi. The eight drugs together can tonify without causing stagnation and can warm without causing dryness, and thus have become a classic formula for CAG due to spleen-stomach deficiency[8].
TheYang Zhong Yin Yin(yin hidden in yang) manipulation is originally seen inJin Zhen Fu(Poem of Golden Needle)[9]. This method is composed of slow-quick, lifting-thrusting, and twisting-rotating manipulations, first tonifying and then reducing, suitable for deficiency-excess complications. Zhongwan (CV 12) is the Influential Point of Fu organs and also the Front-Mu point of the stomach; Zusanli (ST 36) is the He-Sea point of the Foot Yangming Meridian. The two points work together to tonify qi in the middle jiao, invigorate the spleen and harmonize the stomach, reinforce the healthy qi and strengthen the basic, improve qi flow and eliminate phlegm, unblock stagnation and release dampness, and release the fullness[10-15].
It’s proven that acupuncture-moxibustion therapy is effective in treating CAG due to spleen-stomach deficiency[16-21]. Undoubtedly, it provides a new idea to the external treatment for digestive diseases such as CAG.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by Jinyang Community Health Service Center of Pudong New District and Shanghai Jiao Tong University Affiliated Sixth People’s Hospital.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
[1] Wu YC, Wang CM, Fei GW. Clinical research on acupuncture treatment of atrophic gastritis by fist reinforcement and second reduction. Shanghai Zhenjiu Zazhi, 2002, 21(6): 6-7.
[2] Zhao CP.Yi Wei Hua Qidecoction in treating 45 cases of chronic atrophic gastritis. Zhongyi Yanjiu, 2009, 22(9): 28-29.
[3] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 2002: 125-129.
[4] Shanghai Municipal Health Bureau. Shanghai Diagnostic and Therapeutic Guidelines of Traditional Chinese Medicine. 2nd Edition. Shanghai: Publishing House of Shanghai University of Traditional Chinese Medicine, 2003: 18-19.
[5] Chronic atrophic gastritis (criteria of diagnosis and treatment). Hebei Zhongyi, 2009, 31(7): 1115-1116.
[6] Zhou AG. Chinese Medicine. Shanghai: Shanghai Scientific and Technical Publishers, 2012: 177-178.
[7] Huang TK, Shi C. Modern Research Classic for Chinese Herbs and Formulae. Beijing: Science Press, 1996: 1046-1047.
[8] Fan QL. Formulas of Chinese Medicine. Shanghai: Publishing House of Shanghai University of Traditional Chinese Medicine, 2002: 132-133.
[9] Zhang DQ. Dictionary of Chinese Acupuncture-moxibustion. Beijing: Press of Beijing Sport University, 1988: 433.
[10] Qiu ML. Acupuncture and Moxibustion Science. Shanghai: Shanghai Scientific and Technical Publisher, 1988: 41-127.
[11] Tong CG, Gu SZ, Yi HQ, Guo CQ, Xiang XR, Xu B. Research on the specific pathways connecting stomach and its Back-Shu and Front-Mu points by using fluorescent double labeling method. Shanghai Zhenjiu Zazhi, 2003, 22(5): 16-19.
[12] Yang B, Gao Y, Yan XK. Survey of research on acupuncture treatment of peptic ulcer. J Acupunct Tuina Sci, 2008, 6(2): 124-128.
[13] Huang QF, Qi LZ. Treatment of chronic gastritis by acupuncture: a review. J Acupunct Tuina Sci, 2005, 3(2): 7-8.
[14] Liu XN, Guo XL, Wang FC. Research review of the relationship between the Foot Yangming Meridian and stomach diseases. Shanghai Zhenjiu Zazhi, 2011, 30(4): 275-278.
[15] Liu LG, Gu J. Analysis of acupuncture treatment characteristics of epigastric pain in ancient times. J Acupunct Tuina Sci, 2005, 3(2): 4-6.
[16] He J. Clinical observations on treatment of chronic atrophic gastritis by catgut embedding at combined Back-Shu and Frong-Mu points. Shanghai Zhenjiu Zazhi, 2008, 27(12): 8-10.
[17] He S, Luo JF, Chen JF. Clinical study on chronic gastritis treated by acupuncture. J Acupunct Tuina Sci, 2011, 9(3): 179-181.
[18] Jiang WJ, Wu LY, Lu Y, Shi Z, Li J. Experimental and clinical research progress of acupuncture-moxibustion in treating chronic atrophic gastritis. Shanghai Zhenjiu Zazhi, 2013, 32(3): 229-232.
[19] Qian C, Wei K, Shi Z. Research progress of mechanism of moxibustion in treating chronic gastritis. J Acupunct Tuina Sci, 2012, 10(4): 260-264.
[20] Zhong C. Therapeutic observation on acupuncture plus acupoint sticking for chronic atrophic gastritis of spleenstomach deficiency. Shanghai Zhenjiu Zazhi, 2012, 31(6): 399-400.
[21] Ding XY. Intradermal needle therapy and its application in treating gastric diseases. J Acupunct Tuina Sci, 2012, 10(2): 120-124.
Translator: Hong Jue
Wu Yao-chi, chief physician, professor, doctoral supervisor.
E-mail: wuyaochi11238@hotmail.com
R246.1
: A
Date: March 5, 2014
 Journal of Acupuncture and Tuina Science2014年4期
Journal of Acupuncture and Tuina Science2014年4期
- Journal of Acupuncture and Tuina Science的其它文章
- Clinical Observation on Comprehensive Treatment on Cutaneous Region for Low Back Pain
- Clinical Study on Tuina Combined with Auricular Point Sticking for Cervical Radiculopathy
- Clinical Observation on Acupuncture Combined with Hyperbaric Oxygenation in Treating Patients with Cervical Spondylosis of Nerve Root Type in Acute Phase
- Tuina for Leg Length Discrepancy and Lumbosacral Pain Due to Sacroiliac Joint Subluxation
- Clinical Study on Acupoint Injection plus Acupuncture for Insomnia Due to Heart-kidney Disharmony
- Observation on Warm Needling Therapy for Third Lumbar Vertebra Transverse Process Syndrome
