Clinical Study on Acupoint Injection plus Acupuncture for Insomnia Due to Heart-kidney Disharmony
1 Branch of First People’s Hospital of Shanghai, Shanghai 200081, China
2 Shanghai First People’s Hospital, Shanghai Jiaotong University School of Medicine, Shanghai 200080, China
3 Shanghai Yangzhi Rehabilitation Hospital, Shanghai 201619, China
CLINICAL STUDY
Clinical Study on Acupoint Injection plus Acupuncture for Insomnia Due to Heart-kidney Disharmony
Zheng Qiao-ping1, Zhang Bi-meng2, Zhou Jun-mei2, Hu Qi-long3
1 Branch of First People’s Hospital of Shanghai, Shanghai 200081, China
2 Shanghai First People’s Hospital, Shanghai Jiaotong University School of Medicine, Shanghai 200080, China
3 Shanghai Yangzhi Rehabilitation Hospital, Shanghai 201619, China
Author: Zheng Qiao-ping, attending physician.
E-mail: yangyan0003@hotmail.com
Objective: To observe the clinical efficacy of acupoint injection at Neiguan (PC 6) plus acupuncture in treating insomnia due to heart-kidney disharmony.
Methods: A hundred patients with insomnia due to heart-kidney disharmony were randomized into an observation group and a control group. Fifty-three cases in the observation group were intervened by acupoint injection at Neiguan (PC 6) plus acupuncture; while 54 cases in the control group were intervened by acupuncture alone. The Pittsburgh sleep quality index (PSQI) was evaluated before and after intervention, and the therapeutic efficacies of the two groups were compared.
Results: Acupoint injection at Neiguan (PC 6) plus acupuncture produced significantly higher efficacies in improving sleep quality, shortening sleep latency, and enhancing sleep efficiency than acupuncture alone (P<0.05).
Conclusion: The two groups both can improve the condition of insomnia; acupoint injection at Neiguan (PC 6) has significant advantages, manifested by a higher therapeutic efficacy for insomnia due to heart-kidney disharmony, higher safety evaluation, efficiency, and less adverse events, thus proper for clinical application.
Point, Neiguan (PC 6); Hydro-acupuncture; Acupuncture Therapy; Non-interaction Between the Heart and Kidney; Insomnia
Insomnia refers to difficulty initiating and maintaining sleep (easy awakening or early-morning awakening with inability to return to sleep), subsequently leading to decrease of sleep duration or quality, failure to satisfy physical need, obviously affecting social function and quality of life (QOL) during the daytime. Insomnia falls under ‘sleeplessness’ in traditional Chinese medicine, which is a common mental disorder. Long-term insomnia will cause a series of mental and physical symptoms, such as depression or anxiety. A large number of clinical trials have proven the effectiveness of acupuncture-moxibustion in treating insomnia[1-5].
Based on the correlation between insomnia and the deficiency of five Zang organs, we had included insomnia patients due to disharmony between the heart and kidney and treated them with acupoint injection at Neiguan (PC 6) plus acupuncture between July 2009 and December 2012, and compared with ordinary acupuncture. The observation is reported as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of Western medicine
It’s made referring to the diagnostic criteria of insomnia in the third edition ofChinese Classification and Diagnostic Criteria of Mental Disorders(CCMD-3) by Chinese Society of Psychiatry[6]. Predominant complaint of sleeplessness, associated with other secondary symptoms including difficulty initiating sleep, difficulty maintaining sleep, dreaminess, early awakening, difficulty returning to sleep after awakenings, discomfort after awakening, fatigue or sleepiness during daytime; the above sleep difficulty occurring at least 3 nights per week, present for over 1 month; sleeplessness causing significant distress or mental symptoms, or impairment in activities or social function; the sleeplessness was independent from any physical or mental disorders.
1.1.2 Diagnostic criteria of traditional Chinese medicine
It referred to the diagnostic criteria of sleeplessness due to disharmony between the heart and kidney from theGuiding Principles for Clinical Study of New Chinese Medicines[6]. Classic symptoms of insomnia such as difficulty falling asleep, disturbed sleep, difficulty maintaining sleep, inability to return to sleep after awakening; early-morning awakening; inability to sleep during night and sleepiness during daytime; sleep duration less than 5 h, associated with dizziness and tinnitus, soreness and weakness in low back and knee joints, and feverish sensations in the palms, soles and chest, nocturnal emissions and night perspiration, red tongue body, thin and rapid pulse.
1.2 Grading criteria
The grading criteria were made according to theGuiding Principles for Clinical Study of New Chinese Medicines[6].
Mild: Interrupted sleep or unstable sleep, earlymorning awakening, yet not affecting work.
Moderate: Sleep duration less than 4 h, yet work can be maintained.
Severe: Stay awake throughout the night, and can’t work normally.
1.3 Inclusion criteria
Conforming to the above diagnostic criteria; aged between 18 and 75 years old, no gender limitation; no use of sedatives in at least a week before the study; the current disease duration ≥6 months. Pittsburgh sleep quality index (PSQI) score >7 points[7]; having signed the informed consent and guaranteed to come for treatment according to the schedule.
1.4 Exclusion criteria
Against the inclusion criteria; pregnant or breast-feeding women; insomnia secondary to pain, fever, cough, surgery, etc.; severe liver or kidney dysfunctions, or severe diseases of other systems; severe psychotic or malignant tumor; using large dose of sedatives or sleeping pills during the week ahead of the study; fear of acupuncture, unable to cooperate.
1.5 Statistical analysis
The statistical analyses were performed by using SPSS 13.0 version statistical software. Measurement data were expressed byand analyzed byt-test, while the numeration data were by Chi-square test.
1.6 General data
Totally 107 subjects were included, all from the Acupuncture Outpatient and Neurology Inpatient Departments. According to the visiting sequence, they were randomized into two groups, 53 in the observation group and 54 in the control group. During the observation, 4 subjects from the control group and 3 from the observation group failed to finish the whole study, so they were considered as dropouts. Therefore, 100 subjects were included in the final analysis, 50 from each group. The clinical process is shown in Figure 1.
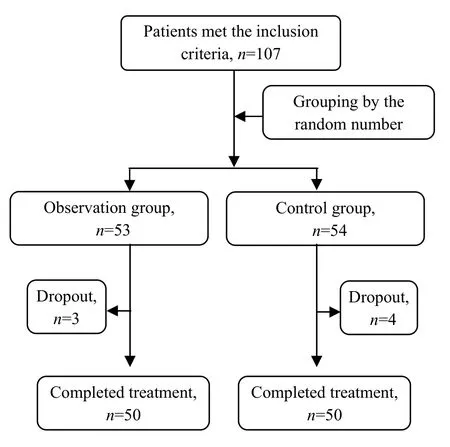
Figure 1. Clinical process of the two groups
There were no significant differences in comparing gender, age, and disease duration between the two groups (P>0.05), indicating the comparability (Table 1).

Table 1. Comparison of the general data
2 Treatment Methods
2.1 Observation group
2.1.1 Acupuncture
Acupoints: Baihui (GV 20), Shenmen (HT 7), Sanyinjiao (SP 6), Anmian (Extra), Xinshu (BL 15), and Shenshu (BL 23).
Operation: Patient took a prone position first. After sterilization with 75% alcohol, filiform needles of 0.30 mm in diameter and 40 mm in length were used for treatment. Bilateral Xinshu (BL 15) were punctured with the needles obliquely towards the spine for 1 cun. Bilateral Shenshu (BL 23) were punctured perpendicularly for 1 cun. The needles were removed when needling qi arrived, and the needling holes were pressed by dry cotton for a while. Then, the patient took a sitting position. Baihui (GV 20), Shenmen (HT 7), Sanyinjiao (SP 6) and Anmian (Extra) were punctured after standard sterilization with even reinforcing-reducing manipulation upon qi arrival. The needles were retained for 30 min, during which the needles were manipulated for 1-2 times. The needling holes were also pressed for a while when the needles were removed.
2.1.2 Acupoint injection
The patient took a sitting position. A disposable sterile 1 mL injection needle (manufactured by Shandong Weigao Group Medical Polymer Co., Ltd.) was used to draw 1 mL Vitamin B12injection. After standard sterilization, bilateral Neiguan (PC 6) were injected with the medicinal fluid when there was no withdrawal blood, 0.5 mL for each point.
The above treatments were given once every other day, 10 times as a treatment course, with a 3-day interval between two courses. The treatment results were evaluated after 2 treatment courses.
2.2 Control group
3 Therapeutic Observation
3.1 Criteria of therapeutic efficacy
It referred to the evaluation criteria from theGuiding Principles for Clinical Study of New Chinese Medicines[6].
Clinical recovery: Sleep duration was restored normal or lasted over 6 h, and sleep was sound and refreshing.
Marked effect: Sleep was significantly improved, sleep duration increased by over 3 h, sleep was deeper (sleep duration increased to 6 h, or sleep duration was less than 6 h sometimes, but subjective symptoms were improved).
Improvement: Symptoms were reduced, but sleep duration increased by less than 3 h.
Failure: Insomnia was not improved or even aggravated.
3.2 Treatment results
3.2.1 Comparison of PSQI scores before and after intervention
The 23 items of PSQI can be grouped to be 7 factors, i.e. subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. Every score was scored 0-3, and the total score should be 21 at maximum. The higher the score, the worse the sleep quality. As the subjects were forbidden from using sleep medications in this study, so only the rest 6 factors were observed.
There were no significant differences in comparing the PSQI global score and component scores between the two groups (P>0.05), indicating the comparability. After intervention, the PSQI global score and component scores dropped significantly in both groups (P<0.05), and there were significant differences between the two groups (P<0.05), indicating that the sleep improvement in the observation group were superior to that in the control group (Table 2).
3.2.2 Comparison of therapeutic efficacies
The total effective rate was 88.0% in the observation group versus 74.0% in the control group, and the difference was statistically significant
(P<0.05), (Table 3).
4 Discussion
Insomnia is an intractable problem, for not only lowering the quality of life but also inducing negative emotions. Currently, benzodiazepines are widely used to treat insomnia, but the long-term use may cause drug dependency and the change of sleep structure.
Table 2. Comparison of PSQI before and after intervention (point)

Table 2. Comparison of PSQI before and after intervention (point)
Note: Intra-group comparison, 1) P<0.05; compared with the control group after intervention, 2) P<0.05
?
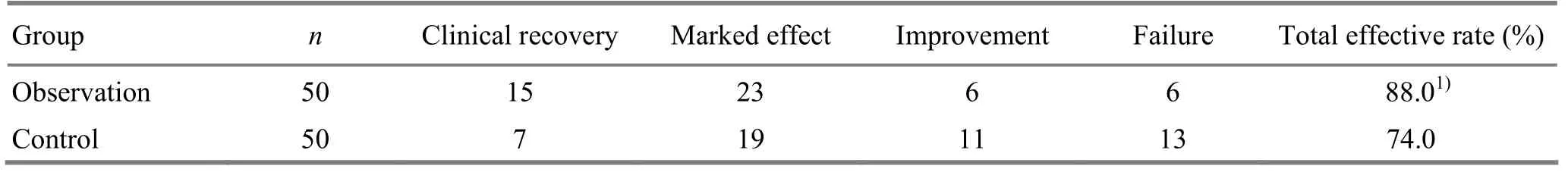
Table 3. Comparison of therapeutic efficacies (case)
Insomnia belongs to the scope of sleeplessness in traditional Chinese medicine, usually caused by deficiency of qi and blood, malnutrition of the heart and mind, or the dysfunctions of Zang-fu organs.
There is a long history to use acupuncturemoxibustion in treating insomnia, for its reliable therapeutic efficacy, relatively less adverse reactions, and high safety. When treating insomnia, the doctor has to learn the condition of yin-yang and qi and blood of the patient by using the four diagnostic methods, and to make an accurate pattern identification. Then, the doctor can treat according to the syndrome by selecting proper acupoints and treatment protocol.
The imbalance of five Zang and six Fu organs and the disharmony of qi and blood can induce insomnia. According to our clinical observation, chronic insomnia is often seen in deficiency of heart-spleen, disharmony between the heart and kidney, and qi-deficiency of the heart and gallbladder. In this study, we chose the commonest type, disharmony between heart and kidney, to treat by using acupoint injection at Neiguan (PC 6) plus acupuncture. As the Luo-Connecting point of the Pericardium Meridian and one of the eight confluent acupoints connecting the Yin Link Vessel, Neiguan (PC 6) works to open chest and regulate qi flow, harmonize stomach and calm mind. Acupoint injection was added to combine the effects of acupoint, acupuncture and medication, for strengthening the therapeutic efficacy. As the Yuan-Primary point of the Heart Meridian, Shenmen (HT 7) can activate heart qi and disperse stagnation, and strengthen the efficacy of calming heart and mind when used together with Neiguan (PC 6). Baihui (GV 20) is located at the crown of head, belonging to the Governor Vessel which goes to brain. Because brain is the house of mind, Baihui (GV 20) has become an essential point for calming mind and activating brain. Traditional Chinese medicine believes that insomnia is a disease of heart, but closely related to liver, spleen, and kidney. Sanyinjiao (SP 6) is the crossing point of the Liver, Spleen, and Kidney Meridians, acting to reinforce heart and spleen, tonify the liver and kidney, and cultivate blood and calm mind. Anmian (Extra) is an extra point, functioning to tranquilize mind. Modern medicine has proven that acupuncture at Anmian (Extra) can regulate the function of extra-intracranial vessels and nerves, and also promote the production and release of endogenous endorphin[8-9]. The transmitters involved in sleep include acetylcholine, γ-aminobutyric acid (GABA), etc. It’s discovered that GABA can inhibit the central nervous system of mammals. It’s also found that the insomnia patient has a relatively lower level of GABA in cerebrospinal fluid, while the level increases after acupoint injection at Neiguan (PC 6)[10].
The current study shows that acupoint injection at Neiguan (PC 6) plus acupuncture is effective in treating insomnia due to disharmony between heart and kidney, as it can improve the sleep quality, and it’s safe and has no adverse effects. During intervention, sleep health education, psychotherapy, and proper exercises can help shorten the treatment duration and enhance the therapeutic efficacy.
Conflict of Interest
There was no potential conflict of interest in this article.
Acknowledgments
This work was supported by Famous Traditional Chinese Medicine Doctor Construction Project of Yan Jun-bai’s Academic Experience Work Room (No. ZYSNXD-CCMZY023).
Statement of Informed Consent
All of the patients in the study signed the informed consent.
[1] Xia FX, Gan L, Ye HM. Clinical observations on the efficacy of catgut embedding at point Neiguan (PC 6) plus auricular point plaster therapy in treating insomnia. Shanghai Zhenjiu Zazhi, 2012, 31(4): 233-235.
[2] Xu TB. Clinical observation on treatment of insomnia with puncturing Back-Shu acupoints. J Acupunct Tuina Sci, 2013, 11(3): 165-168.
[3] Wang GL. Clinical observations on auricular point plaster therapy for insomnia. Shanghai Zhenjiu Zazhi, 2012, 31(10): 725-726.
[4] Fang CJ, Yang WJ, Chen YF. Research progress of acupuncture-moxibustion for insomnia: an analysis of literature in recent 5 years. J Acupunct Tuina Sci, 2013, 11(3): 181-186.
[5] Chinese Society of Psychiatry. Chinese Classification and Diagnostic Criteria of Mental Disorders. 3rd Edition. Jinan: Shandong Science & Technology Press, 2001: 118.
[6] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: People's Medical Publishing House, 1993: 186.
[7] Liu XC. Handbook of Mental Health Rating Scales. Enlarged Edition. Beijing: Chinese Mental Health Journal, 1999: 375-378.
[8] Chen L. Comparison of the curative effects of electroacupuncture on insomnia between different points. Shanghai Zhenjiu Zazhi, 2005, 24(11): 13-14.
[9] Dong LH, Li YZ, An JM, Huang LN, Zhou L. Effect on Shaanxi scalp acupuncture on sleep quality, depression and anxiety in insomnia patients. Shanghai Zhenjiu Zazhi, 2012, 31(11): 809-811.
[10] Pi M, Du SH, Zhang Y. Acupuncture for insomnia and its effect on γ-aminobutyricacid. Jiangxi Zhongyi Xueyuan Xuebao, 2000, 12(4): 160.
Translator: Hong Jue
Received Date: February 25, 2014
Zhang Bi-meng, M.D., associate chief physician.
E-mail: pjzhtiger08@aliyun.com
R246.6
: A
cts from the control group
the same acupuncture intervention as that in the observation group.
 Journal of Acupuncture and Tuina Science2014年4期
Journal of Acupuncture and Tuina Science2014年4期
- Journal of Acupuncture and Tuina Science的其它文章
- Observation on the Effect of Acupoint Injection plus Massage Therapy on Primary Dysmenorrhea
- Observation on Warm Needling Therapy for Third Lumbar Vertebra Transverse Process Syndrome
- Clinical Observation on Comprehensive Treatment on Cutaneous Region for Low Back Pain
- Tuina for Leg Length Discrepancy and Lumbosacral Pain Due to Sacroiliac Joint Subluxation
- Clinical Observation on Acupuncture Combined with Hyperbaric Oxygenation in Treating Patients with Cervical Spondylosis of Nerve Root Type in Acute Phase
- Clinical Study on Tuina Combined with Auricular Point Sticking for Cervical Radiculopathy
