Posterior reversible leukoencephalopathy syndrome presenting in a post-partum, 25-year-old-female with concomitant subarachnoid hemorrhage
Daniel M. Aronovich, Kirsten L. Ritchie, Alexander J. Scumpia
1Mount Sinai Medical Center, Department of Emergency Medicine, 4300 Alton Road, Miami Beach, FL 33140, U.S.A
2Memorial Regional Hospital, Department of Emergency Services, 3501 Johnson Street, Hollywood, FL 33021, U.S.A
Posterior reversible leukoencephalopathy syndrome presenting in a post-partum, 25-year-old-female with concomitant subarachnoid hemorrhage
Daniel M. Aronovich1, Kirsten L. Ritchie1, Alexander J. Scumpia2*
1Mount Sinai Medical Center, Department of Emergency Medicine, 4300 Alton Road, Miami Beach, FL 33140, U.S.A
2Memorial Regional Hospital, Department of Emergency Services, 3501 Johnson Street, Hollywood, FL 33021, U.S.A
Hincheyet al., first described that posterior reversible leukoencephalopathy syndrome has having a unique neuroradiographical finding of vasogenic edema and clinical symptoms including headache, altered mental status, seizure and visual disturbances in 1996. We present a rare case of posterior reversible leukoencephalopathy syndrome in a 2-week, post-partum G2P2A0 (normal spontaneous vaginal delivery at forty-weeks, without complications) 25-year-old-female with subarachnoid hemorrhage.
ARTICLE INFO
Article history:
Received 5 December 2014
Received in revised form 19 December 2014
Accepted 31 December 2014
Available online
Posterior reversible
1. Introduction
We present a rare case of posterior reversible leukoencephalopathy syndrome (PRES) in a 2-week, postpartum G2P2A0 (normal spontaneous vaginal delivery at forty-weeks, without complications) 25-year-old-female with subarachnoid hemorrhage.
2. Case presentation
The patient did not have a significant past medical/ surgical history. She presented with her husband via ambulance with a chief complaint of seizure. This newonset, convulsive episode described by her husband as upper and lower extremity “jerking motions” lasted for approximately 10 min and was aborted via 2 mg intravenous lorazepam administered by the paramedics in the field. Upon emergency department arrival, the patient’s vitals were: blood pressure with 165/117 mm Hg, HR 124 bpm, RR 22, afebrile, SpO2 99% on two liters nasal cannula, 116 mg/dL of finger stick glucose. On physical examination, the patient was hypertensive, alert and oriented×3, protecting her airway, tachycardic, incontinent of urine with complaints of a dull headache and bilateral blurry vision. No additional seizure activity was observed in the emergency department.
Initial resuscitative measures included 2-large peripheral intravenous therapys, cardiac monitoring, pulse oximetry, normal saline infusion, and labs included: complete blood count, complete metabolic profile,prothrombin time/international normalized ratio, partial thromboplastin time, urine analysis with toxicology/drug screen, chest X-ray, electrocardiogram, CT brain with consults to obstetrics and neurology. Lab work revealed a mild leukocytosis; proteinuria 4+ and CT brain (Figure 1) demonstrated a left frontal subarachnoid hemorrhage with multiple hypodensities in the frontal and parieto-occipital subcortical white matter with significant vasogenic edema suggestive of PRES. Obstetrics recommended 4gi.v.magnesium sulfate that was initiated in the emergency department.

Figure 1. CT Brain without contrast (axial view).Left frontal subarachnoid hemorrhage (thin arrow) with subtle hypodensities in the cortex and subcortical white matter of both occipital lobes (bold arrows).
Neurology recommended ani.v.labetalol drip and magnetic resonance imaging/magnetic resonance angiography/magnetic resonance venography (Figure 2) to rule out venous thrombosis/aneurysm. Additional neurosurgical consult recommended serial CT scans to monitor subarachnoid hemorrhage.
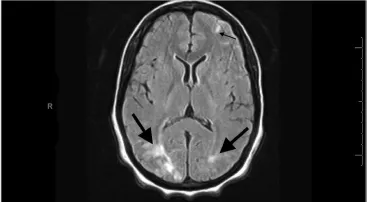
Figure 2. MRI Flair (axial view).Left frontal subarachnoid hemorrhage (thin arrow) again is demonstrated, along with classic hyperintense white matter lesions of PRES in both occipital lobes (bold arrows).
The patient was admitted to the intensive care unit and further work-up was initiated that did not demonstrate any additional findings. The patient was subsequently discharged eight days later after a full recovery.
3. Discussion
Hincheyet al, first described PRES has having a unique neuroradiographical finding of vasogenic edema and clinical symptoms including headache, altered mental status, seizure and visual disturbances in 1996[1]. Vasogenic edema is the most predominant in the posterior portions of white matter[1,2]. Acute hypertensive encephalopathy is the well-known cause, along with fluid retention, immunosuppressive drugs and renal decompensation[1-3].
Interestingly, in pregnant and immediate post-partum women, pre-eclampsia (proteinuria and hypertension) and eclampsia (pre-eclampsia and seizure) are important causes of PRES[1,3]. The case described herein, the young female developed PRES in puerperium without any indicators of pre-eclampsia-eclampsia in her pregnancy[3,4]. Furthermore, intracranial hemorrhage has been also described in the setting of PRES, with a prevalence of 19.4%[2]. This case demonstrates a rare case of PRES with subarachnoid hemorrhage in a 25-yearold, post-partum female. Prompt emergency department diagnosis with appropriate and immediate consultations is paramount for optimum patient outcome.
Conflict of interest statement
The authors report no conflict of interest.
[1] Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med 1996; 334: 494-500.
[2] Sharma A, Whitesell RT, Moran KJ. Imaging pattern of intracranial hemorrhage in the setting of posterior reversible encephalopathy syndrome. Neuroradiology 2010; 52: 855-863.
[3] Uwatoko T, Toyoda K, Hirai Y, Shimada T, Yasumori K, Ibayashi S, et al. Reversible posterior leukoencephalopathy syndrome in a postpartum woman without eclampsia. Intern Med 2003; 42: 1139-1143.
[4] Vaughn CJ, Delanty N. Hypertensive emergencies. Lancet 2000; 356: 411-417.
ment heading
10.1016/S2221-6189(14)60054-8
*Corresponding author: Alexander J. Scumpia, D.O., M.Sc. Emergency Medicine Attending Physician, Department of Emergency Services, Memorial Regional Hospital 3501 Johnson Street Hollywood, FL 33021, U.S.A.
Tel: 1-917-371-3796
E-mail: ascumpia@yahoo.com
Leukoencephalopathy syndrome
Post-partum G2P2AO
Subarachnoid hemorrhage
 Journal of Acute Disease2014年3期
Journal of Acute Disease2014年3期
- Journal of Acute Disease的其它文章
- Acute breast pain after intake of Curcuma comosa Roxb rhizome
- Compartment syndromes
- Evaluation of self-medication practices in acute diseases among university students in Oman
- Heart, tracheo-bronchial and thoracic spine trauma. Succesful multidisciplinary management: a challenging thoracic politrauma
- Acute brain hemorrhage in dengue
- Patients with the tako-tsubo cardiomyopathy-clinical evaluation and outcome
