Patients with the tako-tsubo cardiomyopathy-clinical evaluation and outcome
Agata Salska, Izabela Plesiewicz, Marzenna Zielinska, Krzysztof Chiżynski
Intensive Cardiac Therapy Clinic, Medical University, Sterlinga Str. 1/3, 91-425 Lodz, Poland
Patients with the tako-tsubo cardiomyopathy-clinical evaluation and outcome
Agata Salska*, Izabela Plesiewicz, Marzenna Zielinska, Krzysztof Chiżynski
Intensive Cardiac Therapy Clinic, Medical University, Sterlinga Str. 1/3, 91-425 Lodz, Poland
Objective: Tako-tsubo cardiomyopathy (TTC) or is a rare, acute, reversible cardiac dysfunction mimicking an acute coronary syndrome (ACS) and usually connected with a preceding intense physical or emotional stress trigger. This case series-observational study is to evaluate the clinical findings (including the depression and anxiety disorders) and outcome in patients with the tako-tsubo cardiomyopathy treated in our Centre, during 18 month period. Methods: From the group of 730 patients, who were admitted with the suspected acute myocardial infarct, ten patients, who fulfilled diagnostic criteria for TTC, were evaluated. For each patient we assessed: clinical characteristic, previous medical history including coronary disease risk factors and preceding stress trigger, 12-leads electrocardiography and laboratory tests. All patients underwent coronary-artery angiography, trans-thoracic echocardiography and completed the questionnaire evaluating the depression and anxiety disorders. Results: The estimated prevalence and clinical features of patients with the tako-tsubo cardiomyopathy in our Centre were similar to those in the literature, with the wide range of stress triggers. There was a statistically significant improvement in the ejection fraction during the hospitalization. Psychological tests revealed the 0.7 occurrence of depression or anxiety disorders among our patients. Conclusions: The exact pathogenesis of the tako-tsubo cardiomyopathy remains uncertain, but it is important to take it into account as a differential diagnosis in patients with the clinical features of myocardial infarct in the absence of coronary artery stenosis.
ARTICLE INFO
Article history:
Received 19 September 2014
Received in revised form 22 September 2014
Accepted 7 October 2014
Available online 20 November 2014
Acute coronary syndrome
1. Introduction
Tako-tsubo cardiomyopathy is a rare, acute, reversible cardiac dysfunction. It is connected with an intense physical or emotional stress trigger, mimicking acute coronary syndrome and is also known as “stress cardiomyopathy”,“apical ballooning syndrome” or “broken heart syndrome”. It was first described and named in Japan in 1991 by Sato and Dote[1], but it is also increasingly recognised in other countries. “Tako-tsubo” is the Japanese word for an octopus fishing trap-it describes the characteristic pattern of the left ventricular walls’ motion abnormalities observed in echocardiography. Tako-tsubo cardiomyopathy occurs in the 0.7%-2.5%[2] cases of patients hospitalized with suspected acute coronary syndrome, it mostly affects postmenopausal women. The most common symptoms are: chest pain, electrocardiographic changes suggesting ST-segments’ elevation acute coronary syndrome (STEMI), mild elevation of cardiac enzymes, reversible apical systolic left ventricular dysfunction in echocardiography and the absence of obstructive coronary disease in angiography. This study is to assess the clinical features and diagnostic findings among the patients with the tako-tsubo syndrome treated in our centre-during the period of 18 months.
2. Materials and methods
From the group of 730 patients, who were admittedto our centre during the period of 18 months, with the suspected acute myocardial infarct (STEMI or NSTEMI), we selected the group of ten patients, who fulfilled following diagnostic criteria: no significant coronary artery disease in angiography, new electrocardiographic changes (ST-segment elevation or T-wave inversion) and transient akinesis or dyskinesis of the left ventricular wall with its characteristic pattern in echocardiography.
For each patient we assessed: clinical characteristic, symptoms, previous medical history including coronary disease risk factors, 12-leads electrocardiography (ECG) performed on consecutive days of hospitalization and laboratory tests including cardiac biomarkers: troponin T (TnT) and myocardial creatine kinase (CK-MB). All patients underwent coronary artery angiography at the day of admission and trans-thoracic echocardiography twice during the hospitalization. We determined the presence of preceding stress trigger and established the occurrence of anxiety and depression in the study group using psychological tests: Depression Beck Scale and The Hospital Anxiety and Depression Scale (HADS). All patients were managed according to the treatment guidelines for an acute coronary syndrome and received aspirine, clopidogrel, cardioselective β-blocker, statin and angiotensinconvertin enzyme inhibitor during the hospitalization and as a recommendation at the discharge.
We also assessed the most important clinical data (cardiac death, recurrence of symptoms) in the two months follow-up period using the phone-call interview.
Statistic data are expressed as the arithmetic mean with standard deviation, the ejection fraction in echocardiography variability was estimated usingT-student test.
3. Results
We evaluated 10 from the total group of 730 patients who were admitted to our centre during the period of 18 months period due to acute myocardial infarct (STEMI or NSTEMI). This group of patients with the tako-tsubo cardiomyopathy states for 1.37% patients with acute coronary syndrome and 2.64% patients with ST-segment elevation infarct (379) hospitalised in our centre in the corresponding period. The study group consisted of 10 women aged from 43 to 81 years old, with a mean (62.7±11.53). The predominant first syndrome was retrosternal pressure-like pain (9 patients -0.9), one patient reported dyspnoea. The prevalence of additional diseases and the risk factors of coronary artery disease were: 0.8 for hypertension; 0.5 for hyperlipidemia; 0.1 for diabetes mellitus and 0.2 for smoking habit (Figure 1).
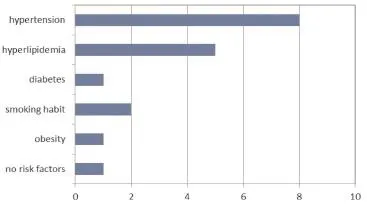
Figure 1. Atherosclerosis risk factors in patients with the tako-tsubo cardiomyopathy.
Clinical findings-the initial electrocardiogram showed ST elevation among all patients with negative T-waves in 4 (0.4) of 10 cases. During further hospitalization these changes were followed by T-wave inversion among all, pathologic Q waves in 3 (0.3) and prolongation of QT interval in 2 (0.2) of 10 cases. The initial troponin T level (TnT) was mildly elevated among all patients - the mean value was (0.46±0.52) ng/mL (normal range < 0.014 ng/mL) with a maximum rise to (0.83±0.83) ng/mL. The myocardial creatine kinase (CK-MB) at the admission was elevated (> 26 U/L) in 6 (0.6) cases. All patients had an immediate coronary angiography at the day of admission, which revealed no significant coronary artery disease. Echocardiography performed in 24 h after admission revealed characteristic heart walls’ motion abnormalities among all patients and the reduced (<55%) ejection fraction with the mean (42.0±6.7)% (with the range of 33%-54%). Follow-up echocardiogram was carried out after 3 to 7 days, it proved the reduction of abnormalities with the normal (7 cases) or improved ejection fraction - mean (58.0±7.4)% (with the range of 48%-69%). Those two results differ significantly (P<0.05).
Seven (0.7) patients reported preceding stress-in two cases it was a physical stress (exacerbation of chronic lung disease, an injury and operation of extensor muscle of the right thumb), and in six cases-an emotional stress (a family member suicide-two cases, or death due to chronic disease -two cases; an argument with husband-one case; pregnant daughters’ hospitalization-one case). One patient had both emotional and physical stress trigger. Three patients (0.3) did not report stressful situation (Table 1).
None of patients had previous history of depression, one suffered from anxiety disorders. Psychological tests (Depression Beck Scale and The Hospital Anxiety andDepression Scale - HADS) revealed the 0.7 occurrence of depression or anxiety disorders.
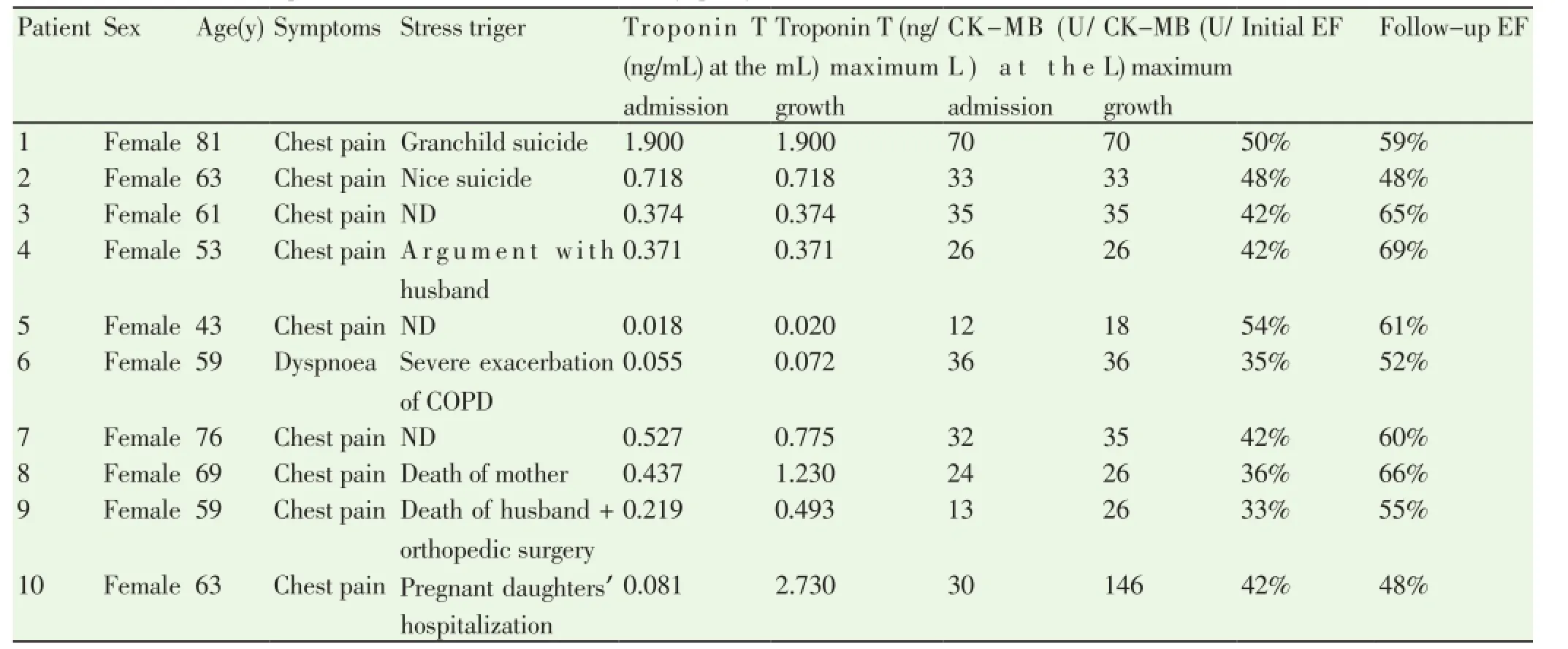
Table 1. Clinical characteristics of patients with the tako-tsubo cardiomyopathy.
None of patients presented severe complications in an acute phase of illness, such as pulmonary oedema or cardiogenic shock and there were no in-hospital or two month follow-up period death. There was one case (0.1) of recurrence of tako-tsubo syndrome after 18 months.
4. Discussion
4.1. Epidemiology
The prevalence of the tako-tsubo cardiomyopathy in different studies is estimated as 0.8%-2.5% among patients who were admitted to the hospital with the suspected acute coronary syndrome[2]. It usually affects women (86%-100%) especially postmenopausal-the mean age is from 62 to 75 years old[3]. The cause of higher incidence of TTC in this group is not explained, the gender-related differences in response to catecholamines and influence of sex hormones are possible[4,5], but the clinical symptoms and outcome do not differ depending on the gender[6], The estimated prevalence of this syndrome in our Centre was 1.37% of patients with an acute coronary syndrome and 2.64% of patients with ST-segment elevation infarct, all were women aged 43-81 years with a mean age of 62.7 years.
4.2. Aetiology
Tako-tsubo cardiomyopathy results from the severe emotional (33%-45%, 0.5 in our study) or physical (17%-22%, 0.2 in our study) stress[7] - for example death or the funeral of a family member, diagnosis of a severe illness, quarrelling, financial loss, public presentation, important meeting, acute physical disorder, surgery or medical examination, acute pain etc[3]. In about one-third (0.3 in our study) of patients no preceding stressor can be indentified, which does not exclude the TTS diagnosis[8]. Physical stress trigger is more frequent among men than women (30% vs 57%), while women more often report emotional stress trigger or no stress trigger[6]. The direct aetiology and pathogenesis of this syndrome remain unknown, the following potential mechanisms are proposed: excessive sympathetic stimulation, ischemia due to epicardial coronary arterial vasospasm, direct injury of myocytes by catecholamines, sympathetically mediated microcirculatory dysfunction[7].
In most cases concomitant diseases are present -hypertension in up to 76% (0.8 in our study), hyperlipidemia in up to 57% (0.5 in our study) and diabetes mellitus in 12% (0.1 in our study) of the patients[3].
The range of both positive and negative emotional stress triggers among patients with the tako-tsubo cardiomyopathy is very wide - it includes such situations as acute psychosis, insomnia, family member death, excessive alcohol consumption, public presentation, quarrelling, appointment or even travelling[3,9]. There is also the impact of mood disorders such as anxiety and depression investigated. Vidi[10] reported 21% and Mudd[11] -40% (significantly higher than in acute coronary syndrome group) prevalence of mood disorders in the tako-tsubo patients group-in our there was 0.7 occurrence of depression or anxiety disorders. Authorssuggest that those patients may develop higher levels of catecholamine during stress or have increased sensitivity to catecholamine stimulation.
4.3. Clinical features
Tako-tsubo cardiomyopathy in its symptoms and diagnostic findings (electrocardiography, biochemical markers) usually mimics an acute ST-elevation myocardial infarction (STEMI), but these patients have no coronary artery stenosis. The clinical profile is very similar for male and female patients[6], and the most common symptoms are - sudden onset retrosternal chest pain, dyspnoea, sometimes syncope. In the acute phase additional manifestations connected with complications such as pulmonary oedema, cardiogenic shock or arrhythmias may occur[4], but the disease is selflimiting.
4.4. Diagnostic findings.
Most of patients require an urgent coronary angiography to exclude the acute coronary syndrome - it reveals no significant coronary artery stenosis. Coronary spasm may be observed[3].
In ECG the most common finding is ST-segment elevation (<2 mm) that may be present only for several hours and is followed by T-wave inversion especially in anterior precordial leads (V1-V3) which may persist for months[3,5]. The following changes may also be present: prolongation of the QT interval, loss of R wave progression, prolonged PR interval, pathologic Q waves[7]. Electrocardiography has no predictive or differentiate value.
In echocardiography a particular shape of the left ventricle walls’ motion abnormalities are observed-apical akinesis or dyskinesis with hyperkinesis of the basal area, these abnormalities extend over the area supplied by one coronary vessel. Other echocardiographical findings are: reduced left ventricular ejection fraction and systolic dysfunction, apical ballooning with abnormal wall motion of the mid and distal left ventricle[3,7]. The normal myocardial function in echocardiography restores to normal within few weeks.
Biochemical markers such as myocardial creatine kinase and troponin T are normal or slightly elevated. Serum concentration of NT-pro-BNP is often elevated and is regarded to be an useful prognostic factor (low values at the admission are related to favourable prognosis)[5].
The MAYO Clinic considerating available data on the most important clinical features of TTC proposed the following diagnostic criteria[12]:
1. Transient hypokinesis, akinesis, or dyskinesis of the left ventricular mid segments with or without apical involvement; the regional wall motion abnormalities extend beyond a single epicardial vascular distribution; a stressful trigger is often, but not always, present.
2. Absence of obstructive coronary disease or angiographic evidence of acute plaque rupture.
3. New electrocardiographic abnormalities (either ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin.
4. Absence of: pheochromocytoma, myocarditis.
All the criteria must be fulfilled. Moreover some authors suggest that the additional features to suspect TTC are - the age of onset usually > 60 years with strong female predominance, mildly elevated creatine, myocardial wall motion abnormalities return to normal in few weeks[5,13]. The last criterion is also emphasized by the authors from MAYO Clinic as the important factor to confirm the diagnosis. The persistence of the left ventricle wall motion abnormalities after 6-8 weeks should prompt the search of another causes[12].
Exclusion criteria are: recent head trauma, intracranial bleeding, phaeochromocytoma, acute myocarditis and hypertrophic cardiomyopathy[3,4].
4.5. Therapy
The treatment method depends on clinical condition and is mostly based on symptomatic supportive management. In the early phase it is equal to the one used for patients with acute myocardial infarction including β-blockers, which should be also given in chronic phases as it may help to prevent recurrences. Complications such as pulmonary oedema, cardiogenic shock or malignant arrhythmias require additional usual treatment. The usage of catecholamines and nitrates should be careful because those substances may enlarge the hemodynamic failure. For prevention of acute thrombus formation low molecular weight heparin should be
considered[3,5].
4.6. Prognosis
Prognosis in patients with the tako-tsubo cardiomyopathy is thought to be favourable, although the long-term prognosis is unknown. The dysfunction of myocardium is reversible -patients present clinical and echocardiographical improvement in few weeks. The left ventricular ejection fraction restores to normal within (6±3) days (we recorded the normalisation of reduced ejection fraction in 7 of 10patients within 7 days), and the echocardiogram normalizes in 4 to 8 weeks[3,7]. Possible complications in early phase are: pulmonary oedema, cardiogenic shock, heart failure, ventricular thrombus, left ventricular rapture or malignant arrhythmia[3,14]. The in-hospital mortality rate in different studies is estimated as 1%-8%, none in our study[3].
Recurrence rate has been described as 2.7%-8.0% patients[5] and up to 10% in other studies[8] - in our group there was one case (0.1) of recurrence of the tako-tsubo syndrome after 18 months.
Singhet al[15] in the recent study analysed the data from 2120 TTC patients and investigated the impact of male gender, advancing age and the secondary tako-tsubo episode. The in-hospital mortality rate among patients with TTC was 4.5%, 38% of deaths were directly related to TTC complications and rest to the underlying noncardiac conditions. Male gender and the secondary TTC episode were associated with higher mortality rate. The mean age of fatal-outcome patients was higher when compared to the total population (72±7)vs(65±7) years. Those observations highlight the importance of a proper differentiation between ACS and TTC patients.
In conclusion it is important to take into account the takotsubo cardiomyopathy as a differential diagnosis in patients with clinical features of myocardial infarct (especially post-menopausal women) in the absence of coronary artery stenosis in angiography. Despite the increasing awareness of the condition, TTC is often misdiagnosed as the myocardial infarct. The differentiation of those acute diseases implies an important difference both in the early and long-term prognosis. The diagnostic outcome should include angiography and echocardiography, which needs to be repeated in order to confirm the diagnosis.
Conflict of interest statement
We declare that have no conflict of interest.
[1] Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. Myocardial stunning due to simultaneous multivessel coronary spasm: a review of 5 cases. J Cardiol 1991; 21: 203-201.
[2] Pilgrim TM, Wyss TR. Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome: A systematic review. Int J Cardiol 2008; 124: 283-292.
[3] Claudia Stöllberger, Josef Finsterer, Birke Schneider. Transient left ventricular dysfunction (tako-tsubo phenomenon): Findings and potential pathophysiological mechanisms. Can J Cardiol 2006; 22(12): 1063-1068.
[4] Bybee KA, Kara T, Prasad A, Lerman A, Barsness GW, Wright RS, et al. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med 2004; 141: 858-865.
[5] Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J 2006; 27: 2907-2908.
[6] Schneider B, Athanasiadis A, Stöllberger C, Pistner W, Schwab J, Gottwald U, et al. Gender differences in the manifestation of tako-tsubo cardiomyopathy. Int J Cardiol (2011), doi:10.1016/ j.ijcard.2011.11.027
[7] Radhakrishnan Ramaraj. Stress cardiomyopathy: aetiology and management. Postgrad Med J 2007; 83: 543-546.
[8] Sharkey SW, Lesser JR, Zenovich AG, Maron MS, Lindberg J, Longe TF, et al. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation 2005; 111: 472-479.
[9] Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblith G, et al. Neurohumoral features of myocardial tunning due to sudden emotional stress. N Engl J Med 2005; 352: 539-548.
[10] Vidi V. Clinical characteristic of tako-tsubo cardiomyopathy. Am J Cardiol 2009; 104: 578-582.
[11] Mudd JO. Patients with stress-induced (takotsubo) cardiomyopathy have an increased prevalence of mood disorders and antidepressant use compared to patients with acute myocardial infarction. J Card Fail 2007; 13: S176.
[12] Madhavan M, Prasad A. Proposed Mayo Clinic criteria for the diagnosis of Tako-Tsubo cardiomyopathy and long-term prognosis. Herz 2010; 35(4): 240-243.
[13] Kurisu S, Sato H, Kawagoe T, Ishihara M, Shimatani Y, Nishioka K, et al. Tako-tsubo-like left ventricular dysfunction with ST-segment elevation: a novel cardiac syndrome mimicking acute myocardial infarction. Am Heart J 2002; 143: 448-455.
[14] Hassid B, Azmoon S, Aronow WS, Palaniswamy C, Cohen M, Gass A. Hemodynamic support with TandemHeart in tako-tsubo cardiomyopathy - a case report. Arch Med Sci 2010; 6(6): 971-975.
[15] Singh K, Carson K, Shah R, Sawhney G, Singh B, Parsaik A, et al. Meta-analysis of clinical correlates of acute mortality in takotsubo cardiomyopathy. Am J Cardiol 2014; 113(8): 1420-1428.
ment heading
10.1016/S2221-6189(14)60052-4
*Corresponding author: Agata Salska, M.D, Intensive Cardiac Therapy Clinic, Medical University, Sterlinga Str. 1/3, 91-425 Lodz, Poland.
Fax/Tel: +48 42 6644364
E-mail: agataiwitek@poczta.fm; salska.agata@gmail.com
The study was approved by the local ethics committee.
Tako-tsubo cardiomyopathy
Stress cardiomyopathy
 Journal of Acute Disease2014年3期
Journal of Acute Disease2014年3期
- Journal of Acute Disease的其它文章
- Acute breast pain after intake of Curcuma comosa Roxb rhizome
- Compartment syndromes
- Evaluation of self-medication practices in acute diseases among university students in Oman
- Heart, tracheo-bronchial and thoracic spine trauma. Succesful multidisciplinary management: a challenging thoracic politrauma
- Posterior reversible leukoencephalopathy syndrome presenting in a post-partum, 25-year-old-female with concomitant subarachnoid hemorrhage
- Acute brain hemorrhage in dengue
