Heat-related illness in Jinshan District of Shanghai: A retrospective analysis of 70 patients
Wei-chun Mo, Xia Gao, Guo-ping Liu, Wei Wang, Jun-mei Shen, Ming-jia Xu, Jie Shen
1Department of Emergency Medicine, Jinshan Hospital, Fudan University, Shanghai 201508, China
2Center for Disease Control and Prevention, Jinshan, Shanghai 201500, China
3Intensive Care Unit, Jinshan Hospital, Fudan University, Shanghai 201508, China
Corresponding Author:Jie Shen, Email: j1999sh@163.com
Heat-related illness in Jinshan District of Shanghai: A retrospective analysis of 70 patients
Wei-chun Mo1, Xia Gao2, Guo-ping Liu1, Wei Wang1, Jun-mei Shen1, Ming-jia Xu2, Jie Shen3
1Department of Emergency Medicine, Jinshan Hospital, Fudan University, Shanghai 201508, China
2Center for Disease Control and Prevention, Jinshan, Shanghai 201500, China
3Intensive Care Unit, Jinshan Hospital, Fudan University, Shanghai 201508, China
Corresponding Author:Jie Shen, Email: j1999sh@163.com
BACKGROUND:This study aimed to investigate the epidemiological and clinical characteristics of patients with heat-related illness, and guide the prevention, diagnosis and treatment of heat-related illness.
METHODS:From June 2013 to August 2013, seventy patients with heat-related illness were treated at Jinshan Hospital of Fudan University, and their epidemiological characteristics, laboratory results, treatment and prognosis were retrospectively analyzed.
RESULTS:In the 70 patients, 18 patients suffered from heat stroke and 52 patients from nonheat stroke. When the environmnent temperature was above 35 °C, the body temperature of the patients began to increase markedly. The patients with heat stroke were significantly older than those with non-heat stroke (P<0.05). The body temperature, heart rate, blood glucose, blood lactate dehydrogenase and blood creatine kinase in the patients with heat stroke were higher than those in the patients with non-heat stroke (P<0.05). Blood lactate dehydrogenase and blood creatine kinase were positively correlated with body temperature (r=0.801).
CONCLUSION:When the environmental temperature goes above 35 °C, heat-related illness should be prevented, especially in the elderly. The body temperature, heart rate, blood glucose, blood lactate dehydrogenase and blood creatine kinase in patients with heat stroke are higher than those in patients with non-heat stroke. Blood lactate dehydrogenase and blood creatine kinase are positively correlated with body temperature, but their relationship with heat-related illness awaits further study.
Heat-related illness; Heat stroke; Blood lactate dehydrogenase; Blood creatine kinase
INTRODUCTION
The summer of 2013 was the hottest in Shanghai since 1934. The patients with heat-related illness (HRI) significantly increased in the face of the sudden hot weather. Jinshan District, which is the coastal area in southwest Shanghai, also experienced the hottest year for decades. The hot weather seriously affected the people's health, and led to sickness, even death. We retrospectively analyzed 70 patients with HRI treated at Jinshan Hospital of Fudan University of Shanghai in 2013. We studied their epidemiological and clinical characteristics of heatrelated illness and its prevention and treatment.
METHODS
Population
Of the 70 patients with HRI treated at Jinshan Hospital of Fudan University from June 2013 to August 2013, 54 patients were male. The age of the 70 patients ranged from17 to 92 years, with a mean age of 45.2±18.1 years. Eighteen patients suffered from heat stroke and 52 patients from non-heat stroke.
Methods
Medical history and physical examination were collected from the patients. Blood examination wasperformed in terms of blood routine, liver and kidney function, electrolyte, glucose, and gas analysis, and enzyme of myocardial injury. At the same time, all of the patients were cooled and rehydrated; viscera function was protected. Water and electrolyte balance was maintained, and circulatory failure, infections and other complications were prevented and treated. The patients were divided into a heat stoke group and a non-heat stroke group.
Statistical analysis
Statistical analysis was made using the software package SPSS for Windows version 16.0 (SPSS, Chicago, IL, USA). Data were presented as mean±SD, amd univariate and multivariate analyses were used for comparisons. Comparisons between different segments were analyzed using an unpaired t-test when normally distributed and using the Mann-Whitney U test when non-normally distributed. And for all tests, a P value < 0.05 was considered statistically signi fi cant.
RESULTS
Epidemiological characteristics
Seven patients with HRI were found in June, 29 patients in July, 34 patients in August. The medial environmental temperature from June to August was 34.8 °C, 37.1 °C, and 37.8 °C respectively. The medial environmental humidity was 78.2%, 81.9%, and 81.6% respectively. The average environmental wind force was 3.2, 3.1, and 3.3 respectively (Figure 1).
As the environmental temperature was increased, the onset of HRI patients was also gradually increased, especially from July 29 to July 30. The highest environmental temperature was up to 39 °C. From August 5 to August 9, the highest environmental temperature was near 40 °C, and the number of HRI patients increased signi fi cantly (Table 1).
When the environmental temperature varied from 34 °C to 35 °C, HRI developed in 4 patients respectively. When the environmental temperature rose to 36 °C to 37 °C, HRI developed in 7 and 8 patients, respectively, and showed an increasing trend. When the environmental temperature rose to 38 °C, 39 °C and 40 °C, HRI developed in 11, 15, and 21 patients respectively (Figure 2).
The characteristics of age in HRI patients
In the 70 HRI patients (54 males, mean age 45.2±18.1 years), 18 patients had heat stroke (mean age 64.1±14.9 years), and 52 patients had non-heat stroke (mean age 38.6±14.1 years) (Table 2). The non-heat stroke patientswere significantly younger than the heat stroke patients (P<0.05).
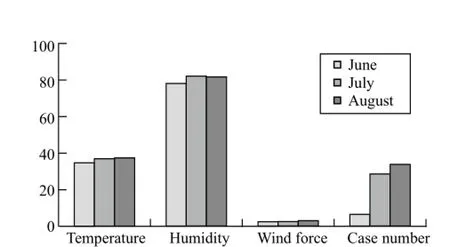
Figure 1. The environmental conditions from June to August. Temperature: environmental temperature; humidity: environmental humidity; wind force: environmental wind force.
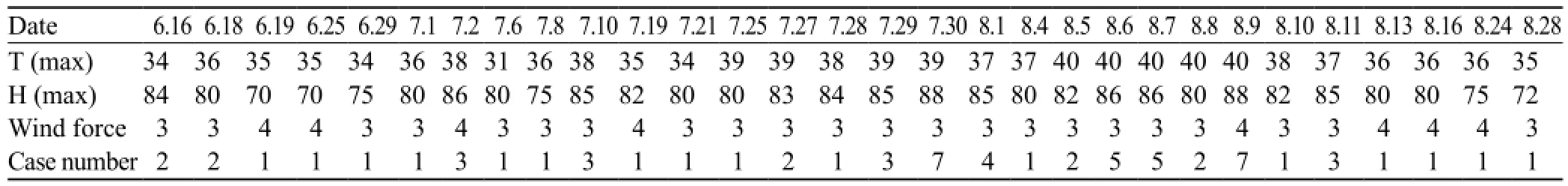
Table 1. The daily environmental conditions
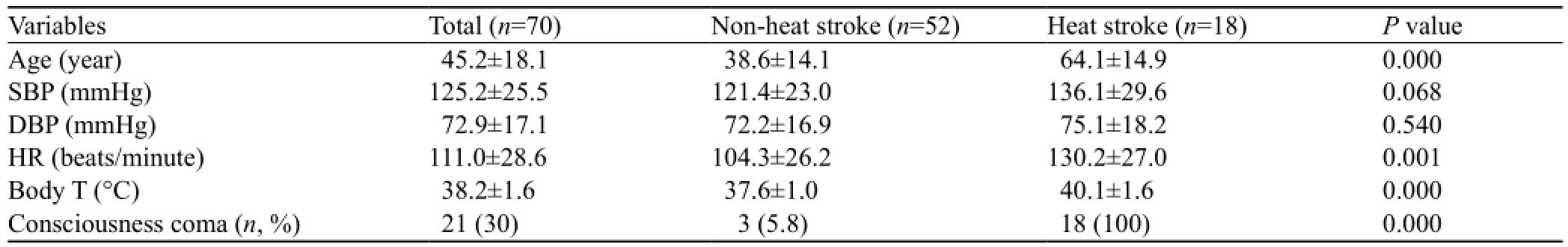
Table 2. The clinical data of HRI patients
The vital signs and laboratory characteristics of HRI patients
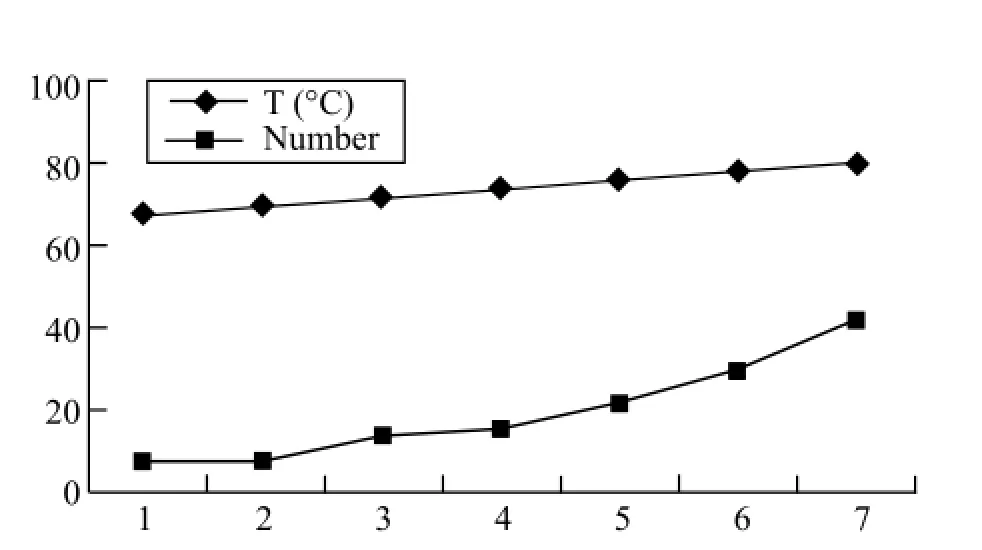
Figure 2. The environmental temperature and the onset of HRI. T: the environmental temperature; Number: the onset of HRI patients.
The heart rate of heat stroke patients was faster than that of non-heat stroke patients (P=0.001). The body temperature of heat stroke patients was significantly higher than that of non-heat stroke patients (P=0.000). The creatine kinase of heat stroke patients was higher than that of non-heat stroke patients (P=0.000). The lactate dehydrogenase of heat stroke patients was higher than that of non-heat stroke patients (P=0.002). The PLT, RBC, Hb, PCV, serum calcium and serum sodium of non-heat stroke patients were higher than those of heat stroke patients (P<0.05) (Table 3).
The correlation of lactate dehydrogenase, creatine kinase and body temperature
With the increase of body temperature, the levels of lactate dehydrogenase and creatine kinase of HRI patients increased obviously ( r1=0.801, r2=0.801, respectively, P<0.05) (Figure 3).
Treatment
Body temperature was controlled in all HRI patients.In the heat stroke patients with high fever, viscera function was protected, water and electrolyte balance maintained, and circulatory failure, shock, infection and other complications actively prevented and treated. In the 70 patients, 61 were cured and 9 died (8 patients with heat stroke and 1 patient with non-heat stroke).
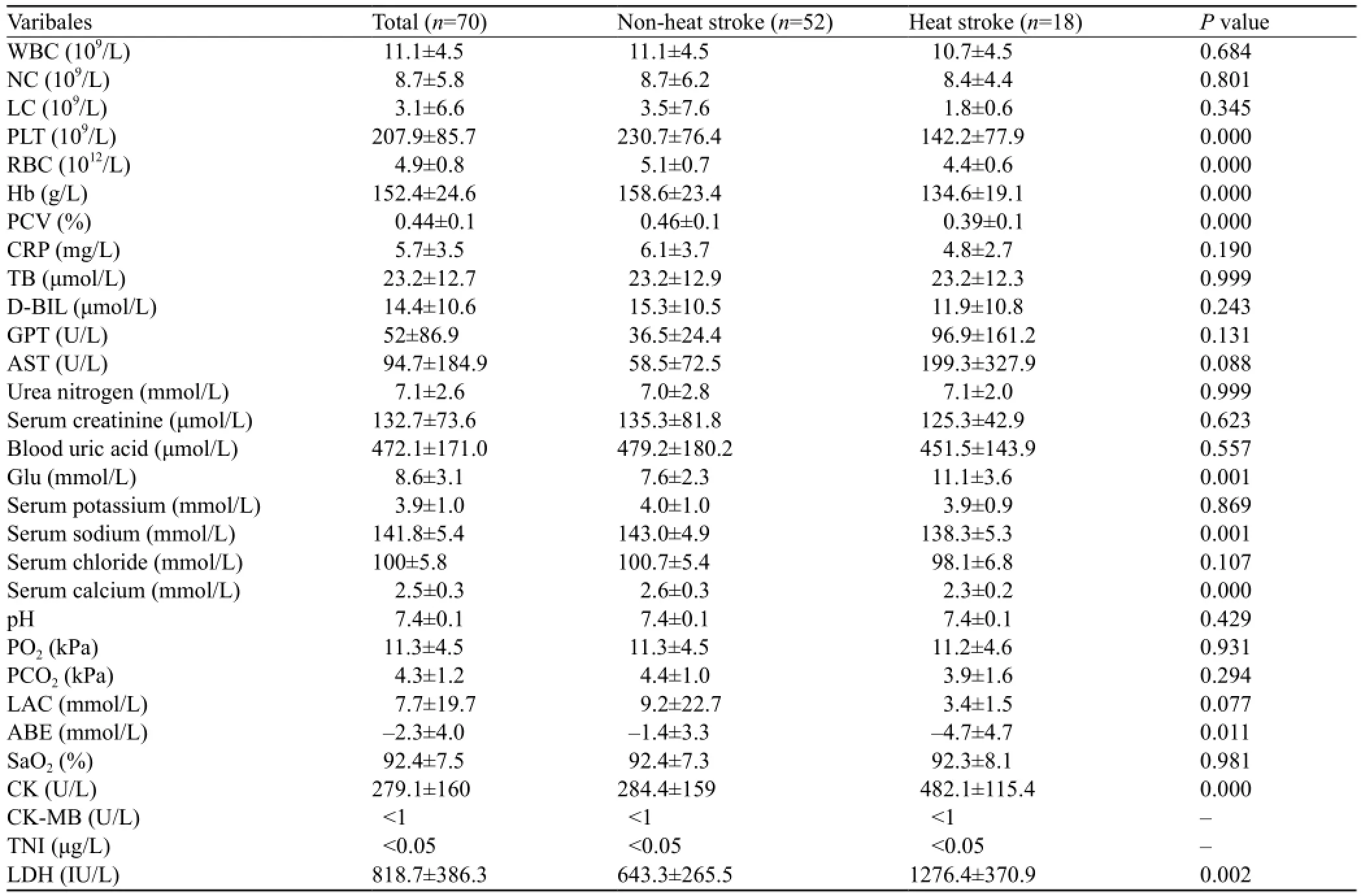
Table 3. The laboratory characteristics of patients with heat-related illness
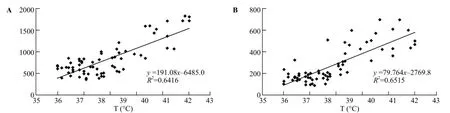
Figure 3. The correlation of body temperature with laboratory indexes. A: LDH against body T (r=0.801, P<0.05); B: CK against body T (r=0.807, P<0.05); LDH: lactate dehydrogenase; CK: creatine kinase; T: body temperature.
DISCUSSION
Heat-related illness (HRI) is an acute disease caused by the dysfunction of human body temperature regulation. There are different types of HRI, including heat rash, heat cramp, heat syncope, heat exhaustion and heat stroke. Heat stroke is a disorder of adjustment of body temperature caused by high environmental temperature. Heat excessively saves in the body, and leads to the damage of the nerve system. Heat stroke is a kind of severe and fatal heat illness. It is able to affect the function of the brain, liver, kidney, and heart ,with a high fatality rate.[1,2]
Jinshan district of Shanghai is located in the north subtropical and monsoon climate zone. Influenced by winter summer wind, this area has clear four seasons, abundant precipitation, more sunlights, and a long frostfree period. The summer begins in June, and lasts for about 3 months. This season has high temperature and heat. The period from mid-June to mid-July is the rainy season. In the cold area, the temperature is low, the weather is continuous wet and precipitated. In the warm cold area, the weather is stuffiness, sometimes sunny and sometimes rainy, but the temperature is high. Mid-July to mid-August is the hottest period in the year. The summer is the hottest reason in 2013 since 1934. In the face of the sudden heat wave, the number of HRI patients increased obviously.
In 2013, 70 HRI patients (7 patients seen in June, 29 patients in July, and 34 patients in August), were admitted to Jinshan Hospital of Fudan University. When the environmental temperature increases to 35 °C above, the temperature exceedes the human physiological limit. When the environmental temperature reaches 38 °C or above, the relative humidity approaches 50%. The body sweats a lot, evaporats abundant water, and is dehydrated, At this time, HRI may occur. The human body is easily to show the dysfunction of temperature regulation and failure of sweat gland, resulting in HRI at last.
The age of the heat stroke patients was older than that of the non-heat stroke patients (P=0.000) in this series. This finding is related to the living environment of the elderly patients[3]who have the weak ability of body temperature regulation and viscera function and the decreasing heat dissipation ability. So the elderly are more likely to develop heat stroke. Hence more attention should be paid to the improvement of the living conditions of the elderly in summer.
The body temperature was elevated and the heart rate increased in HRI patients, especially in heat stroke patients, who were more evident than non-heat stroke patients (P=0.000, P=0.001). The increased body temperature and heart rate can cause the occurrence of complications including dysfunction of the heart, brain, liver and kidney.[4]Hence it is important to control the patient's temperature. Preventing the occurrence of complications and the failure of visceral function can reduce the fatality rate.[4–6]
The values of platelet, red blood cell, hemoglobin, packed-cell volume, serum sodium, and serum calcium were higher in the non-heat stroke patients than in the heat stroke patients. This finding may be related to profuse sweating and blood concentration.[7]With regard to liver function the heat stroke patients developed failure of liver function. But there was no significantly difference between each type of HRI. The levels of blood glucose, creatine kinase and lactate dehydrogenase increased significantly in the heat stroke patients.[8]Lactate dehydrogenase as a glycolytic enzyme existedin the cytoplasm of all tissues and cells in the body. The levels of creatine kinase and lactate dehydrogenase were elevated in the HRI patients, and were higher in the heat stroke patients than in the non-heat stroke patients (P=0.000, P=0.002). The levels of creatine kinase and lactate dehydrogenase were positively correlated with body temperature: the higher the body temperature, the higher the level of creatine kinase and lactate dehydrogenase (r=0.801, r=0.807). This may be due to high fever, muscle damage, rhabdomyolysis.[8–11]The rise of blood glucose, however, is related to diabetes and the patient's stress response.[7]
Hypothermia is the most important method for the early treatment of HRI. The whole body soaked in ice water is the most effective cooling method.[12,13]
ACKNOWLEDGEMENT
We are grateful to Dr. Zhi-hua Zhang for her guidance in writing and reviewing the article.
Funding:None.
Ethical approval:Not needed.
Con fl icts of interest:The authors declare that there is no con fl ict of interest.
Contributors:Mo WC proposed the study. All authors contributed to the design and interpretation of the study, and approved the fi nal manuscript.
REFERENCES
1 Simon HB. Hyperthermia. The New Eng J of Med 1993; 329: 483–487.
2 Sithinamsuwan P, Piyavechviratana K, Kitthaweesin T, Chusri W, Orrawanhanothai P, Wongsa A, et al. Exertional heatstroke: early recognition and outcome with aggressive combined cooling-a 12-year experience. Mil Med 2009; 174: 496–502.
3 Leon LR, Helwig BG. Heat stroke: role of the systemic in fl ammatory response. J Appl Physiol 2010; 109: 1980–1988.
4 Zeller L, Novack V, Barski L, Jotkowitz A, Almog Y. Exertional heatstroke: clinical characteristics, diagnostic and therapeutic considerations. Eur J Intern Med 2011; 22: 296–299.
5 Marom T, Itskoviz D, Lavon H, Ostfeld I. Acute care for exercise-induced hyperthermia to avoid adverse outcome from exertional heat stroke. J Sport Rehabil 2011; 20: 219–227.
6 Carter R 3rd, Cheuvront SN, Williams JO, Kolka MA, Stephenson LA, Sawka MN, et al. Epidemiology of hospitalizations and deaths from heat illness in soldiers. Med Sci Sports Exerc 2005; 37: 1338–1344.
7 Garcin JM, Bronstein JA, Cremades S, Courbin P, Cointet F. Acute liver failure is frequent during heat stroke. World J Gastroenterol 2008; 14: 158–159.
8 Hashim IA. Clinical biochemistry of hyperthermia. Ann Clin Biochem 2010; 47 (Pt 6): 516–523.
9 Varghese GM, John G, Thomas K, Abraham OC, Mathai D. Predictors of multi-organ dysfunction in heatstroke. Emerg Med J 2005; 22: 185–187.
10 Capacchione JF, Muldoon SM. The relationship between exertional heat illness, exertional rhabdomyolysis, and malignant hyperthermia. Anesth Analg 2009; 109: 1065–1069.
11 Glazer JL. Management of heatstroke and heat exhaustion J. Am Fam physician 2005; 71: 2133–2140.
12 Bouchama A, Dehbi M, Chaves-Carballo E. Cooling and hemodynamic management in heatstroke: practical recommendations. Crit Care 2007; 11: R54.
13 McDermott BP, Casa DJ, Ganio MS, Lopez RM, Yeargin SW, Armstrong LE, et al. Acute whole-body cooling for exerciseinduced hyperthermia: a systematic review. J Athl Train 2009; 44: 84–93.
Received May 13, 2014
Accepted after revision October 11, 2014
World J Emerg Med 2014;5(4):286–290
10.5847/wjem.j.issn.1920–8642.2014.04.008
 World journal of emergency medicine2014年4期
World journal of emergency medicine2014年4期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- A man with a fracture from minor trauma
- A minimally invasive multiple percutaneous drainage technique for acute necrotizing pancreatitis
- Effects of mild hypothermia on the ROS and expression of caspase-3 mRNA and LC3 of hippocampus nerve cells in rats after cardiopulmonary resuscitation
- Simvastatin inhibits apoptosis of endothelial cells induced by sepsis through upregulating the expression of Bcl-2 and downregulating Bax
- A single subcutaneous dose of tramadol for mild to moderate musculoskeletal trauma in the emergency department
