International normalized ratio as a predictor of mortality in trauma patients in India
Ankur Verma, Tamorish Kole
1Department of Emergency Medicine, King Hamad University Hospital, Busaiteen, Kingdom of Bahrain, India
2Department of Emergency Medicine, Max Hospital, Saket, New Delhi 110017, India
Corresponding Author:Ankur Verma, Email address: anksv25@gmail.com
International normalized ratio as a predictor of mortality in trauma patients in India
Ankur Verma1, Tamorish Kole2
1Department of Emergency Medicine, King Hamad University Hospital, Busaiteen, Kingdom of Bahrain, India
2Department of Emergency Medicine, Max Hospital, Saket, New Delhi 110017, India
Corresponding Author:Ankur Verma, Email address: anksv25@gmail.com
BACKGROUND:Hemorrhage is the second leading cause of death in trauma patients preceded only by traumatic brain injury. But hemorrhagic shock is the most common cause of preventable death within 6 hours of admission. Traumatic coagulopathy is a hypocoagulable state that occurs in the most severely injured. International normalized ratio (INR) and its relationship with trauma mortality have not been studied speci fi cally. This study aimed to establish a predictive value of INR for trauma-related mortality.
METHODS:A total of 99 trauma patients aged 18–70 years were included in the study. Their INR was determined and patient progression was followed up till death/discharge. According to previous retrospective studies, the cutoff value for INR in our study was kept at 1.5.
RESULTS:The total mortality rate of the patients was 16.16% (16/99). The mean INR was 1.45 with a SD of 1.35. INR was deranged in a total of 14 patients (14.14%). Of these patients, 11 died (78.57%) and 3 survived. INR was deranged in 11 (68.75%) of the 16 patients who died, but 5 deaths (31.25%) had normal INR values. The sensitivity of INR was 69% (95%CI 41%–88%) and the specificity 96% (95%CI 90%–99%). The diagnostic accuracy of INR was 92% (95%CI 85%–96%). Positive predictive value and negative predictive value were 79% (95%CI 49%–95%) and 94% (95%CI 87%–98%), respectively.
CONCLUSION:Our results showed that INR is a good predictor of mortality in trauma patients.
Hemorrhage; Trauma; International normalized ratio; Mortality
INTRODUCTION
Trauma is one of the leading causes of morbidity and mortality around the world. Tramuma accidents are the 5th leading cause of death in the United States.[1]Uncontrolled bleeding and life-threatening coagulopathy are common clinically unresolved problems in trauma patients.[2]Hemorrhage is responsible for 40% of trauma deaths[3]and patients requiring massive transfusions have a mortality of over 50% in most series.[4]The existence of a distinct coagulopathic process associated with severe trauma was first recognized during the Vietnam War.[5]US military reports estimated that 15%–20% of traumatic deaths are potentially preventable and 66%–80% of these deaths occur from hemorrhage.[6]Rural civilian data indicate that approximately 10% of traumatic deaths are preventable[7]and 16% of preventable deaths are due to hemorrhage.[8]Hemorrhage is the second leading cause of death in trauma patients preceded only by traumatic brain injury. But hemorrhagic shock is the most common cause of preventable death within 6 hours of admission.[9]
Acute traumatic coagulopathy (ATC) is a hypocoagulable state that occurs in the severely injured patients.[10,11]There are multiple factors contributing to this coagulopathy induced by a combination of trauma and shock, and driven by the degree of tissue perfusion.[12]ATC can be identi fi ed 20 minutes after injury. Immediately after theinjury, hypoperfusion may cause coagulopathy as a result of increased anti-coagulation and hyper-fibrinolysis via increased protein C production and tissue plasminogen activators, and decreased concentrations of plasminogen activator inhibitors and thrombin activatable fi brinolysis inhibitors.[9,12,13]
ATC can lead to further hemorrhage, and subsequently other drivers of trauma induced coagulopathy (TIC) vis-à-vis dilution, hypothermia and acidemia are established.[13]These processes are termed as acute coagulopathy of trauma-shock (ACoTS). The presence of ATC or ACoTS in patients on admission suggests that earlier correction of coagulopathy may lead to reduced bleeding, less transfusion requirements and improved outcomes in such patients. With the need for massive transfusions, coagulopathy is one of the most accurate predictors of poor outcomes in trauma patients, civilians or military personel. Recent studies have shown that the mortality in trauma patients is associated with deranged coagulation pro fi les and reduced platelet counts.[11,14]
Coagulopathy and hemorrhage are known contributors to trauma deaths. Coagulation factors such as prothrombin time (PT), partial thromboplastin time (PTT) and platelet counts have been extensively studied, and their relationship with trauma mortality has also been studied. However, international normalized ratio (INR) and its relationship to trauma mortality have not yet been investigated specifically. With only a 15-minute turnaround time to get reports, INR was studied. This study aimed to establish a predictive value of INR for traumarelated mortality. A strong co-relationship between INR and trauma mortality may lead to early diagnosis of ATC or ACoTS, and thus early appropriate management of trauma patients is feasible.
METHODS
Study design
A pilot prospective observational study was designed with the approval from the Scientific Review Board and Ethics Committee of the hospital. Written informed consent was obtained from patients or their relatives. In addition, no patient-identifying information was collected. The study was not supported by grants from any organization or institution.
Conducted in one year from April 2012 to April 2013, the study was involved in the emergency department of an urban tertiary care center with an annual management of 64 800 patients in New Delhi and the National Capital Region (NCR).
Ninety-nine patients aged 18–70 years were enrolled at last. They were victims of high speed collisions, falls from height, gunshot wounds, stab/blunt assaults injuring visceral, solid organs, and bomb blasts.
But patients referred from other centers who had already received fluid resuscitation or blood products were excluded from the study. And those with a history of use of warfarin or vitamin K de fi ciency and a history of liver disease were also excluded. Patients with simple bruises, lacerations, contusions, concussions and fractures (except shaft femur and pelvis) were also excluded from the study.
All patients included in the study underwent STAT INR testing, for which the turn around time (TAT) was only 15 minutes at the study center. The cutoff value for INR in the study was kept at 1.5.
The data were collected by the principal investigator during his shifts. Team leaders during their particular shifts were also instructed to collect data according to the data collection sheet and the inclusion and exclusion criteria provided to them. These were then handed over to the principal investigator and the progress of the patients to their outcomes (death/discharge) was followed.
Statistical analysis
INRs of survivors and non-survivors were compared and analyzed using the commercial software STATA system version 9.0.
RESULTS
In the 99 patients, 86 (86.86%) were males and 13 (13.13%) females. In this series, 16 male patients (16.16%) died.
INR was deranged in 14 patients (14.14%),of whom 11 died (78.57%) and 3 survived (Figure 1). Of the 16 deaths, 11 (68.75%) showed deranged INR, whereas 5 (31.25%) non-survivors had normal INR. The mean INR in all the patients was 1.45±1.35, but in the non-survivorsit was as high as 3.13±2.78 and in the survivors, 1.13±0.17 (Figure 2).
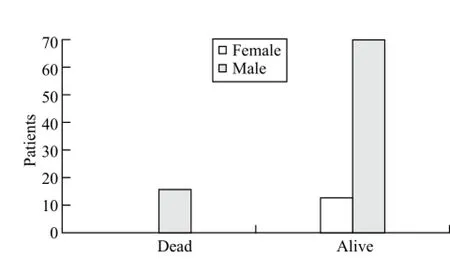
Figure 1. The male to female ratio of non-survivors and survivors.

Figure 2. The representation of INR v/s mortality.
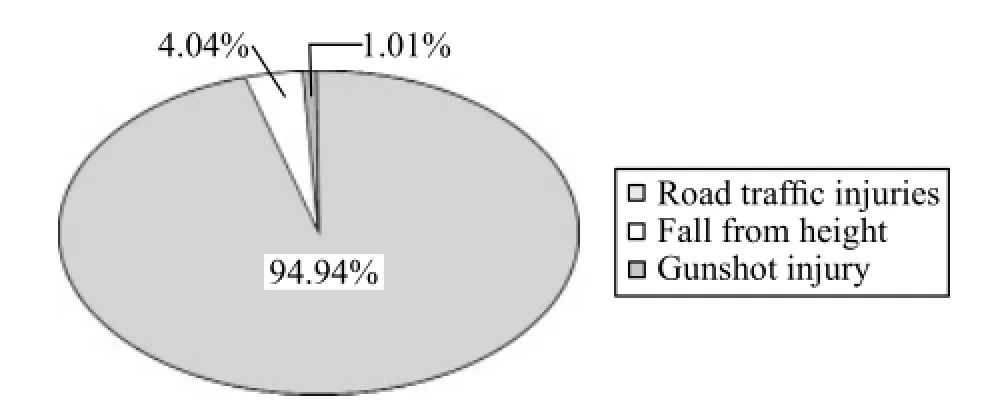
Figure 3. Causes of injury.

Figure 4. Causes of death in injured patients.
In the 99 patients, 84 (94.94%) suffered from traf fi c injuries, 4 (4.04%) from a fall from height, and 1 from a gunshot injury (Figure 3). Twelve (75%) of the 16 deaths were due to hemorrhagic shock, and 4 (25%) to traumatic brain injury (Figure 4).
In this series, the sensitivity of con fi dential test was 69% (95%CI 41%–88%) and the speci fi city was as high as 96% (95%CI 90%–99%).The diagnostic accuracy of INR as a predictor of mortality was 92% (95%CI 85%–96%).The positive predictive value and negative predictive value were 79% (95%CI 49%–95%) and 94% (95%CI 87%–98%), respectively.
DISCUSSION
Trauma, one of the leading causes of death and disability, affects all populations worldwide. In Europe almost a million people die from injury each year.[15]In the United States, trauma accounts for 42 million emergency department visits and 2 million hospital admissions each year.[16]In 2010, there were 180 811 deaths ascribed to trauma in the United States.[16]
Hemorrhage and exsanguinations were preceded only by traumatic brain injury (TBI).[17]They were involved in the derangement of prothrombin time (PT), partial thromboplastin time, INR and platelet levels in patients suspected of traumatic coagulopathy.
Recent studies[10,11]have shown that up to 25% of patients who are sent to the hospital alive after a serious injury are coagulopathic on arrival (before major resuscitation efforts begin) and that coagulopathy on arrival at trauma receiving unit is independently associated with an increased mortality.
Hess et al[14]retrospectively studied records of all patients admitted to the R. Adams Cowley Shock Trauma Centre of the University of Maryland Medical System from 2000 through 2006. They found that abnormal coagulation tests were increasingly frequent with increasing injury severity, ranging from 5% to 43% for the PT as the injury severity scores increased from 5% to over 45% and 4% to 18 % for platelet counts of less than 150X109per liter. Abnormal coagulation tests were associated with excess mortality even below conventional transfusion triggers, and this was especially true for the partial PTT.
Antifibrinolytic agents such as tranexamic acid (TXA) have been shown to reduce bleeding and mortality in patients with hemorrhagic trauma. The Cochrane review of 4 trials involving the use of antifibrinolytic agents like TXA, aprotinin and epsilon-aminocaproic acid following acute traumatic injury concluded that TXA can be safely used to reduce mortality in patients with bleeding trauma without increasing the risk of any adverse events.[18]The authors also concluded that further trials are needed to determine the effects of TXA on isolated traumatic brain injuries.
We infer that if a test can quickly predict the mortality in patients with coagulopathic bleeding,the faster use of antifibrinolytic therapy in such patients would be feasible.
The association of coagulopathies with trauma has been well established, yet it still faces criticism from various sects of medicine. The need for more evidencebased studies has been emphasized as the concepts of trauma resuscitation are undergoing changes.
India is a leading developing country with a large number of trauma deaths. Yet there has not been a major advancement in trauma research and coagulation studies in this country.
This study had its own limitations. First, the samplesize was very small, and thus this brought down the sensitivity and positive predictive value of the study. Second, the team leaders from different shifts (where principal investigator was not present) may have had different motivations for collecting data and hence a bias in selecting and reporting the patients may have occurred.
This study aimed at narrowing down on one coagulation test that had a quick TAT and that could be used to modify trauma resuscitation. The study shows that INR is indeed a good predictor of mortality in trauma patients, with a high diagnostic accuracy.
Funding:None.
Ethical approval:This study was approved by the Institutional Review Board.
Conflicts of interest:The authors have no competing interests relevant to the study.
Contributors:Verma A was the principal researcher and Kole T provided supervision and mentorship for the study.
REFERENCES
1 Xu J, Kochanek KD, Murphy SL, Tejada-Vera B. Deaths: final data for 2007. Natl Vital Stat Rep 2010; 58: 1–19.
2 Ragaller M. What's new in emergencies, trauma and shock? Coagulation is in the focus! J Emerg Trauma Shock 2010; 3: 1–3.
3 Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, et al. Epidemiology of trauma deaths: a reassessment. J Trauma 1995; 38: 185–193.
4 Malone DL, Hess JR, Fingerhaut A. Massive transfusion practices around the globe and a suggestion for common massive transfusion protocol. J Trauma 2006; 60: 591–596.
5 Innes D, Sevitt S. Coagulation and fibrinolysis in injured patients. J Clin Pathol 1964; 17: 1–13.
6 Holcomb JB, Caruso J, McMullin NR, Wade CE, Champion HR, Lawnick M, et al. Causes of death in special operations forces on the modern battlefield: 2001–2004. Ann Surg 2007; 245: 986–991.
7 Esposito TJ, Sanddal ND, Hansen JD, Reynolds S. Analysis of preventable trauma deaths and inappropriate trauma care in a rural state. J Trauma 1995; 39: 955–962.
8 Tien HC, Spencer F, Tremblay W, Rizoli SB, Brenneman FD. Preventable deaths from hemorrhage at a Level I Canadian trauma center. J Trauma 2007; 62: 142–146.
9 Spinella PC, Holcomb JB. Resuscitation and transfusion principles for traumatic hemorrhagic shock. Blood Reviews 2009; 23: 231–240.
10 Brohi K, Singh J, Coats T. Acute traumatic coagulopathy. J Trauma 2003; 54: 1127–1130.
11 Mac Leod JB, Lynn M, McKenney MG, Cohn SM, Murtha M. Early coagulopathy predicts mortality in trauma. J Trauma 2003; 55: 39–44.
12 Brohi K, Cohen MJ, Ganter MT, Schultz MJ, Levi M, Mackersie RC, et al. Acute coagulopathy of trauma: hypoperfusion induces systemic anticoagulation and hyper fi brinolysis. J Trauma 2008; 64: 1211–1217.
13 Brohi K. Trauma induced coagulopathy. J R Army Med Corps 2009; 155: 320–322.
14 Hess JR, Lindell AL, Stansbury LG, Dutton RP, Scalea TM. The prevalence of abnormal results of conventional coagulation tests on admission to a trauma center. Transfusion 2009; 49: 34–39.
15 Maegele M, Paffrath T, Bovillon B. Acute traumatic coagulopathy in severe injury – incidence, risk strati fi cation and treatment options. Dtsch Arztebl Int 2011; 108: 827–835.
16 Centers for disease control and prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query And Reporting System (WISQARS) [online]. Accessed May 8, 2013.
17 Siegel JH. The effect of associated injuries, blood loss and oxygen debt on death and disability in blunt traumatic brain injury; the need for early physiologic predictors of severity. J Neurotrauma 1995; 12: 579–590.
18 Roberts I, Shakur H, Ker K, Coats T, CRASH-2 Trial collaborators. Antifibrinolytic drugs for acute traumatic injury. Cochrane Database Syst Rev 2011; (1): CD004896.
Received December 20, 2013
Accepted after revision May 19, 2014
World J Emerg Med 2014;5(3):192–195
10.5847/ wjem.j.issn.1920–8642.2014.03.006
 World journal of emergency medicine2014年3期
World journal of emergency medicine2014年3期
- World journal of emergency medicine的其它文章
- Cardiac arrest: a case-based review
- Life-threatening complications of ascariasis in trauma patients: a review of the literature
- Instructions for Authors
- Abdominal cocoon in a young man
- Effects of aspirin on the expression of nuclear factor-κB in a rat model of acute pulmonary embolism
- Attitudes towards child restrains and seat belts usage in the learned population of Karachi, Pakistan
