Therapeutic Evaluation on Needling Method of Regulating the Conception Vessel and Calming the Mind for Perimenopausal Sleep Disorder
Sun Yuan-zheng, Liu Rui
1 The Second Affiliated Hospital of Heilongjiang University of Traditional Chinese Medicine, Harbin 150001, China
2 Heilongjiang University of Traditional Chinese Medicine, Harbin 150040, China
Therapeutic Evaluation on Needling Method of Regulating the Conception Vessel and Calming the Mind for Perimenopausal Sleep Disorder
Sun Yuan-zheng1, Liu Rui2
1 The Second Affiliated Hospital of Heilongjiang University of Traditional Chinese Medicine, Harbin 150001, China
2 Heilongjiang University of Traditional Chinese Medicine, Harbin 150040, China
Objective: To observe the clinical efficacy of needling method of regulating the Conception Vessel and calming the mind in treating sleep disorder in perimenopausal women, and to provide clinical evidence for future treatment of the disease.
Methods: Sixty eligible subjects with perimenopausal sleep disorder were enrolled and randomized into an observation group and a control group, 30 cases in each group. The observation group was intervened by needling method of regulating the Conception Vessel and calming the mind, and the control group was treated by taking Yi Kun Yin orally. Two-week treatment was considered as a treatment course. Major symptoms of traditional Chinese medicine and Pittsburgh Sleep Quality Index (PSQI) were observed, and clinical efficacies were compared.
Results: After treatment, the difference in total effective rate between the two groups was statistically significant (P<0.05); except for flaccidity of lumbar and knees, both groups achieved significant improvements in the other 5 symptoms of traditional Chinese medicine (P<0.05 or P<0.01); PSQI global score and component scores dropped in both groups, and the improvements in the observation group were markedly superior to that in the control group (P<0.05 or P<0.01).
Conclusion: The needling method of regulating the Conception Vessel and calming the mind is better than Yi Kun Yin in improving traditional Chinese medicine symptoms and sleep quality in patients with perimenopausal sleep disorders.
Acupuncture Therapy; Perimenopause Syndrome; Sleep Disorders; Climacteric Syndrome
Perimenopause refers to the one-year time from the occurrence of ovary dysfunction to menopause. During this period, due to degenerated ovary function and decreased estrogen production, women usually experience degeneration of nervous system function and mental stability, low adaptability to external environment, hypersensitivity to psychological factors and physical diseases, poor endurance, and a series of subsequent dysfunction of autonervous system and sex gland endocrine, which are termed perimenopausal syndrome. Sleep disorder is a very common symptom of perimenopausal syndrome, and it affects patient’s work and life in severe cases. We adopted needling method of regulating the Conception Vessel and calming the mind to treat 30 patients with perimenopausal sleep disorder, and it is reported as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of Western medicine
The diagnostic criteria of perimenopausal syndrome were made according to the 7th version of Gynecology[1]. Perimenopausal patients have the following clinical manifestations: irregular menstrual cycles, prolonged period, and heavy menstrual bleeding; hot flashes of neck and face, and consistent sweating of face or whole body; difficulty falling asleep, anxiety, and low mood; irritation, loss control of anger, and depression; loss of memory, defeated attention; lab test finding decreased estradiol (E2), and increased follicle stimulating hormone (FSH) and luteinizing hormone (LH). Meanwhile, FSH >10 U/L is defined as decreased ovarian reserve; FSH >40 U/L indicates ovarian failure.
Diagnostic criteria of sleep disorder were made according to the second version of International Classification of Sleep Disorders (ICSD-2)[2]. Sleep disorder presents with difficulty falling asleep or staying asleep, sleep disturbances, difficulty falling asleep again after wake-up, or even staying up all night, accompanied by nervosity, irritation, poor memory, headache, and night sweating; lumbago, joint pain, irregular menstrual cycle, prolonged menstrual period, and reduced amount of menstrual blood.
1.1.2 Diagnostic criteria of traditional Chinese medicine
Diagnostic criteria of traditional Chinese medicine were based upon the Guiding Principles for Clinical Study of New Chinese Medicines[3], and patients with liver-kidney yin deficiency were selected.
Major symptoms: Hot flashes, insomnia and dream-disturbed sleep, restlessness and irritation.
Secondary symptoms: Dizziness and tinnitus, lumbar and knee flaccidity, stuffy chest, palpitation, forgetfulness, lassitude, itchy skin, dry vagina, bitter taste, dry mouth and throat, feverish sensations in the palms and soles, frequent urination and dark urine, and dry stool.
Tongue and pulse: Red tongue body with thin coating; wiry or thin and rapid pulse.
Diagnosis is made when the above major symptoms and 2 or more items of secondary symptoms are present, with help of tongue and pulse examinations.
1.2 Inclusion criteria
In accordance with the above Chinese and Western diagnostic criteria; female aged between 45 and 60 years old; the global score of the six components of Pittsburgh Sleep Quality Index (PSQI) >6; subjects who have singed the informed consent form.
1.3 Exclusion criteria
Subjects who have bilateral ovary removed, or who have ovary or breast tumor; subjects who haven’t been recovered from an agnogenic irregular vaginal bleeding; subjects who took sex hormone drugs in the recent 3 months, or who are participating in other clinical trials; subjects with allergies; subjects in co-morbid with severe primary diseases of cardiocerebrovascular, liver, kidney, or hematopoietic systems, or psychological problems; subjects who refuse to sign informed consent form.
1.4 General data
Sixty eligible subjects were selected from the female outpatients of Acupuncture Department, the Second Affiliated Hospital of Heilongjiang University of Traditional Chinese Medicine from December 2011 to June 2012. The subjects were numbered by their visiting sequence and then divided into an observation group and a control group by random number table, 30 each. In the observation group, subjects were aged between 45 and 59 years old and their disease duration ranged from 6 to 38 months. In the control group, subjects were aged between 47 and 58 years old and their disease duration ranged from 8 to 32 months. There were no significant differences in comparing age and disease duration between the two groups (P>0.05), indicating the comparability (table 1).
Table 1. Comparison of general data ()
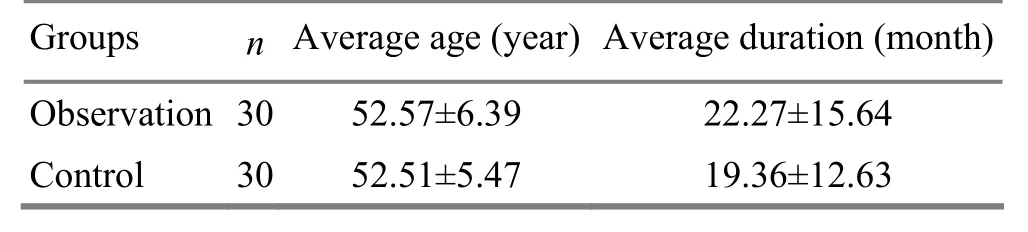
Table 1. Comparison of general data ()
Observation 3052.57±6.39 22.27±15.64 Control 3052.51±5.47 19.36±12.63
2 Treatment Methods
2.1 Observation group
Major acupoints: Zigong (EX-CA 1), Zhongji (CV 3), Guanyuan (CV 4), Qihai (CV 6), and Anmian [Extra, locates at the midpoint between Yifeng (TE 17) and Fengchi (GB 20)].
Adjunctive acupoints: Shenting (GV 24), Baihui (GV 20), and bilateral Neiguan (PC 6), Shenmen (HT 7), Sanyinjiao (SP 6), Taixi (KI 3), Taichong (LR 3), and Fengchi (GB 20).
Operation: For each treatment, the major acupoints were all selected, while the adjunctive acupoints were used alternately by selecting 10 acupoints for each time. Patient was asked to take a supine position. After standard sterilization on local areas, filiform needles of 0.35 mm in diameter and 40 mm in length were used to insert into Baihui (GV 20) and Shenting (GV 24) horizontally. The other acupoints were inserted perpendicularly. When needling sensation was obtained, even reinforcing-reducing manipulations were performed and the needles were retained for 30 min. The treatment was given once per day, a continuous 2-week treatment as a course. There was a 2-day interval between two treatment courses. It took 8 weeksto finish the whole treatment.
2.2 Control group
Subjects in the control group took Yi Kun Yin (supplied by Pharmaceutical Preparation Department of Nanjing Hospital of Traditional Chinese Medicine, Standard No. Z04000787), 10 mL per phial, 2 phials each time, twice a day, 2 weeks as a treatment course, and for 8 weeks in total. Yi Kun Yin is composed of Sheng Di (Radix Rehmanniae) 15 g, Gou Qi Zi (Fructus Lycii) 15 g, Bai Shao (Radix Paeoniae Alba) 10 g, Sheng Mu Li (Concha Ostreae) 20 g, Gou Teng (Ramulus Uncariae Cum Uncis) 10 g, He Huan Pi (Cortex Albizziae) 15 g, Huang Qi (Radix Astragali) 15 g, Fu Ling (Poria) 10 g, and Xian Ling Pi (Herba Epimedii) 10 g.
3 Observation on Therapeutic Efficacy
3.1 Observation indexes
3.1.1 Major symptoms of traditional Chinese medicine
According to the Guiding Principles for Clinical Study of New Chinese Medicines[3], the changes of symptoms of traditional Chinese medicine including hot flashes, perspiration, sleeplessness and dreaminess, restlessness and irritation, dizziness and tinnitus were recorded after treatment, and the recovery rates would be compared afterwards[4].
Recovery rate=Number of recovered subjects/Subject number in the group ×100%.
3.1.2 PSQI
The changes of PSQI global score were evaluated from the following aspects: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. An inter-group comparison would be conducted afterwards. PSQI global score ranges 0-21, and a higher score indicates a poorer sleep quality. It usually takes 5-10 min for the subject to finish the whole questionnaire.
3.1.3 Total effective rate
It was made based on the criteria of therapeutic efficacy in the Guiding Principles for Clinical Study of New Chinese Medicines[3].
Clinical recovery: The sleep duration is normal, night sleep duration >6 h, and sleep is sound and refreshing.
Marked effect: Sleep is improved, sleep duration is increased, sleep is deeper, but the total sleep duration<6 h.
Failure: Sleep is not improved or the problem worsens after treatment.
The therapeutic efficacies in the two groups were evaluated according to the above criteria, and the total effective rates were calculated and compared.
3.2 Statistical method
The PEMS 3.1 statistical software was used to deal with the data. Mean ± standard deviation (), median, and constituent ratio were generated by using a descriptive method; t-test was used for inter-group comparison of measurement data; rank-sum test was adopted for data with abnormal distribution and heterogeneity of variance; Chi-square test (or exact probability) was for inter-group comparison of numeration data; Ridit or rank-sum test was for inter-group comparison of ranked data, and the level was defined as α=0.05.
3.3 Results
3.3.1 Comparison of therapeutic efficacy
The total effective rate was 93.3% in the observation group versus 73.3% in the control group, and the difference was statistically significant according to Ridit test, indicating that the observation group has a better therapeutic efficacy than the control group (table 2).
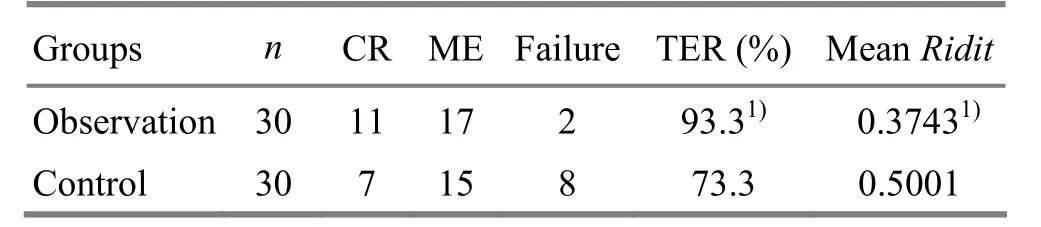
Table 2. Evaluation of therapeutic efficacy (case)
3.3.2 Comparison of major symptoms of traditional Chinese medicine
After treatment, major symptoms of traditional Chinese medicine obtained certain improvements in both groups. Except for lumbar and knee flaccidity, both groups had significant improvements in the other symptoms of traditional Chinese medicine (P<0.05 or P<0.01). It also shows that the observation group has better therapeutic effect than the control group in improving hot flashes, perspiration, sleeplessness and dreaminess, restlessness and irritation, dizziness and tinnitus (table 3).
3.3.3 Comparison of PSQI scores before and after treatment
There were no significant differences in comparing the PSQI global score and component scores between the two groups before treatment (P>0.05). After treatment, PSQI global score and component scores all dropped in both groups, and the improvements in subjective sleep quality, sleep duration, sleep disturbances and PSQI global score of the observation group were superior to those in the control group (P<0.05 or P<0.01), (table 4).
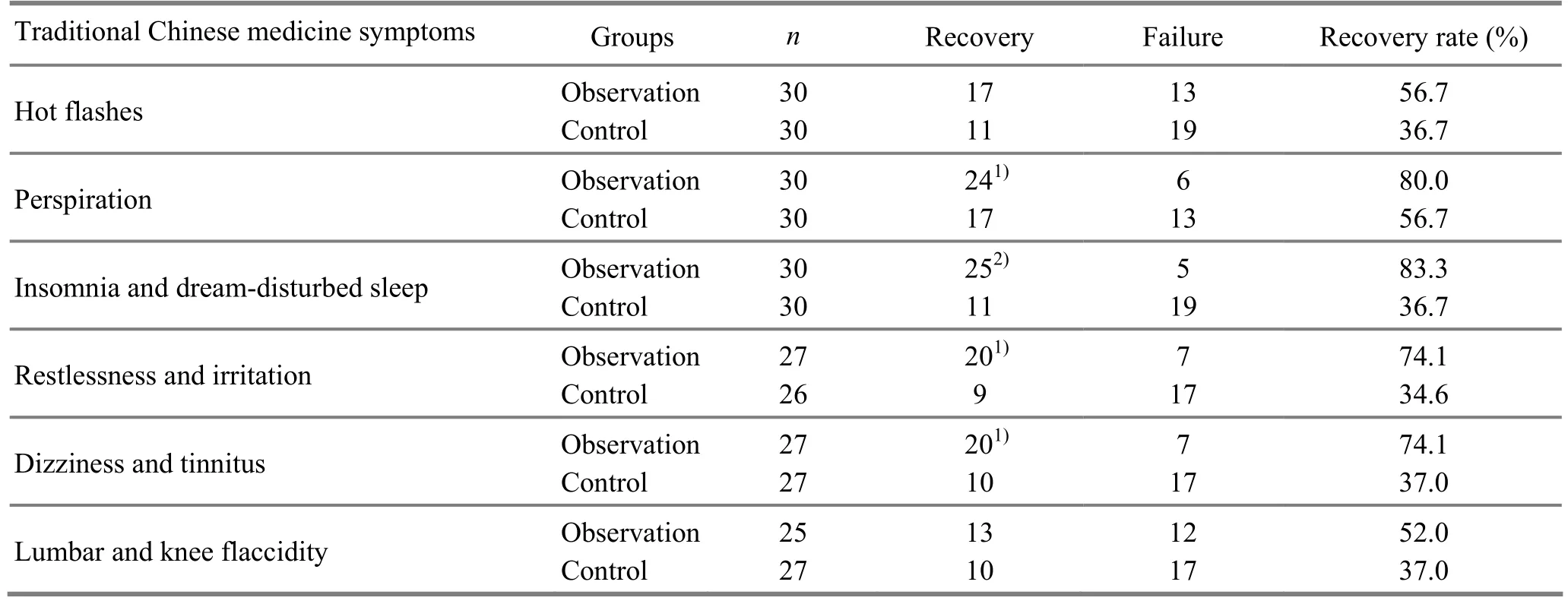
Table 3. Comparison of major symptoms of traditional Chinese medicine before and after treatment (case)
Table 4. Comparison of PSQI scores between the two groups (, score)

Table 4. Comparison of PSQI scores between the two groups (, score)
Note: Inner-group comparison with pre-treatment level, 1) P<0.05, 2) P<0.01; compared with the control group after treatment, 3) P<0.01
4 Discussion
Perimenopausal sleep disorder does not have an equivalent name in traditional Chinese medicine; but, its clinical manifestations can be found in the elaborations of symptoms around menopause and sleeplessness syndrome. Traditional Chinese medicine holds that it’s caused by kidney deficiency, insufficiency of the Thoroughfare and Conception Vessels, dysfunction of Zang-fu organs, and loss of balance between yin and yang. Well, the key point of acupuncture-moxibustion treatment is to restore the balance between yin and yang and normal physical function by regulating yin and yang and dredging meridians and collaterals. Perimenopausal sleep disorder is often diagnosed by traditional Chinese medicine with kidney yin deficiency, in which kidney is not able to produce enough fluid to go up to inhibit the heart fire, subsequently inducing restlessness, sleeplessness, and dreaminess. Zhongji (CV 3), Qihai (CV 6), and Zigong (EX-CA 1) locate on the lower abdomen, and can directly regulate the function of female reproductive system. As the crossing acupoints of Conception Vessel and the Three Yin Meridians of Foot, Zhongji (CV 3) and Guanyuan (CV 4) simultaneously adjust the function of the Conception Vessel and the Three Yin Meridians of Foot, and also act to tonify the kidney, benefit the spleen, and dredge the liver. Shenmen (HT 7) is the Yuan-Primary acupoint of the Heart Meridian, and it can tonify the heart and get rid of irritation and calm the mind; Neiguan (PC 6) is the Luo-Connecting acupoint of the Pericardium Meridian and one of the Eight Confluent Acupoints, and its major indications include the heart and stomach diseases, because of its functions of soothing stomach and calming the mind, and it can also be used to clear the heart fire and relieve restlessness by reducing manipulation. When Neiguan (PC 6) and Shenmen (HT 7) are used together, it can calm the mind and get rid of restlessness. Sanyinjiao (SP 6) is the crossing acupoint of the Spleen, Liver, and Kidney Meridians, and it can be tonified to benefit the spleen qi and nourish the Three Yin Meridians of Foot. Taichong (LR 3) is the Yuan-Primary acupoint of theLiver Meridian, and with even reinforcing-reducing manipulaitons, it can soothe and dredge the liver. As the Yuan-Primary acupoint of the Kidney Meridian, Taixi (KI 3) can strengthen yin and tonify the kidney, which is to treat the root by tonifying the congenital. Shenting (GV 24) and Baihui (GV 20) are two acupoints locate on the head essentially for calming the mind. Moreover, Baihui (GV 20) works to lift qi-blood up to the head. The above acupoints were used all along to restore the yin-yang balance and address the problem from both the superficial and original causes[5-10].
Yi Kun Yin nourishes kidney yin, clears liver and heart fire, and thus can regulate patient’s emotion and endocrine function. Compared to the needling method of regulating the Conception Vessel and calming the mind, it’s not sufficient for sleep disorder. The results suggest that the needling method of regulating the Conception Vessel and calming the mind has better therapeutic efficacy than Yi Kun Yin, which may benefit from the multiple-target effect of acupuncture. However, the exact mechanism still expects further studies.
[1] Le J. Gynecology. 7th Edition. Beijing: People’s Medical Publishing House, 2008.
[2] American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic and Coding Manual. 2nd Edition. Westchester, Illinois: American Academy of Sleep Medicine, 2005.
[3] Ministry of Public Health of People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 1997: 17-18.
[4] Cao ZY. China Gynecology. Beijing: People’s Medical Publishing House, 2004: 11-12.
[5] Huang QF, Li S, Huang Y. A survey of the treatment of climacteric syndrome with acupuncture and moxibustion after the foundation of P. R. China. Shanghai Zhenjiu Zazhi, 2006, 25(4): 43-44.
[6] Zhou YL, Li J. Survey on clinical and basic study on perimenopausal syndrome treated by moxibustion. J Acupunct Tuina Sci, 2009, 7(5): 315-320.
[7] Liu DH. Observations on the efficacy of acupuncture and moxibustion plus psychotherapy in treating female climacteric syndrome. Shanghai Zhenjiu Zazhi, 2009, 28(7): 373-374.
[8] Zhou Q, Wang JX. Clinical observation on acupuncture for perimenopausal syndrome. J Acupunct Tuina Sci, 2009, 7(3): 200-202.
[9] Li Y, Xia Y, Liu SM, Ju ZY, Shi XL, Chen MG, Cheng L, He JS. Effect of electroacupuncture on serum sex hormones in patients with perimenopausal syndrome. Shanghai Zhenjiu Zazhi, 2010, 29(4): 199-201.
[10] Shi XL, Yang S, Zhang GQ, He JS. Effect analysis on the treatment of perimenopausal depression by acupuncture and medication respectively. Shanghai Zhenjiu Zazhi, 2010, 29(12): 756-758.
Translator: Hong Jue
R246.3
A
Date: November 25, 2012
Author: Sun Yuan-zheng, chief physician, doctoral supervisor
Liu Rui, master degree candidate.
E-mail: ruicute@163.com
 Journal of Acupuncture and Tuina Science2013年3期
Journal of Acupuncture and Tuina Science2013年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Clinical Observation on Treatment of Insomnia with Puncturing Back-Shu Acupoints
- Clinical Observation on Deep Acupuncture at Huantiao (GB 30) for Patients with Chronic Prostatitis
- Clinical Observation on Acupuncture for Perimenopausal Syndrome
- Therapeutic Efficacy Observation on Acupuncture for Postmenopausal Osteoporosis
- Research Progress of Acupuncture-moxibustion for Insomnia: An Analysis of Literature in Recent 5 Years
- Therapeutic Efficacy Observation on Integrative Acupuncture Therapy for Chronic Urticaria
