Clinical Observation on Treatment of Insomnia with Puncturing Back-Shu Acupoints
Xu Tian-bing
Acupuncture-moxibustion Department, Guanggu Branch, Hubei Hospital of Traditional Chinese Medicine, Wuhan 430073, China
Clinical Observation on Treatment of Insomnia with Puncturing Back-Shu Acupoints
Xu Tian-bing
Acupuncture-moxibustion Department, Guanggu Branch, Hubei Hospital of Traditional Chinese Medicine, Wuhan 430073, China
Objective: To evaluate the clinical efficacy of puncturing Back-Shu acupoints for insomnia.
Methods: Sixty patients were randomly divided into two groups, 30 cases in each. Back-Shu acupoints acupuncture was employed in the treatment group, whereas conventional acupoints acupuncture was administered in the control group. And the efficacy was assessed by the efficiency rate of relief of sleep disorders and the global Pittsburgh Sleep Quality Index (PSQI) score.
Results: The total effective rate was 93.3% in the treatment group, versus 80.0% in the control group, showing that the two groups were significantly different (P<0.01). After treatment, the global PSQI scores in the two groups decreased compared with those before treatment (P<0.01), and the global PSQI scores of the two groups after treatment were also statistically different (P<0.05).
Conclusion: Puncturing Back-Shu acupoints can effectively reduce the global PSQI score, improve the patient's quality of life, has a good effect on insomnia.
Acupuncture Therapy; Insomnia; Points, Back-Shu
Insomnia is a subjective feeling of insufficient sleep, and an inability to fall asleep or to stay asleep as long as desired, as well as it is an unsatisfactory state of the quality and quantity of the sleep that lasts for an extended period[1-2]. In China, with the accelerating pace of life and increasing work pressure, there are increasing incidences of insomnia. At present, though the domestic and abroad medicines for insomnia have good immediate effect, they have varying degrees of side effects and can induce dependence of the patients, thus they cannot be long-term used. I have used Back-Shu acupoints for 30 patients with insomnia, and clinically compared with another 30 cases treated by conventional acupuncture as controls, which are reported as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of traditional Chinese medicine
Diagnostic criteria of traditional Chinese medicine are referred to the Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes[3]. Insomnia is the chief complaint of the patients, and accompanied by at least five of the following eight symptoms: ① Dizziness; ② headache; ③dreaminess; ④ burnout; ⑤ forgetfulness; ⑥ palpitations; ⑦ anorexia; ⑧irritability.
1.1.2 Diagnostic criteria of Western medicine
Diagnostic criteria of Western medicine are referred to the third edition of Chinese Classification and Diagnostic Criteria of Mental Disorders (CCMD-3) established by the Psychiatric Branch of Chinese Medical Association[4]: ①Typical symptoms of insomnia, sleep disorder is almost the only symptom, which induces other secondary symptoms including difficultly falling asleep, waking up easily, a lot of dreams, waking up too early in the morning, difficultly falling asleep again after waking up, unwell sensation after waking up, and being tired or sleepy during the day; ② the sleep disorder symptoms mentioned above occur at least three times per week lasting for 1 month or more; ③ insomnia causes significant distress, or reduces mental activity efficiency, or impedes patient’s social function; ④ the symptom is not caused by any kind of physical illness or mental disorder.
1.2 Inclusion criteria
Patients who have suffered from insomnia for more than 6 months and met the following conditions: Their chief complaint was physiological dysfunction of sleep (interrupted sleep or sleep disorders caused by the reduced sleep time); fatigue during daytime, dizziness, distending feeling in head and other symptoms, which were caused by sleep disorders; their ages were between 18 to 70 years old.
1.3 Exclusion criteria
The insomnia was induced by systemic diseases (such as pain, fever, cough, surgery, and so on) and external environmental interference factors; patient whose age was below 18 years old or more than 70 years old; patient who was pregnant or lactating; patient who suffered from primary severe diseases of cardiovascular, lung, liver, kidney and hematopoietic systems; patient whose sleep time reduced without daytime discomfort (short sleep shall not be considered as insomnia); patient who did not meet the inclusion criteria; patient who did not accord with the specified treatment and thus the efficacy could not be evaluated or incomplete data affect the efficacy assessment.
1.4 General data
All the 60 cases with insomnia were from the Acupuncture Clinic of our hospital, and they were randomly divided into a treatment group and a control group according to visiting sequence, 30 cases in each group. General data comparisons of the two groups’patients were shown in table 1. There was no statistically significant differences between the two groups in gender, age, disease duration, degree of insomnia, mental state, and Chinese and Western medicine treatment conditions (P>0.05), suggesting that the two groups were comparable.
Table1. Comparisons of general data between the two groups()
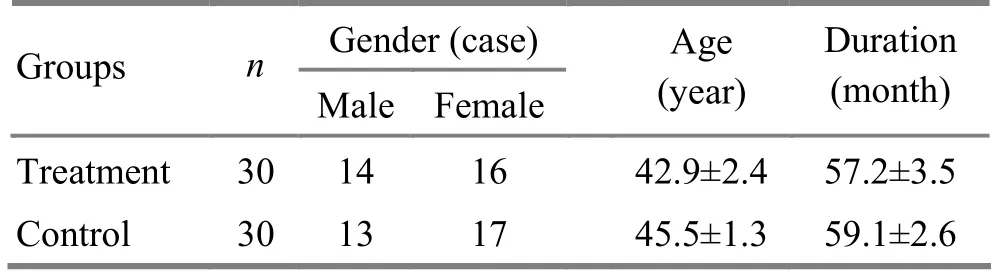
Table1. Comparisons of general data between the two groups()
The clinical flow of the two groups is shown in Fig.1.
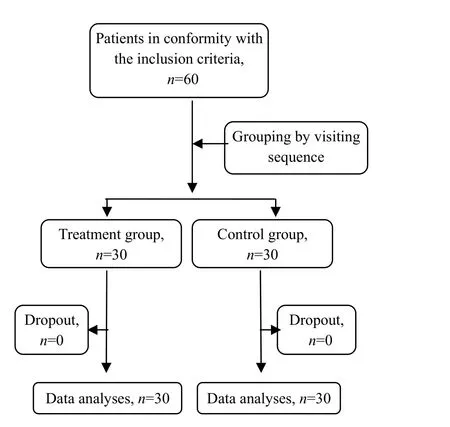
Fig.1 Clinical flow chart in the two groups
2 Methods
2.1 Treatment group
Acupoints: Xinshu (BL 15), Ganshu (BL 18), Danshu (BL 19), Pishu (BL 20) and Shenshu (BL 23)[5].
Operation: ask the patient to take a prone position. After routine disinfection of the acupuncture area skin with 75% ethanol, puncture above acupoints using stainless steel filiform needles of 0.30 mm in diameter and 40 mm in length, use even reinforcing-reducing manipulation after arrival of qi, and conduct lifting-thrusting, twisting and rotating methods, and retain the needles for 30 min.
The above acupuncture treatment was performed once a day, five days a week. And the effect was evaluated after 4 weeks of continuous treatment.
2.2 Control group
Acupoints: Baihui (GV 20), Sishencong (EX-HN 1), Yintang (GV 29), Anmian [Extra, locates at the midpoint of the connection between Yifeng (TE 17) and Fengchi (GB 20)], Shenmen (HT 4), Zhaohai (KI 6) and Shenmai (BL 62).
Acupuncture operation and treatment course were the same as those in the treatment group.
2.3 Statistical process
The SPSS 15.0 version statistical software was used for all the data analysis, and Chi-square test for rate comparison, and () for measurement data. The efficacies were compared by the paired t-test, while different groups were compared by independent sample t-test. P<0.05 indicates statistically significant difference.
第一类以广东地区为代表:20世纪90年代,为解决缺电局面,广东地区陆续投产了一些燃油电厂。后来由于燃油成本及环保等原因,这些电厂在2000年后陆续改造为天然气发电厂,例如美视电厂、钰湖电厂等。21世纪初,为配合广东大鹏LNG项目,先后建设有惠州昭阳、深圳前湾、深圳东部和广州珠江4个电厂,并取得了较好的经济效益;为配合福建LNG项目,福建也建设了晋江、厦门和莆田3个燃气电厂。
3 Therapeutic Efficacy Observation
3.1 Observation indexes
Patients in the two groups were evaluated before and after treatment by Pittsburgh Sleep Quality Index (PSQI). The PSQI consists of 19 self-assessment items and 5 other-assessment ones; and latter ones and the 19th self-assessment item are not scored. And the 18 self-assessment items which can be scored consist of seven factors, including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction, each factor is scored 0, 1, 2 or 3, and finally they are accumulated to be the global PSQI score (0 to 21 points). The higher score indicates worse sleep quality. The PSQI scale is easy to use, and has high credibility and validity, thus it can be used for clinical comprehensive evaluation of patients’ sleep quality[6].
3.2 Therapeutic effect criteria
It was determined according to therapeutic effect criteria of insomnia in the Guiding Principles for Clinical Study of New Chinese Medicines[7].
Clinical recovery: The patient’ sleep time returns to normal or the sleep time at night is more than 6 h, and the patient has a deep sleep and is energetic after waking up.
Marked effect: The patient improves significantly in sleep, and his or her sleep time increases by 3 h, and has a deeper sleep.
Improvement: The symptoms relieve, and sleep time increases less than 3 h.
3.3 Therapeutic results
3.3.1 Comparison of curative effect between the two groups
After four weeks of treatment, the total effective rate of the treatment group was 93.3%, and versus 80.0% of the control group, and the difference between the two groups was statistically significant (P<0.01), indicating that the effect in the treatment group was better than that in the control group (table 2).
3.3.2 Comparison of PSQI scores between the two groups
After treatment, the global PSQI scores of the two groups were significantly lower (P<0.01); the difference was statistically significant between the two groups (P<0.05). And it’s suggested that the two protocols of acupoint selection can significantly improve PSQI score of insomnia patients; however, there was more obvious improvement in the treatment group than the control group (table 3).
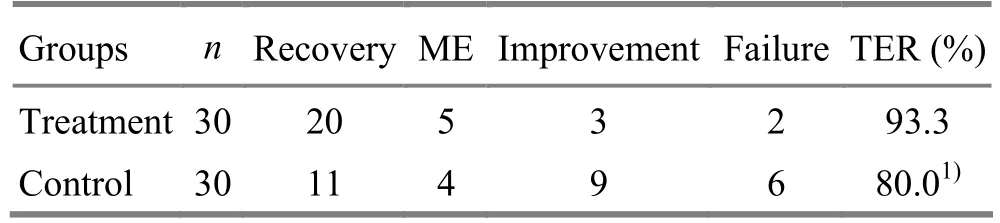
Table 2. Comparison of therapeutic effect between the two groups (case)
Table 3. Comparison of the global PSQI score between the two groups (, point)

Table 3. Comparison of the global PSQI score between the two groups (, point)
Note: Compared with before-treatment result of the same group, 1) P<0.01; compared with the control group, 2) P<0.05
4 Discussion
The ancient physicians considered that normal sleep resulted from yin-yang, qi and blood ordinary transformation of the heart, liver, spleen, kidney and other organs. Various factors can cause dysfunctions of Zang-fu organs, including liver stagnation transforming into fire, internal disturbance of phlegm-heat, deficiency of spleen qi and heart blood, fire hyperactivity due to yin deficiency and qi deficiency of the heart and gallbladder, which induces nervous mind and sleeplessness[8].
The insomnia definition of the American Sleep Disorders Center Association is as follows: Insomnia is sleep disorders caused by sleep apnea and reduced sleep time, and it is one of the subtypes of sleep difficulty and sleep disorder which are associated with neuropsychiatric disease. Modern medicine holds that insomnia is caused by multiple etiologies, including medical conditions, medications, mental illness and poor sleep habits. In most cases, depression, drug or both of them forms as the potential reasons.
The neuroanatomy has confirmed that there are spinal nerve branches in both sides of the spine where Back-Shu acupoints are located, and there are sympathetic trunk, sympathetic paravertebral sectionand the gray and white communicating branches associated with spinal nerve in the deep areas. Therefore, puncturing Back-Shu acupoints can not only effectively adjust the disorders of autonomic nervous function and the superfacial micro-circulation system, but also stimulate the internal organs to regulate nerves and the function of body fluids[9]. Puncturing Back-Shu acupoints can also regulate the imbalance of the organs function, and it can remove depression and calm mind as well as tonify deficiency to restore health qi, so that qi and blood are regulated and mind is calmed. Finally, a pathological sleep condition returns to normal one, yin-yang balance is restored in the body, and sleep quality is improved[10].
[1] Meng S, Lǚ JB, Wei RP, Xu XY. Clinical observation on combined use of Yuan-Primary and Back-Shu points in catgut embedding for insomnia. Shanghai Zhenjiu Zazhi, 2011, 30(10): 677-678.
[2] Shi Q, Chen C, Gao C, Tian C, Zhou W, Zhang B, Han J, Dong XP. Clinical and familial characteristics of ten Chinese patients with fatal family insomnia. Biomed Environ Sci, 2012, 25(4): 471-475.
[3] State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing: Nanjing University Press, 1994: 175.
[4] Chinese Society of Psychiatry. Chinese Classification and Diagnostic Criteria of Mental Disorders. 3rd Edition. Jinan: Shandong Science & Technology Press, 2001: 151.
[5] Shi XM. Acupuncture-moxibustion Science. Beijing: China Press of Traditional Chinese Medicine, 2002: 231.
[6] Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res, 1989, 28(2): 193-213.
[7] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: People’s Medical Publishing House, 1993: 186.
[8] Yuan X. Clinical observation on acupuncture plus auricular point sticking in treating insomnia. J Acupunct Tuina Sci, 2010, 8(5): 302-303.
[9] Lin WZ, Wang P. Experimental Acupuncture Science. Shanghai: Shanghai Scientific and Technical Publishers, 2003: 256-258.
[10] Li JP, Zhang H, He PD. Observations on the efficacy of auricular point plaster therapy plus aligned cupping on dorsal bladder meridians in treating chronic insomnia. Shanghai Zhenjiu Zazhi, 2011, 30(4): 230-232.
Translator: Deng Ying
R246.1
A
Date: December 20, 2012
Author: Xu Tian-bing, associate chief physician.
E-mail: xufengshou1999@sohu.com
 Journal of Acupuncture and Tuina Science2013年3期
Journal of Acupuncture and Tuina Science2013年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Efficacy Observation on Acupuncture for Postmenopausal Osteoporosis
- Treatment of 30 Cases of Vertigo due to Qi-blood Deficiency by Pricking Jingbailao (EX-HN 15) with Fire Needle Therapy
- Clinical Observation on Deep Acupuncture at Huantiao (GB 30) for Patients with Chronic Prostatitis
- Clinical Observation on Acupuncture for Perimenopausal Syndrome
- Research Progress of Acupuncture-moxibustion for Insomnia: An Analysis of Literature in Recent 5 Years
- Therapeutic Efficacy Observation on Integrative Acupuncture Therapy for Chronic Urticaria
