Inferior vena cava obstruction and collateral circulation as unusual manifestations of hepatobiliary cystadenocarcinoma
Athens, Greece
Inferior vena cava obstruction and collateral circulation as unusual manifestations of hepatobiliary cystadenocarcinoma
Nikolaos Arkadopoulos, Anneza I Yiallourou, Constantinos Palialexis, Emmanouil Stamatakis, Evi Kairi-Vassilatou and Vassilis Smyrniotis
Athens, Greece
BACKGROUND:Hepatobiliary cystadenocarcinoma represents a rare epithelial malignant tumor derived from the intrahepatic bile duct.
METHODS:A 71-year-old woman, who had undergone laparoscopic drainage of a cystic lesion of the right hepatic lobe, was misdiagnosed as having hepatic echinococcal disease, and received intracystic infusion of 95% ethanol four years ago. She was admitted to our hospital for further treatment.
RESULTS:Physical examination revealed dilated superf i cial veins across the right abdominal wall. After mapping the direction of blood fl ow in these vessels, we assumed that this was a sign of inferior vena cava obstruction. Abdominal ultrasound, computed tomography, magnetic resonance imaging combined with magnetic resonance angiography showed a large cystic mass in the right upper quadrant and epigastrium, displacing the adjacent structures, adherent to the inferior vena cava, which was not patent, resulting in dilation of superf i cial epigastric veins. The patient underwent an exploratory laparotomy. Total excision of the huge mass measuring 16× 15 cm was possible under selective vascular exclusion of the liver. Removal of the tumor resulted in immediate restoration of fl ow in the inferior vena cava. On the basis of the pathology and fi ndings of immunohistochemical analysis, a hepatobiliary cystadenocarcinoma was diagnosed.
CONCLUSIONS:In the present case, hepatobiliary cystadenocarcinoma was accompanied by dilated superf i cial venous collaterals due to inferior vena cava obstruction. Selective vascular exclusion of the liver allowed a safe oncological resection of the tumor.
(Hepatobiliary Pancreat Dis Int 2013;12:329-331)
hepatobiliary cystadenocarcinoma; inferior vena cava obstruction; collateral circulation
Introduction
Hepatobiliary cystadenocarcinoma represents a rare epithelial malignant tumor.[1]Cystadenocarcinoma may arisede novofrom the intrahepatic bile ducts forming multilocular cysts lined by mucus secreting epithelium with papillary infoldings. It is most often solitary and large at the time of diagnosis. This clinical entity may be misdiagnosed as a hepatic abcess, hydatid cyst, metastatic tumor with cystic degeneration, or even a simple hepatic cyst. We herein report a patient presenting with dilated superf i cial veins due to inferior vena cava (IVC) obstruction caused by a huge hepatobiliary cystadenocarcinoma.
Case report
A 71-year-old Caucasian woman was suspected of having a cystic lesion of the right hepatic lobe, which was misdiagnosed as hepatic echinococcal disease, four years ago. The patient initially underwent laparoscopic drainage of the cyst followed a few months later by intracystic infusion of 95% ethanol. The cyst gradually enlarged with a diameter of 16 cm on admission to our hospital. She suffered from discomfort in the right upper quadrant. Dilated superf i cial veins were observedacross the right abdominal wall (Fig. 1A). Mapping the direction of blood fl ow in these vessels revealed that this was a sign of IVC obstruction. Moreover, an enlarged liver could be palpated. Serologic examination for hepatitis or parasitic infection was negative. Tumor markers were all within normal ranges.

Fig. 1.A. The patient's right abdominal wall showing dilated superficial veins;B. MR angiography depicting the large cystic mass adherent to the IVC, which was not patent (short arrows), the displacement of the adjacent structures, and the dilated superficial epigastric veins (long arrow);C. Contrast-enhanced T1-weighted axial MR image of the liver confirming the cystic nature of the mass and the absence of contrast uptake.
Abdominal ultrasound, computed tomography, and magnetic resonance (MR) imaging combined with magnetic resonance angiography were performed (Fig. 1B). The radiographic workup showed a large cystic mass in the right upper quadrant and epigastrium, displacing the adjacent structures, adherent to the IVC, which was not patent (Fig. 1C), resulting in dilation of superf i cial epigastric veins (Fig. 1C). The patient underwent an exploratory laparotomy. A huge encapsulated mass measuring 16×15 cm was found below the liver, displacing the hepatoduodenal ligament, the stomach and the large bowel (Fig. 2A). The obstruction of the IVC was due to mass effect of the tumor and collateral circulation. Total excision of the lesion was possible by selective vascular exclusion of the liver, i.e. a combined occlusion of the hepatoduodenal ligament and the extrahepatic trunks of the major hepatic veins.[2]Removal of the tumor resulted in immediate restoration of fl ow in the IVC. The patient perioperatively required two units of packed red blood cells (pRBCs) to maintain Hb>9 g/dL. Her postoperative course was uneventful.
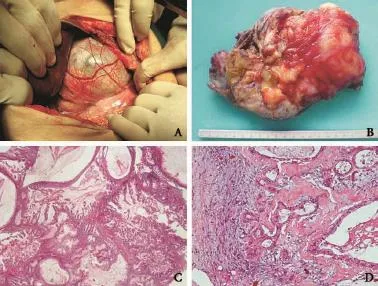
Fig. 2.A. Intraoperative image of the huge encapsulated mass located exactly below the liver;B. Gross view of a large multicystic tumor of the liver, measuring 16×15×5 cm;C. Histological section of the hepatobiliary neoplasm showing complex papillary structures in mucus-f i lled cystic spaces, separated by thin stroma (hematoxylin-eosin, original magnif i cation ×25);D) Histological section of the hepatobiliary neoplasm showing capsular infiltration by neoplasmatic glands (hematoxylin-eosin, original magnif i cation ×120).

Fig. 3.Postoperative contrast-enhanced T1-weighted axial MR image of the liver showing complete resection of the mass and restoration of fl ow in the IVC.
Macroscopic examination showed an encapsulated cystic lesion measuring 16×15×5 cm, with multilocular cysts characterized by internal septa and nodularity of the internal wall. Hemorrhagic, bilious and mucinous fl uid was retained by the cysts (Fig. 2B). Histologically, the cyst was a hepatobiliary cystic neoplasm with areas of complex papillary architecture, moderate to remarkable nuclear atypia and foci of stromal and capsular inf i ltration by neoplastic cells. Ovarian-like stroma was also detected (Fig. 2C, D). On the basis of the above mentioned fi ndings and the immunohistochemical analysis, a hepatobiliary cystadenocarcinomawas diagnosed.
Upon 15 months of follow-up, recurrence of the tumor has not been observed (Fig. 3).
Discussion
Hepatobiliary cystadenocarcinoma was divided into two groups: one arising from preexisting cystadenoma with mesenchymal stroma which predominantly occurs in women with a rather good prognosis, and the other not associated with preexisting cystadenoma which occurs in men with an extremely aggressive clinical course.[1]
Clinical manifestations of cystadenocarcinomas may vary from upper abdominal pain or discomfort[3]to a clearly palpable mass. Asymptomatic lesions may be discovered incidentally during radiologic or surgical procedures for unrelated conditions. Jaundice due to compression of the bile duct or ascites due to compression of the vena cava and hepatic vein are rarely encountered.[4]In our patient, there were dilated veins across the right abdominal wall, a sign attributed to the obstruction of the IVC. To our knowledge, this physical sign has not been reported.
Preoperative imaging studies are crucial, despite the fact that differential diagnosis between hepatobiliary cystadenoma and cystadenocarcinoma on the basis of imaging fi ndings alone is not reliable.[5]Ultrasound, computed tomography and gadolinium enhanced MRI in combination with MRCP are valuable tools in accurately locating the tumor. The presence of a multilocular hypodense mass with echogenic internal septations and papillary projections into the cystic space or wall thickening with fi ne septal calcif i cations should trigger the suspicion of cystadenocarcinoma. Aspiration of cystic content for cytological examination has been reported as an effective way for early detection of suspicious patients.[6]However, some authors emphasize the risk of contamination by bacterial elements inside the tumor as well as the seeding of malignant cells along the needle track.[3]Complete surgical resection remains the treatment of choice for hepatobiliary cystadenocarcinoma.[7,8]The tumor may be of low grade malignancy and those patients in whom adequate local clearance was obtained have a relatively good prognosis.[9]With regards to prognosis of cystadenocarcinoma after liver excision, Uchiro et al[10]reported that the 3- and 5-year survival rates were 69% and 43%, respectively.
In conclusion, hepatobiliary cystadenocarcinoma is an unusual malignant tumor of the liver, which can be frequently misdiagnosed. In the present patient, the lesion was initiallly misdiagnosed as a hydatid cyst until the patient developped the unique clinical fi nding of dilated superf i cial veins due to IVC obstruction. Our surgical approach of selective vascular exclusion of the liver allowed complete resection of the tumor with minimal blood loss and adequate tumor-free margin.
Contributors:YAI drafted the manuscript. KVE performed histopathological and immunohistochemical analysis. AN was responsible for critical revision of scientif i c content. All authors contributed to the design and interpretation of the study and to further drafts. YAI is the guarantor.
Funding:None.
Ethical approval:Not needed.
Competing interests:No benef i ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Devaney K, Goodman ZD, Ishak KG. Hepatobiliary cystadenoma and cystadenocarcinoma. A light microscopic and immunohistochemical study of 70 patients. Am J Surg Pathol 1994;18:1078-1091.
2 Smyrniotis V, Arkadopoulos N, Kostopanagiotou G, Farantos C, Vassiliou J, Contis J, et al. Sharp liver transection versus clamp crushing technique in liver resections: a prospective study. Surgery 2005;137:306-311.
3 Sang X, Sun Y, Mao Y, Yang Z, Lu X, Yang H, et al. Hepatobiliary cystadenomas and cystadenocarcinomas: a report of 33 cases. Liver Int 2011;31:1337-1344.
4 Zhang M, Yu J, Yan S, Zheng SS. Cystadenocarcinoma of the liver: a case report. Hepatobiliary Pancreat Dis Int 2005;4: 464-467.
5 Kinoshita H, Tanimura H, Onishi H, Kasano Y, Uchiyama K, Yamaue H. Clinical features and imaging diagnosis of biliary cystadenocarcinoma of the liver. Hepatogastroenterology 2001;48:250-252.
6 Mortelé KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics 2001;21:895-910.
7 Läuffer JM, Baer HU, Maurer CA, Stoupis C, Zimmerman A, Büchler MW. Biliary cystadenocarcinoma of the liver: the need for complete resection. Eur J Cancer 1998;34:1845-1851.
8 Okazaki M, Shimizu I, Shiraishi T, Horie T, Iuchi A, Atagi Y, et al. Hepatobiliary cystadenocarcinoma without mesenchymal stroma showing a good prognosis. J Gastroenterol Hepatol 2006;21:1356-1358.
9 Del Poggio P, Jamoletti C, Forloni B, De Benedictis R, Mattiello M, Corti D, et al. Malignant transformation of biliary cystadenoma: a diff i cult diagnosis. Dig Liver Dis 2000;32:733-736.
10 Uchiro J, Kurauchi N, Sazi H, Takahashi M, Manabe K. Treatment of cystic adenocarcinoma of the liver. Kan-Tan-Sui (Hepato-Biliary-Pancreas) 1992;24: 285-293.
Received August 20, 2011
Accepted after revision August 5, 2012
AuthorAff i liations:4th Department of Surgery, Attikon University Hospital, University of Athens, Athens Greece (Arkadopoulos N and Smyrniotis V); 2nd Department of Surgery (Yiallourou AI), Department of Radiology (Palialexis C), Department of Anesthesiology (Stamatakis E) and Department of Pathology (Kairi-Vassilatou E), Aretaieion Hospital, University of Athens, Athens Greece
Anneza I Yiallourou, MD, 2nd Department of Surgery, Aretaieion Hospital, University of Athens, 76, Vasilissis Sophias Avenue, Athens 11528, Greece (Tel: 302107286182; Fax: 302107286128; Email: annyiallo@yahoo.gr)
© 2013, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(13)60052-1
 Hepatobiliary & Pancreatic Diseases International2013年3期
Hepatobiliary & Pancreatic Diseases International2013年3期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Surgical treatment of hepatocellular carcinoma with inferior vena cava tumor thrombus:a new classification for surgical guidance
- Pancreatic duct disruption and nonoperative management: the SEALANTS approach
- Pancreatic Castleman disease treated with laparoscopic distal pancreatectomy
- Clinical features and outcomes of patients with severe acute pancreatitis complicated with gangrenous cholecystitis
- Double-blind randomized sham controlled trial of intraperitoneal bupivacaine during emergency laparoscopic cholecystectomy
- Propofol inhibits the adhesion of hepatocellular carcinoma cells by upregulating microRNA-199a and downregulating MMP-9 expression
