不同质子泵抑制剂与抗血小板药物联用时心血管安全性Meta分析
齐乐,陈洪
(1.东南大学医学院,江苏南京 210009;2.东南大学附属中大医院,江苏南京 210009)
口服氯吡格雷与阿司匹林双联抗血小板药物是急性冠脉综合征(acute coronary syndrome,ACS),尤其是冠状动脉介入治疗术后(coronary artery interventional therapy,PCI)患者预防心源性死亡、心肌梗死、支架内血栓、靶血管再次血运重建等心血管事件的标准治疗方案。双联抗血小板治疗虽然降低了缺血性心血管事件的发生率,但同时增加了胃肠道损伤的风险,特别是对于老年人和既往曾有消化性溃疡病史的患者,会明显增加消化道出血的发生率。为了预防消化道出血的不良反应,临床指南推荐双联抗血小板药物与质子泵抑制剂(proton pump inhibitors,PPI)联合使用[1-3]。然而,一些研究发现,与不联合使用PPI相比,抗血小板药物联合使用PPI会增加心血管事件的发生;研究同时发现,选用不同种类的PPI时关于心血管事件的发生率的结论各有差异。因此,为了既保证氯吡格雷与阿司匹林的疗效,又最大限度地减少胃肠道不良反应,如何合理选用PPI是一个具有重要意义的问题。
1 材料与方法
1.1 纳入标准
1.1.1 纳入文献类型 随机对照试验、观察性研究及回顾性研究。
1.1.2 研究对象 (1)年龄、性别不限,符合2009年美国心脏病学会/美国心脏病协会及心血管造影与介入联合会关于ACS的诊断标准且长期使用阿司匹林和氯吡格雷的患者;(2)既往3个月内未使用其他抗血小板药物、PPI或其他抑酸药物;(3)使用PPI期间无药物更换;(4)药物使用剂量均符合指南推荐的标准用量。
1.1.3 结局指标 主要不良心血管事件(major adverse cardiovascular events,MACE),包括心源性死亡、非致死性心肌梗死、心绞痛、靶血管再次血运重建、再次PCI或冠状动脉旁路移植术(coronary artery bypass grafting,CABG)。
1.2 剔除标准
(1)文献类型:综述、病例报告、信件、会议记录、动物试验、基础试验。(2)缺少干预组数据和正在进行的研究。(3)随访时间少于半年。
1.3 文献检索与筛查
1.3.1 数据库 计算机检索Cochrane图书馆、PubMed、EMbase、SSCI、Web of science数据库,检索时间均从2010年1月至2012年9月,限制语言为英语。
1.3.2 检索策略 关键词 clopidogrel、asipirin、proton pump inhibitor、omeprazole、rabeprazole、esomeprazole、lansoprazole、pantoprazole、cardiovascular event。
1.4 质量评价及资料提取
使用统一的质量评价表,由两位研究者独立对每篇符合纳入标准的文献进行质量评价和资料提取,并交叉核对,如有分歧,通过讨论协助解决。方法学质量依据Cochrane手册4.2.6版非随机对照试验的质量评价标准进行评价。在文献的选择性偏倚方面,主要检查组间可比性和影响因素的分析、调整;对于实施偏倚,主要是考察干预措施的准确性。失访偏倚和测量偏倚的评价与随机对照试验的评价相同。提取资料主要包括:(1)一般资料,即文题、作者姓名、发表日期和文献来源;(2)研究特征,即研究对象的一般情况、各组患者的基线可比性、干预措施;(3)结局指标,即MACE,包括心源性死亡、非致死性心肌梗死、心绞痛、靶血管再次血运重建、再次PCI或CABG(表1)。
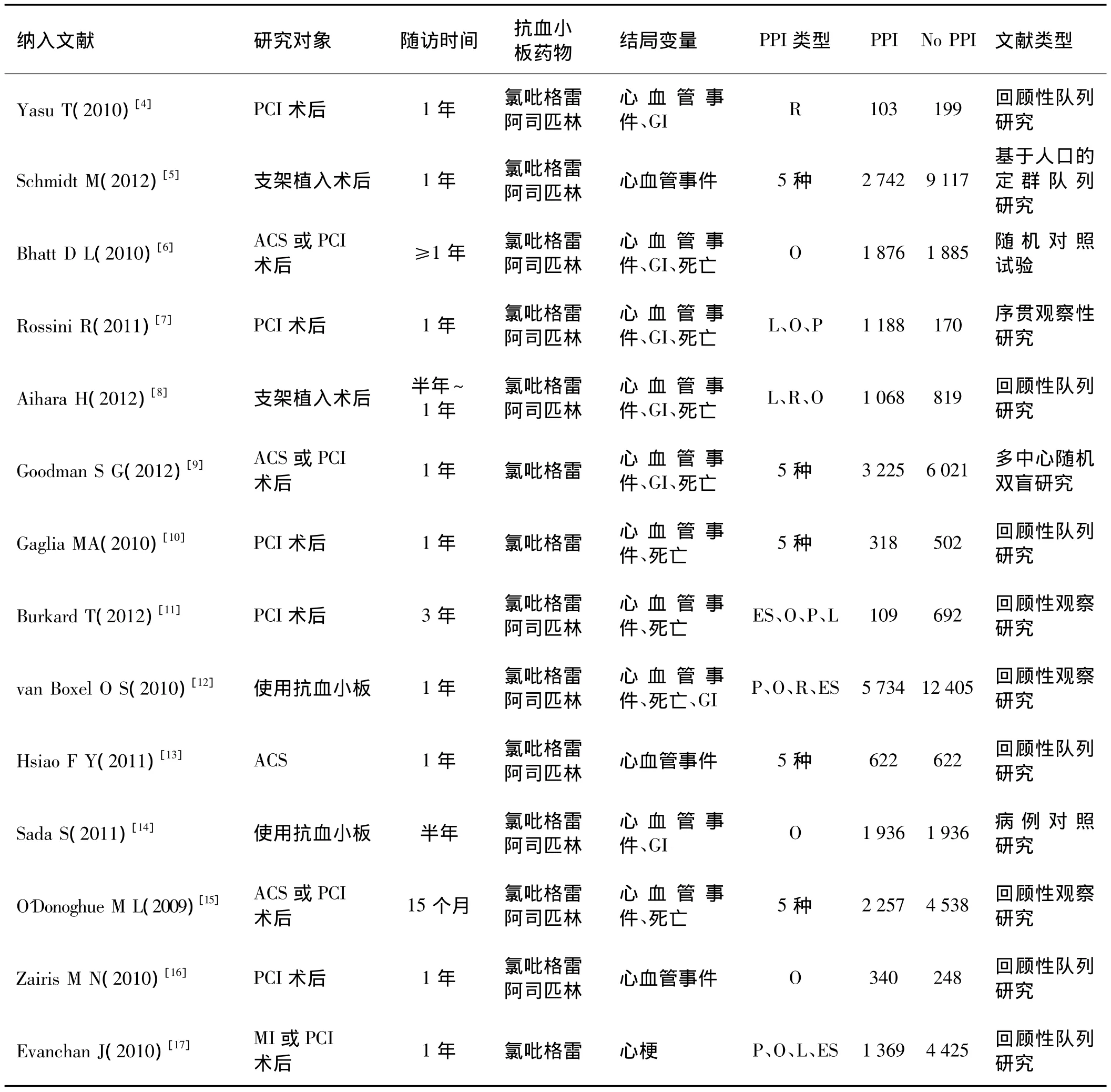
表1 纳入文献基本情况
1.5 统计学处理
采用Cochrane协作网提供的RevMan 5.0软件从心血管事件风险结局指标进行Meta分析,通过计数资料计算风险比(RR),并给出其95%可信区间,以Meta分析森林图(MetaView)形式描述呈现。纳入研究间的异质性采用χ2检验,当P<0.1和I2>50%时采用随机效应模型,反之则采用固定效应模型进行合并分析。纳入足够多的研究时,则进行漏斗图分析判断是否存在发表偏倚。
2 结 果
14篇文献纳入研究,共67 131例患者,均满足纳入标准。
2.1 奥美拉唑与抗血小板药物联用对心血管事件发生影响
共纳入研究 10 篇[5-7,9-10,12-16],各研究间有统计学异质性(I2=83%),故采用随机效应模式进行Meta分析(表2)。结果显示,奥美拉唑与抗血小板药物联用较单独使用抗血小板药物可增加心血管事件发生的风险 [RR=1.32,95%CI(1.01,1.71)]。
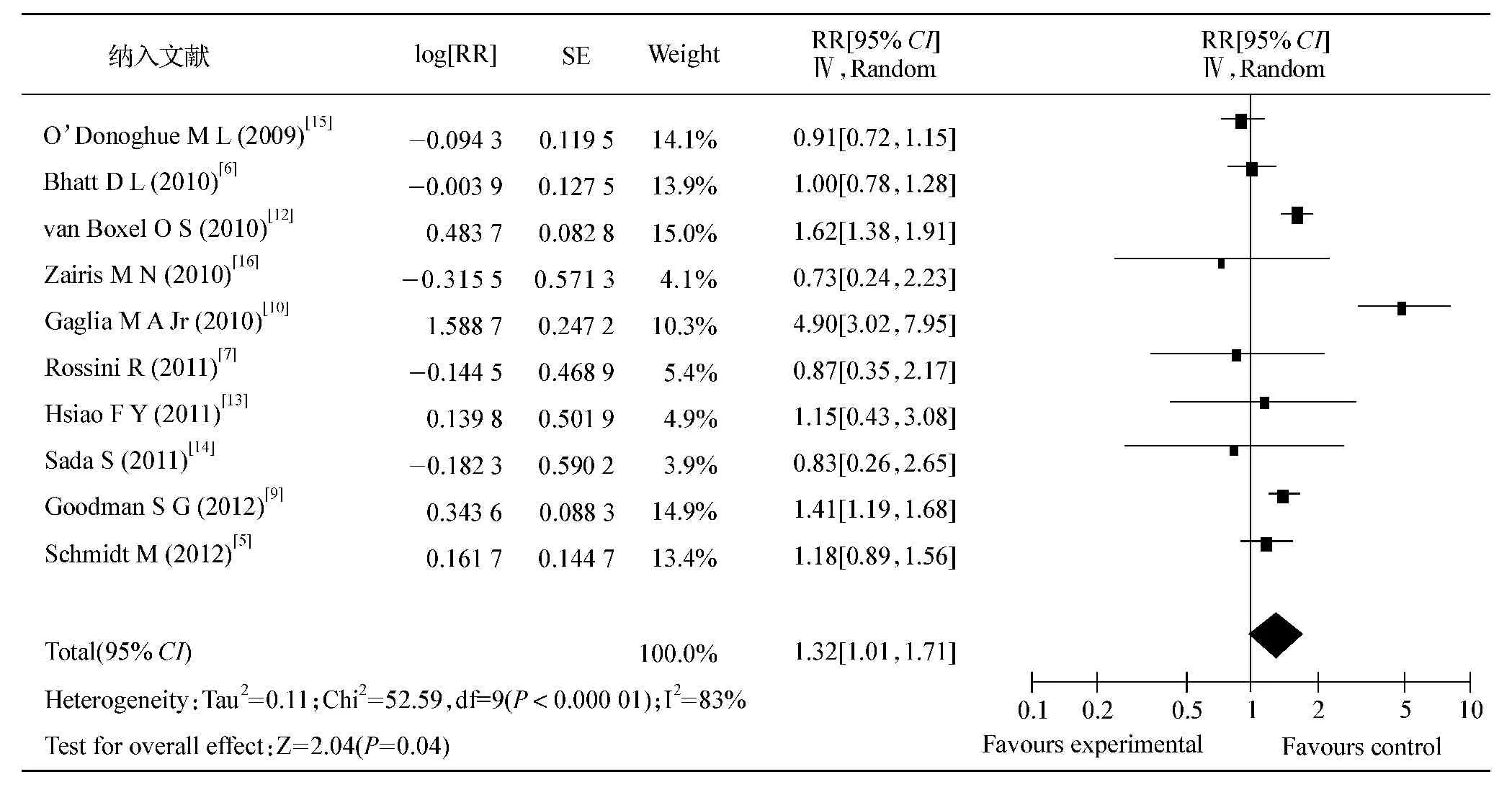
表2 奥美拉唑与抗血小板药物联用对心血管事件发生影响的Meta分析
2.2 雷贝拉唑与抗血小板药物联用对心血管事件发生影响
共纳入研究 6 篇[4-5,9-10,12-13],各研究间无统计学异质性(I2=5%),故采用固定效应模式进行Meta分析(表3)。结果显示,雷贝拉唑与抗血小板药物联用较单独使用抗血小板药物可增加心血管事件发生的风险[RR=1.57,95%CI(1.12,2.19)]。
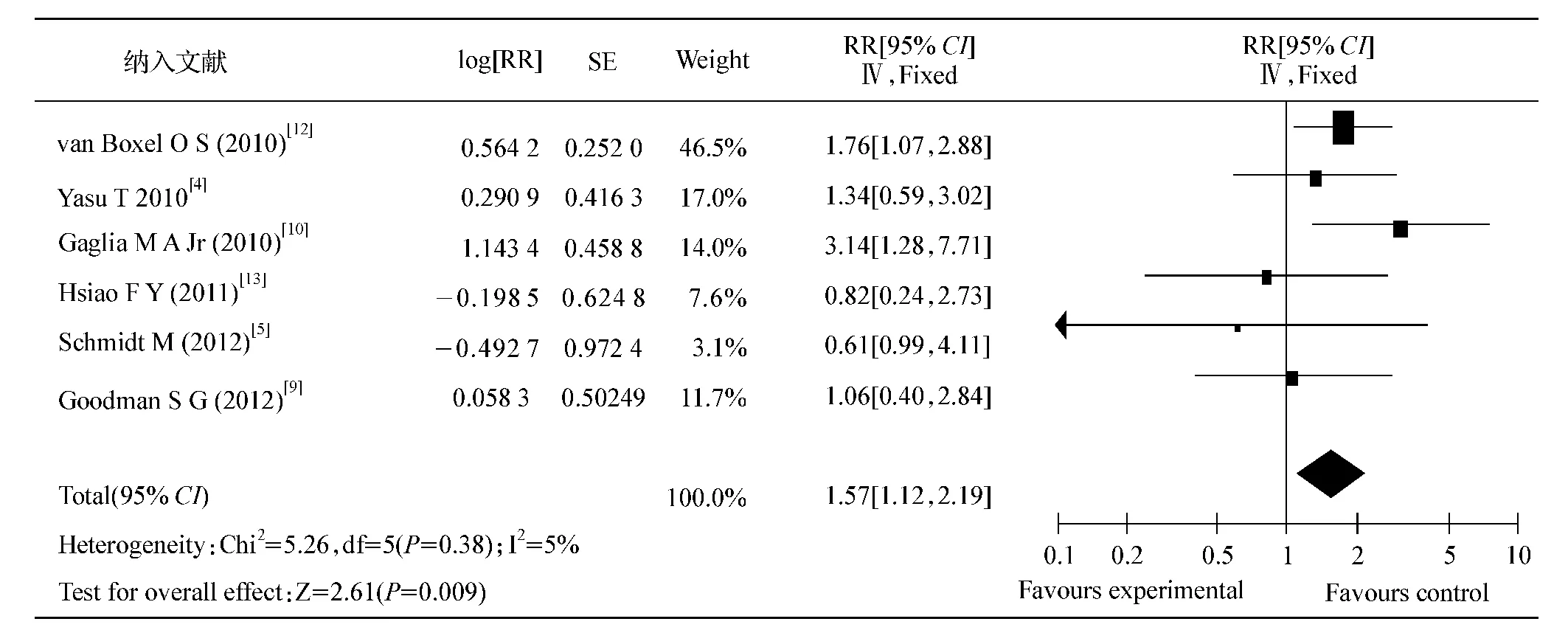
表3 雷贝拉唑与抗血小板药物联用对心血管事件发生影响的Meta分析
2.3 兰索拉唑与抗血小板药物联用对心血管事件发生影响
共纳入研究 6 篇[5,7,9-10,13,16],各研究间无统计学异质性(I2=41%),故采用固定效应模式进行Meta分析(表4)。结果显示,兰索拉唑与抗血小板药物联用较单独使用抗血小板药物在心血管事件发生的风险上差异无统计学意义[RR=1.11,95%CI(0.93,1.32)]。
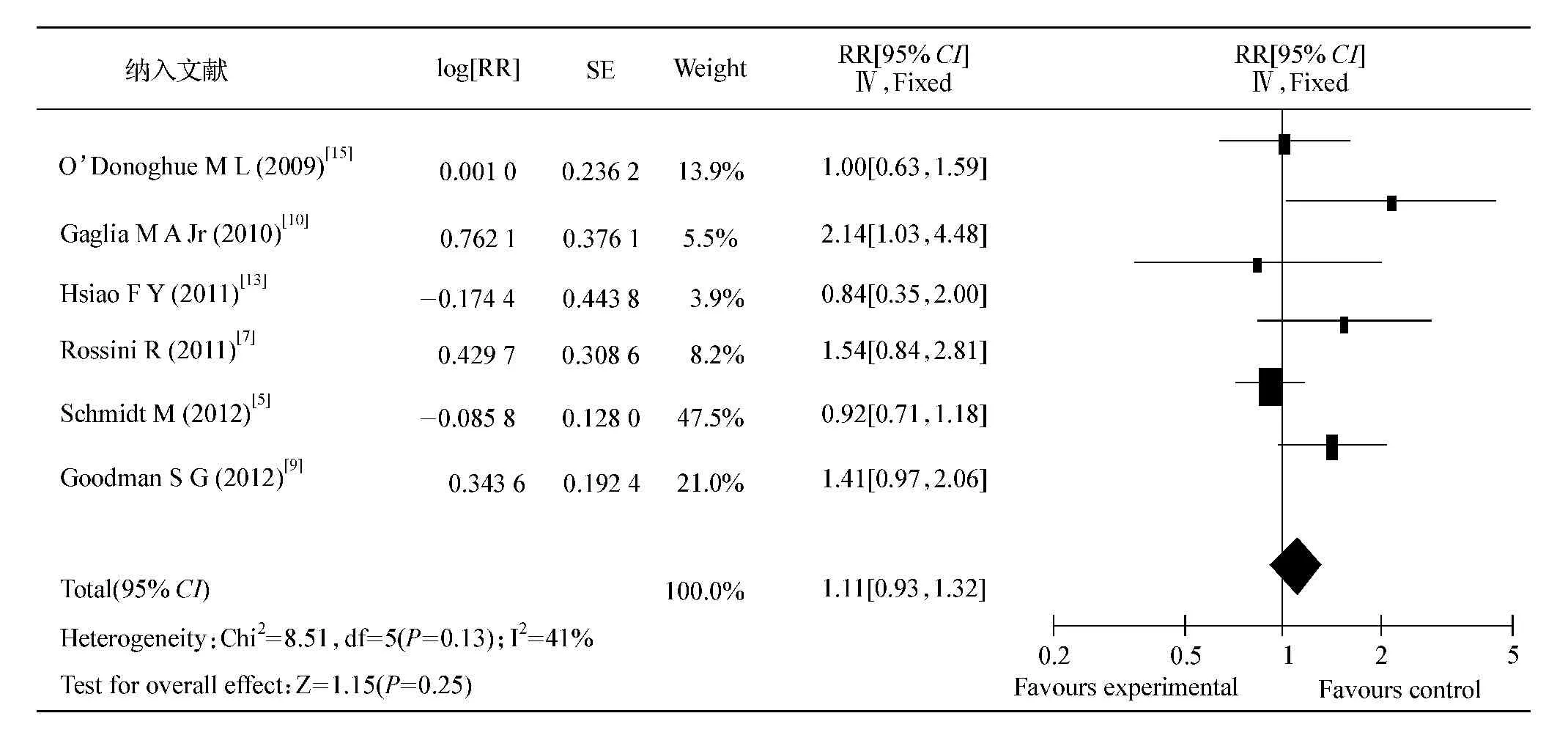
表4 兰索拉唑与抗血小板药物联用对心血管事件发生影响的Meta分析
2.4 泮托拉唑与抗血小板药物联用对心血管事件发生影响
共纳入研究 7 篇[5,7,9-10,12-13,16],各研究间有统计学异质性(I2=86%),故采用随机效应模式进行Meta分析(表5)。结果显示,泮托拉唑与抗血小板药物联用较单独使用抗血小板药物在心血管事件发生的风险上差异无统计学意义[RR=1.24,95%CI(0.91,1.68)]。
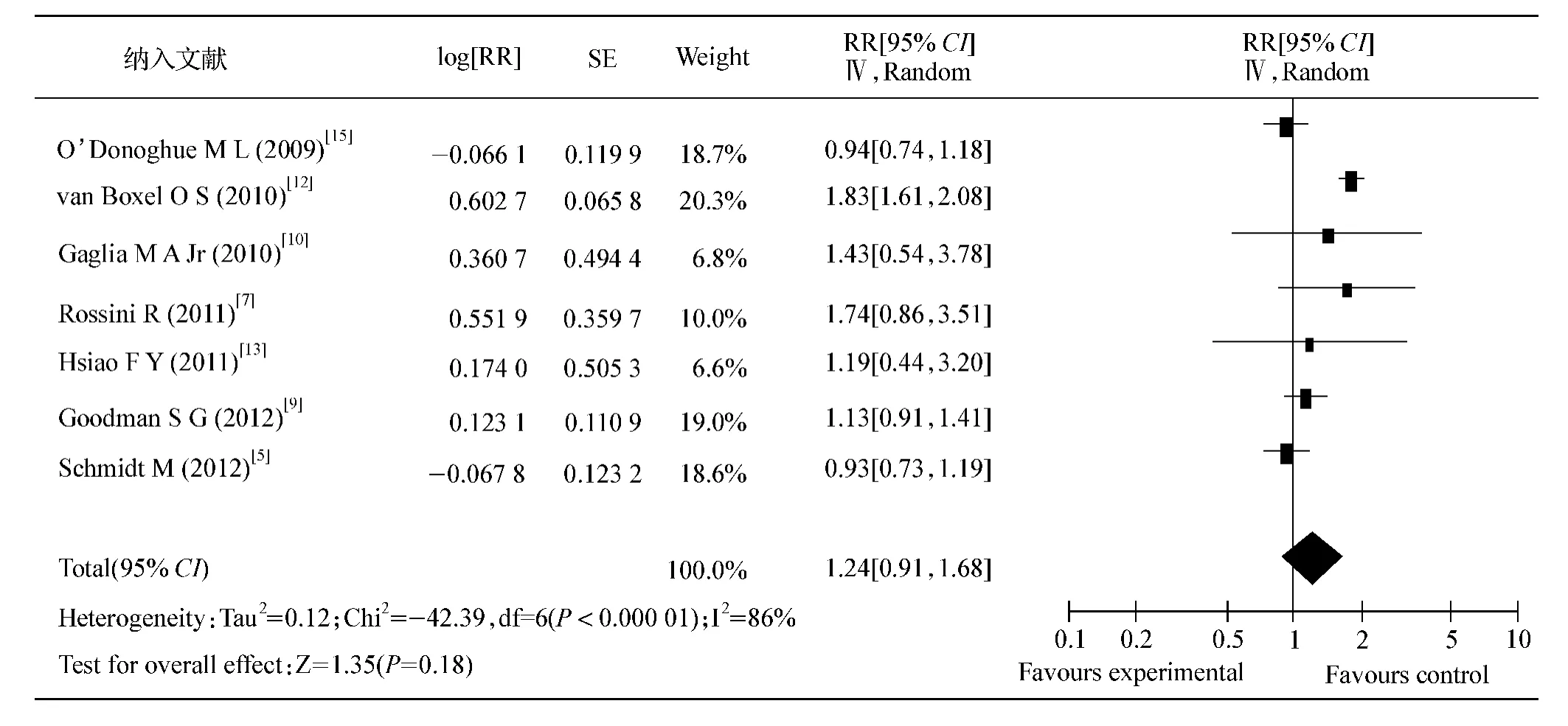
表5 泮托拉唑与抗血小板药物联用对心血管事件发生影响的Meta分析
2.5 埃索美拉唑与抗血小板药物联用对心血管事件发生影响
共纳入研究 6 篇[5,9-10,12-13,16],各研究间有统计学异质性(I2=88%),故采用随机效应模式进行Meta分析(表6)。结果显示,埃索美拉唑与抗血小板药物联用较单独使用抗血小板药物在心血管事件发生的风险上差异无统计学意义[RR=1.34,95%CI(0.93,1.92)]。
3 讨 论
本研究以抗血小板药物与PPI联用对比单用抗血小板药物的心血管事件发生指标,采用Cochrane系统评价方法对符合纳入标准的14篇原始研究进行Meta分析,涵盖病例67 131例,结果发现奥美拉唑和雷贝拉唑可明显增加心血管事件的发生风险,而其余3种PPI对于临床上心血管事件的发生均无明显影响。
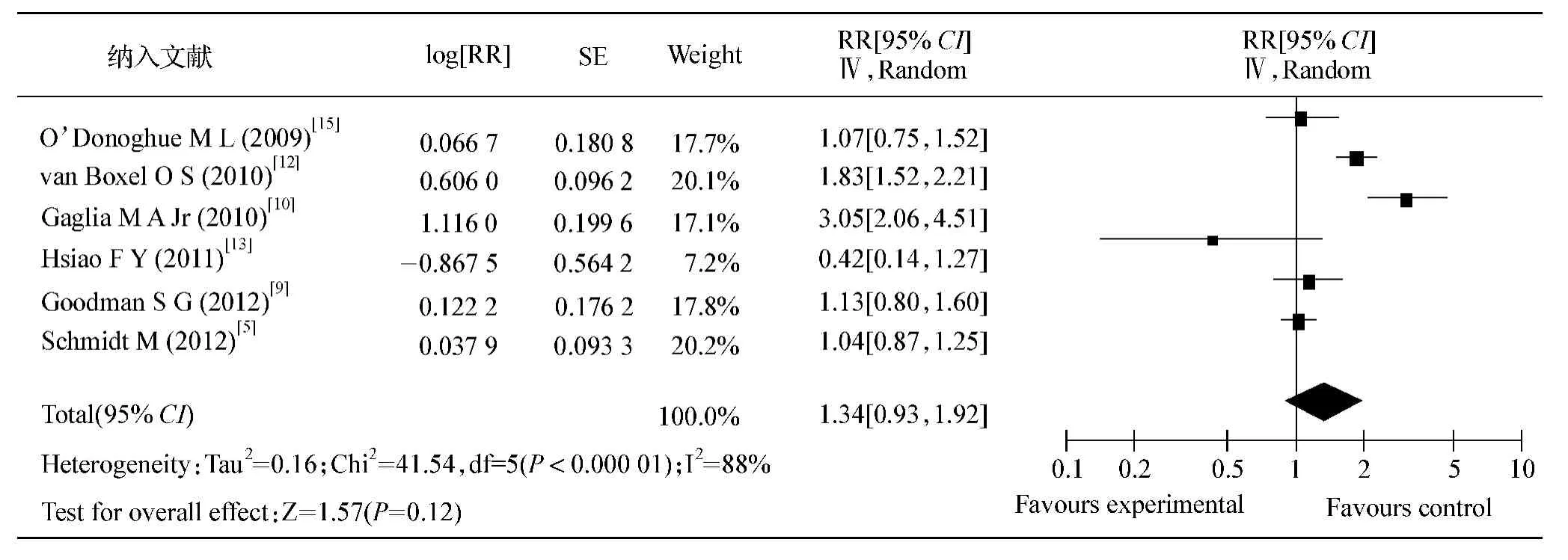
表6 埃索美拉唑与抗血小板药物联用对心血管事件发生影响的Meta分析
当前冠心病作为一种严重危害人们健康的常见病、多发病,每年约有百万患者因发生心肌梗死或接受冠状动脉介入治疗术。而阿司匹林与氯吡格雷双联抗血小板治疗对具有冠心病危险因素患者心血管事件的二级预防及PCI术后血栓的预防有重要作用,尤其是ACS患者和支架置入术后的患者,更加强调双联抗血小板治疗的重要性。2009年美国心脏病学会/美国心脏病协会及心血管造影与介入联合推荐应用双联抗血小板药至少12个月[1]。一些临床指南推荐,双联抗血小板治疗与PPI联合使用来预防消化道出血不良反应[1-2]。然而,最近发表的研究显示,合用PPI在有效减少消化道出血发生率的同时,可能影响氯吡格雷的血小板聚集抑制效应,进而削弱其心血管保护作用[18-22]。但进一步的研究认为,不同类型的PPI与抗血小板药物联合使用时,心血管事件的发生几率各不相同[23-29,31-33,35]。
药物相互作用机制的研究表明,PPI会干扰氯吡格雷的代谢。氯吡格雷是一种新型噻吩吡啶类衍生物,本身不具有抗血小板活性,在体内须经过肝脏细胞色素P450氧化酶(cytochrome P450,CYP450)氧化水解成活性代谢产物后才能选择性地、不可逆地与血小板表面二磷酸腺苷(ADP)受体P2Y12结合,抑制纤维蛋白原与血小板糖蛋白GPⅡb/Ⅲa受体结合及继发的ADP介导糖蛋白GPⅡb/Ⅲa复合物的活化,进而抑制血小板的聚集[30,34,36]。CYP450 的同工酶 CYP2C19、CYP3A4、CYP1A2、CYP2C9、CYP3A5、CYP2B6 等参与氯吡格雷的代谢过程,其中CYP2C19是氯吡格雷生物活性转化的主要代谢酶,其活性对氯吡格雷生物的活性转化过程起决定性作用[37-38]。另一方面,PPI也是主要由肝脏中CYP450同工酶催化完成氧化代谢。奥美拉唑、兰索拉唑、泮托拉唑、埃索美拉唑代谢的主要途径是通过 CYP2C19,次要途径为 CYP3A4[39]。雷贝拉唑主要经还原消除,且无需代谢酶介导,受 CYP2C19和CYP3A4影响较少。故PPI与氯吡格雷合用时可能会因共同竞争CYP2C19的同一结合位点而影响各自的药物作用,其受影响程度和结果取决于与CYP450同工酶相对亲合力的大小,高亲和力化合物将与酶结合并抑制低亲和力化合物的生物转化。Li等[40]使用人类肝脏微粒体制备物和重组CYP2C19(rCYP2C19)来研究奥美拉唑、埃索美拉唑、兰索拉唑、泮托拉唑、雷贝拉唑对CYP2C19活性竞争性抑制的效力强度和特异性,结果显示兰索拉唑>奥美拉唑>埃索美拉唑>雷贝拉唑>泮托拉唑。Blume等[41]研究亦得到同样的结果。但在实际临床应用中,对于5种PPI与氯吡格雷联用是否与心血管事件发生相关联尚未有统一的结论。
本研究结果证实,奥美拉唑或雷贝拉唑增加心血管事件发生,而兰索拉唑、埃索美拉唑及泮托拉唑则不增加。可能的机制有:(1)奥美拉唑代谢主要依赖CYP2C19,故可明显降低氯吡格雷的抗血小板作用。(2)雷贝拉唑虽无需代谢酶介导,受 CYP2C19和CYP3A4影响较少,但其代谢产物雷贝拉唑硫醚对CYP2C19具有较强的抑制效力[42],可能会影响氯吡格雷的抗血小板作用。(3)埃索美拉唑为奥美拉唑的左旋异构体,其抑酸作用更强,体内个体差异较小,疗效较稳定,但肝内代谢中埃索美拉唑主要依赖CYP3A4代谢[43]。当氯吡格雷通过CYP2C19的代谢时,对氯吡格雷的抗血小板作用抑制较小。(4)泮托拉唑则具有独特的硫酸化代谢旁路,当有氯吡格雷通过CYP2C19代谢时,它可通过旁路代谢[44],因此对氯吡格雷抗血小板作用影响较小。
本研究虽通过Meta分析得出了一定的结论,但这些结论也存在着一定的局限性:(1)目前以不同的质子泵抑制剂作为的临床试验的文献数目较少,而且文献之间存在高度异质性,对氯吡格雷与PPI如何联用还需更多临床试验的证实。(2)双联抗血小板治疗过程中,氯吡格雷和阿司匹林共同维持机体总体抗血小板效应的平衡,当氯吡格雷的抗血小板效应因某种因素受到抑制时,阿司匹林抗血小板作用途径可能会发生适应性代偿,对这些影响仍需进一步研究。
综上所述,临床中根据患者年龄、既往有无消化性溃疡或出血病史、有无血液系统疾病等,充分评估心血管危险因素和消化系统对抗血小板治疗的耐受性后,对需要使用PPI的心血管事件高危患者,应当避免使用奥美拉唑和雷贝拉唑,可选择泮托拉唑、埃索美拉唑及兰索拉唑。同时,对所有接受PPI联合抗血小板药物治疗者,都须进行心血管事件监测,以便及早发现、积极处理。
[1]KUSHNER F G,HAND M,SMITH S C,et al.2009 focused updates:ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction(updating the 2004 guideline and 2007 focused update)and ACC/AHA/SCAI guidelines on percutaneous coronary intervention(updating the 2005 guideline and 2007 focused update):a report of the A-merican College of Cardiology Foundation/American Heart Association Task Force on practice guidelines[J].Catheter Cardiovasc Interv,2009,74(7):E25-68.
[2]ABRAHAM N S,HLATKY M A,ANTMAN E M,et al.ACCF/ACG/AHA 2010 expert consensus document on the concomitant use of proton pump inhibitors and thienopyridines:a focused update of the ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use[J].J Am Coll Cardiol,2010,56(24):2051-2066.
[3]KWOK C S,NIJJAR R S,LOKE Y K.Effects of proton pump inhibitors on adverse gastrointestinal events in patients receiving clopidogrel:systematic review and meta-analysis[J].Drug Saf,2011,34(1):47-57.
[4]YASU T,IKEE R,MIYASAKA Y,et al.Efficacy and safety of concomitant use of rabeprazole during dual-antiplatelet therapy with clopidogrel and aspirin after drug-eluting stent implantation:a retrospective cohort study[J].Yakugaku Zasshl,2010,130(12):1743-1750.
[5]SCHMIDT M,JOHANSEN M B,ROBERTSON D J,et al.Concomitant use of clopidogrel and proton pump inhibitors is not associated with major adverse cardiovascular events following coronary stent implantation[J].Aliment Pharmacol Ther,2012,35(1):165-174.
[6]BHATT D L,CRYER B L,CONTANT C F,et al.Clopidogrel with or without omeprazole in coronary artery disease[J].N Engl J Med,2010,363(20):1909-1917.
[7]ROSSINI R,CAPODANNO D,MUSUMECI G,et al.Safety of clopidogrel and proton pump inhibitors in patients undergoing drug-eluting stent implantation[J].Coron Artery Dis,2011,22(3):199-205.
[8]AIHARA H,SATO A,TAKEYASU N,et al.Effect of individual proton pump inhibitors on cardiovascular events in patients treated with clopidogrel following coronary stenting:results from the Lbaraki Cardiac Assessment Study Registry[J].Catheter Cardiovasc Interv,2012,80(4):556-563.
[9]GOODMAN S G,CLARE R,PIEPER K S,et al.Association of proton pump inhibitor use on cardiovascular outcomes with clopidogrel and ticagrelor:insights from the platelet inhibition and patient outcomes trial[J].Circulation,2012,125(8):978-986.
[10]GAGLIA M A Jr,TORGUSON R,HANNA N,et al.Relation of proton pump inhibitor use after percutaneous coronary intervention with drug-eluting stents to outcomes[J].Am J Cardiol,2010,105(6):833-838.
[11]BURKARD T,KAISER C A,BRUNNER-LA ROCCA H,et al.Combined clopidogrel and proton pump inhibitor therapy is associated with higher cardiovascular event rates after percutaneous coronary intervention:a report fromthe BASKET trial[J].J Intern Med,2012,271(3):257-263.
[12]van BOXEL O S,van OIJEN M G,HAGENAARS M P,et al.Cardiovascular and gastrointestinal outcomes in clopidogrel users on proton pump inhibitors:results of a large dutch cohort study[J].Am J Gastroenterol,2010,105(11):2430-2436.
[13]HSIAO F Y,MULLINS C D,WEN Y W,et al.Relationship between cardiovascular outcomes and proton pump inhibitor use in patients receiving dual antiplatelet therapy after acute coronary syndrome[J].Pharmacoepidemiol Drug Saf,2011,20(10):1043-1049.
[14]SADA S,COSTANTINO G.The prophylactic use of a proton pump inhibitor(PPI)in patients treated with clopidogrel and aspirin for an acute coronary syndrome or placement of a coronary stent reduces the rate of upper gastrointestinal bleeding with no apparent increase in cardiovascular events[J].Intern Emerg Med,2011,6(2):159-160.
[15]O'DONOGHUE M L,BRAUNWALD E,ANTMAN E M,et al.Pharmacodynamic effect and clinical effcacy of clopidogrel and prasugrel with or without a proton-pump inhibitor:an analysis of two randomised trials[J].Lancet,2009,374(9694):989-997.
[16]ZAIRIS M N,TSIAOUSIS G Z,PATSOURAKOS N G,et al.The impact of treatment with omeprazole on the effectiveness of clopidogrel drug therapy during the first year after successful coronary stenting[J].Can J Cardiol,2010,26(2):e54-57.
[17]EVANCHAN J,DONNALLY M R,BINKLEY P,et al.Recurrence of acutemyocardial infarction in patients discharged on clopidogrel and a proton pump inhibitor after stent placement for acute myocardial infarction[J].Clin Cardiol,2010,33(3):168-171.
[18]HO P M,MADDOX T M,WANG L,et al.Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome[J].JAMA,2010,301(9):937-944.
[19]CHARLOT M,AHLEHOFF O,NORGAARD M L,et al.Proton-pump inhibitors are associated with increased cardiovascular risk independent of clopidogrel use:a nationwide cohort study[J].Ann Intern Med,2010,153(6):378-386.
[20]van BOXEL O S,van OIJEN M G,HAGENAARS M P,et al.Cardiovascular and gastrointestinal outcomes in clopidogrel users on proton pump inhibitors:results of a large Dutch cohort study[J].Am J Gastroenterol,2010,105(11):2430-2436.
[21]HO P M,MADDOX T M,WANG L,et al.Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome[J].JAMA,2009,301(9):937-944.
[22]JUURLINK D N,GOMES T,KO D T,et al.A populationbased study of the drug interaction between proton pump inhibitors and clopidogrel[J].CMAJ,2009,180(7):713-718.
[23]HSIAO F Y,TSAI Y W,HUANG W F,et al.A comparison of aspirin and clopidogrel with or without proton pump inhibitors for the secondary prevention of cardiovascular events in patients at high risk for gastrointestinal bleeding[J].Clin Ther,2009,31(9):2038-2047.
[24]SILLER-MATULA J M,JILMA B,SCHRÖR K,et al.Effect of proton pump inhibitors on clinical outcome in patients treated with clopidogrel:a systematic review and meta-analysis[J].J Thromb Haemost,2010,8(12):2624-2641.
[25]LIMA J P,BROPHY J M.The potential interaction between clopidogrel and proton pump inhibitors:a systematic review[J].BMC Med,2010,8:81.
[26]GILARD M,ARNAUD B,CORNILY J C,et al.Infuence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin:the randomized,double-blind OCLA(omeprazole clopidogrel aspirin)study[J].J Am Coll Cardiol,2008,51(3):256-260.
[27]SILLER-MATULA J M,SPIEL A O,LANG I M,et al.Effects of pantoprazole and esomeprazole on platelet inhibition by clopidogrel[J].Am Heart J,2009,157(1):148.e1-5.
[28] FERNANDO H,BASSLER N,HABERSBERGER J,et al.Randomized double-blind placebo-controlled crossover study to determine the effects of esomeprazole on inhibition of platelet function by clopidogrel[J].J Thromb Haemost,2011,9(8):1582-1589.
[29]FONTES-CARVALHO R,ALBUQUERQUE A,ARA'UJO C,et al.Omeprazole,but not pantoprazole,reduces the antiplatelet effect of clopidogrel:a randomized clinical crossover trial in patients after myocardial infarction evaluating the clopidogrel-PPIs drug interaction[J].Eur J Gastroenterol Hepatol,2011,23(5):396-404.
[30]ANGIOLILLO D J,GIBSON C M,CHENG S,et al.Differential effects of omeprazole and pantoprazole on the pharmacodynamics and pharmacokinetics of clopidogrel in healthy subjects:randomized,placebo-controlled,crossover comparison studies[J].Clin Pharmacol Ther,2011,89(1):65-74.
[31]NEUBAUER H,ENGELHARDT A,KRÜGER J C,et al.Pantoprazole does not infuence the antiplatelet effect of clopidogrel-a whole blood aggregometry study after coronary stenting[J].J Cardiovasc Pharmacol,2010,56(1):91-97.
[32]RAY W A,MURRAY K T,GRIFFN M R,et al.Outcomes with concurrent use of clopidogrel and proton-pump inhibitors:a cohort study[J].Ann Intern Med,2010,152(6):337-345.
[33]SIMON T,STEG P G,GILARD M,et al.Clinical events as a function of proton pump inhibitor use,clopidogrel use,and cytochrome P450 2C19 genotype in a large nationwide cohort of acute myocardial infarction:results from the French Registry of Acute ST-Elevation and NonST-Elevation Myocardial Infarction(FAST-MI)registry[J].Circulation,2011,123(5):474-482.
[34]KAZUI M,NISHIYA Y,ISHIZUKA T,et al.Identifcation of the human cytochrome P450 enzymes involved in the two oxidative steps in the bioactivation of clopidogrel to its pharmacologically active metabolite[J].Drug Metab Dispos,2010,38(1):92-99.
[35]CUISSET T,FRERE C,QUILICI J,et al.Comparison of omeprazole and pantoprazole infuence on a high 150-mg clopidogrel maintenance dose the PACA(Proton Pump Inhibitors And Clopidogrel Association)prospective randomized study[J].J Am Coll Cardiol,2009,54(13):1149-1153.
[36]KAZUI M,NISHIYA Y,ISHIZUKA T,et al.Identifcation of the human cytochrome P450 enzymes involved in the two oxidative steps in the bioactivation of clopidogrel to its pharma-cologically active metabolite[J].Drug Metab Dispos,2010,38(1):92-99.
[37]KIM K A,PARK P W,HONG S J,et al.The effect of CYP2C19 polymorphism on the pharmacokinetics and pharmacodynamics of clopidogrel:a possible mechanism for clopidogrel resistance[J].Clin Pharmacol Ther,2008,84(2):236-242.
[38] PARK B K.Cytochrome P450 enzymes in the heart[J].Lancet,2000,355(9208):945-946.
[39] ANDERSSON T.Pharmacokinetics,metabolism and interactions of acid pump inhibitors.Focus on omeprazole,lansoprazole and pantoprazole[J].Clin Pharmacokinet,1996,31(1):9-28.
[40]LI X Q,ANDERSSON T B,AHLSTRÖM M,et al.Comparison of inhibitory effects of the proton pump-inhibiting drugs omeprazole,esomeprazole,lansoprazole,pantoprazole,and rabeprazole on human cytochrome P450 activities[J].Drug Metab Dispos,2004,32(8):821-827.
[41]BLUME H,DONATH F,WARNKE A,et al.Pharmacokinetic drug interaction profiles of proton pump inhibitors[J].Drug Saf,2006,29(9):769-784.
[42]LIND T,RYDBERG L,KYLEBÄCK A.et al.Esomeprazole provides improved acid controlvs.omeprazole in patients with symptoms of gastrooesophageal refux disease[J].Aliment Pharmacol Ther,2000,14(7):861-867.
[43]SHI S,KLOTZ U.Proton pump inhibitors:an update of their clinical use and pharmacokinetics[J].Eur J Clin Pharmacol,2008,64:935-951.
[44]BLUME H,DONATH F,WARNKE A,et al.Pharmacokinetic drug interaction profles of proton pump inhibitors[J].Drug Saf,2006,29(9):769-784.