卵巢纤维瘤的CT表现
刘梦雨,薛华丹,金征宇
中国医学科学院 北京协和医学院 北京协和医院放射科,北京 100730
·论著·
卵巢纤维瘤的CT表现
刘梦雨,薛华丹,金征宇
中国医学科学院 北京协和医学院 北京协和医院放射科,北京 100730
目的探讨多层螺旋CT对卵巢纤维瘤的诊断价值。方法回顾性分析2004年至2010年经病理证实的9例卵巢纤维瘤的CT征象,其中3例有增强检查。两名放射科大夫对图像进行诊断。结果9例患者均表现为一侧附件区的肿块,边界清晰。按其CT表现分为3型:单纯型、变性型和合并腹水型。单纯型4例,表现为密度均匀的实性肿块,无强化,2例影像诊断为子宫肌瘤,2例诊断为卵巢来源的良性肿瘤;变性型3例,肿块边界清晰,内有圆形或不规则形低密度影,无强化,影像诊断为恶性1例、盆腔占位2例;合并腹水型2例,肿块密度均匀,无强化,1例伴有腹盆腔积液,1例伴有右侧胸腔积液、腹盆腔积液,影像诊断均为恶性肿瘤,卵巢来源可能性大。结论卵巢纤维瘤的CT表现多样化,多表现为一侧附件区边界清楚的实性肿块,无明显强化,若伴有胸腔积液和腹腔积液,则可诊断为Meigs综合征。
卵巢肿瘤;纤维瘤;体层摄影,X线计算机;Meigs综合征
ActaAcadMedSin,2012,34(2):104-108
卵巢纤维瘤是常见的卵巢性索间质肿瘤,术前经常被误诊为浆膜下子宫肌瘤、阔韧带肌瘤或不能确诊。近年来,非手术介入治疗子宫肌瘤方法的展开,使得其鉴别诊断直接影响治疗方法的选择。本文对9例病理证实的卵巢纤维瘤进行回顾性分析,旨在提高对本病的认识。
对象和方法
对象选取我院2004年4月至2010年8月经手术病理证实的卵巢纤维瘤9例,年龄27~75岁,平均55.6岁。手术病理结果均为卵巢纤维瘤。
方法对所有患者影像学表现进行回顾性分析。所有患者均于术前接受CT腹盆检查,其中3例同时行增强扫描。CT检查采用Siemens公司64层螺旋CT(Somatom Sensation 64,Forchheim,Germany),管电压120 kV,管电流200 mAs,螺距1.2,准直0.6×32×2,扫描时间10~13 s,层厚7 mm,层距7 mm。增强扫描注射非离子碘型造影剂[优维显 Ultravist(Iopromide),Bayer Schering Healthcare,Germany]90~100 ml,碘含量为300 mgI/ml,注射速度为3 ml/s,行动脉期(35 s)、门脉期(60 s)及延迟期(200 s)扫描。两名放射学专业放射诊断学医师分别读片,之后进行讨论得到统一结论后作为最终的诊断结果。两名医师阅片时并不了解患者最终的病理诊断结果, 但知道 CT检查旨在观测病变位置、大小、内部密度特征、强化特点以及观测是否伴有胸腹腔积液及淋巴结增大,并对其进行定性诊断。
结 果
临床病史9例患者中6例为体检发现盆腔内占位、2例可扪及下腹包块、1例下腹痛伴右肾积水及右侧输尿管梗阻;其中6例已绝经4~24年,平均(15.2±8.8)年。1例患者血清CA125水平升高,为75.9 U/ml(0~35 U/ml),余8例血清CA125水平均在正常范围内。
超声表现9例患者均表现为边界清楚的盆腔内低回声或无回声肿块,其中7例无血流信号、2例肿块周边少许血流信号。
CT表现9例均表现为单发盆腔肿块,其中右侧附件区6例、左侧附件区3例,直径1.2~16.0 cm,平均(8.3±5.5)cm。肿块呈圆形、卵圆形或分叶状,边界清楚、光滑。根据肿瘤内部密度以及是否合并腹腔积液,将其分为以下3种类型:(1)单纯型4例,表现为一侧附件区边界光滑的实性肿块(图1、2),密度均匀,CT值36~49 HU,注射对比剂后无明显强化及延迟强化(图3、4),其中1例(1/3)肿瘤内可见点状钙化;(2)变性型3例,肿瘤内部均可见不规则形(图5)、类圆形低密度影,实性部分CT值38~48 HU,注射对比剂后肿瘤实性成分无明显强化,其内低密度区无强化(图6),其中1例(1/3)肿瘤内可见点状钙化并伴有盆腔积液(图7);(3)合并腹水型2例,病变直径均大于9 cm,密度较均匀,无明显强化,1例伴腹腔积液、盆腔积液,液体密度约8 HU,1例胸腹腔积液(图8)、盆腔积液、腹腔及盆腔可见大量游离液体,液体密度约10 HU。 9例患者盆腔及腹膜后均未见明显肿大淋巴结影。

图1 54岁,右下腹右侧附件区肿块,边界清晰,密度均匀Fig 1 CT of a 54-year-old patient shows a well-defined mass with homogeneous density in the right ovary

图2 60岁,盆腔肿物,密度较均匀,可见盆腔积液Fig 2 CT of a 60-year-old patient shows homogeneous density intrapelvic mass with pelvic effusion

图3 与图2同一患者,动脉期病变无明显强化Fig 3 In the same patient as in Fig 2, the mass shows no enhancement in the arterial phase

图4 与图2、3同一患者,延迟期病变无延迟强化Fig 4 In the same patient as in Fig 2 and 3, the mass shows no delaying enhancement

图5 69岁,盆腔巨大肿物,肿物内部可见不规则形低密度影Fig 5 CT of a 69-year-old patient shows huge intrapelvic mass with inhomogeneous hypodensity inside
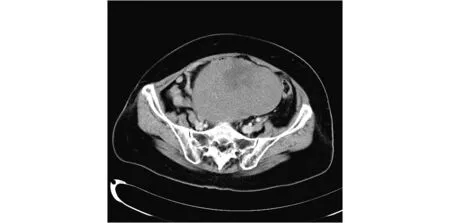
图6 与图5同一患者,注射对比剂后,肿物实性成分无明显强化,增强幅度约3HU,低密度区无强化Fig 6 In the same patient as in Fig 5, after injection of contrast medium, the solid part of the mass shows no obvious enhancement with 3HU elevated, and no enhancement of the hypodensity part of the mass is found

图7 与图5、6同一患者,肿块内可见点状钙化,并可见盆腔积液Fig 7 In the same patient as in Fig 5 and 6, the mass shows dotty calcification and pelvic effusion

图8 56岁,卵巢纤维瘤,伴有右侧胸腔积液、腹腔积液Fig 8 CT of a 56-year-old patient with ovarian fibroma shows right pleural effusion and ascites
影像诊断4例单纯型卵巢纤维瘤中,2例误诊为子宫肌瘤、2例诊断为卵巢良性病变;3例变性型卵巢纤维瘤中,1例误诊为卵巢恶性病变,2例诊断为盆腔占位,不能确定良恶性;2例合并腹水型卵巢纤维瘤均误诊为恶性肿瘤,卵巢来源可能性大。
病理表现大体观:8例卵巢增大,内见结节或团块状肿块,1例卵巢大小正常,下极附着一实性黄白色带蒂肿瘤,瘤蒂直径2cm。肿块包膜完整,质硬。切面观:表面均呈灰黄色或灰粉色。6例切面均匀一致,呈淡黄色编织状,3例切面可见肿块内部有片状水肿或囊变区。镜下观:可见形态一致的、良性梭形肿瘤细胞,肿瘤细胞排列呈束状或车辐状,核分裂像缺乏或罕见(图9)。

图9 组织病理图片,瘤体由大量束状排列的肿瘤细胞和纤维胶原基质构成(HE染色,×40)Fig 9 Photomicrograph of the histopathologic specimen shows abundant spindle-shaped cells and fibrocollagenous stroma(HE, ×40)
讨 论
卵巢纤维瘤是卵巢性索基质来源良性肿瘤,约占全部卵巢肿瘤的4%[1],无内分泌功能,多发生于中年妇女,尤其是绝经后妇女。卵巢纤维瘤多发生于一侧附件,文献报道双侧仅为4%~8%[2],本研究病例均为单侧单发。肿块生长缓慢,多在体检时偶然发现,无明显临床症状。肿瘤体积较大时,可以产生相应的压迫症状,如腹痛、泌尿系梗阻等,当肿瘤发生蒂扭转时,可发生下腹剧烈疼痛、恶心及呕吐等急腹症症状[3]。本组患者平均年龄为55.6岁,多为绝经后妇女,与文献报道基本相符[4-5],Chen等[6]报道,卵巢纤维瘤最小年龄为7月龄,可见卵巢纤维瘤的年龄分布范围很广。卵巢纤维瘤的手术切除效果好,且预后良好。
卵巢纤维瘤的CT表现多样,不同学者根据其CT表现对其进行分型。俞琳玲等[7]将其16例卵巢纤维瘤分为4种类型:单纯肿块型、变性型、合并腹水型及血管扩张型。本组病例分为3型:单纯肿块型、变性型及合并腹水型。单纯肿块型最为常见,肿块边界清晰,CT平扫密度较均匀,与子宫相比呈等密度,注入对比剂后,子宫明显强化,而肿块无明显强化;变性型包括囊变、水肿、出血及坏死。囊变、水肿及坏死表现为肿瘤内部有类圆形或片状低密度,出血于CT片表现为片状高密度影,于磁共振则表现为片状短T1信号;合并腹水型:即Meigs综合征,相对少见,易误诊为恶性病变。Meigs综合征是指伴有胸腹腔积液的卵巢有实体良性肿瘤,且手术切除后胸腹腔积液不复发。其中良性肿瘤多为纤维瘤,也可为泡膜细胞瘤、颗粒细胞瘤、良性brenner瘤等。Meigs综合征产生胸腹腔积液的原因不明,有人认为与肿瘤对腹膜的机械刺激、肿瘤对血管或淋巴管的压迫造成回流障碍等有关[8]。本组9例患者中1例有腹腔积液、盆腔积液,1例有胸腹腔积液及盆腔积液,术前均误诊为恶性病变,故了解此种类型卵巢纤维瘤的CT表现,对卵巢肿瘤的诊断有重要意义。纤维瘤多无明显强化,俞琳玲等[7]报道2例纤维瘤明显强化,且肿瘤内部伴较大斑块状钙化,将其命名为血管扩张型,此型纤维瘤国内外报道少见。
卵巢纤维瘤是附件区的良性实性肿瘤,术前做出正确的诊断,对指定治疗方案和手术方式有重要的指导意义。卵巢纤维瘤的影像表现多样,需与以下盆腔肿瘤相鉴别:当肿瘤内部密度均匀时,需与以下肿瘤相鉴别,包括子宫浆膜下肌瘤、阔韧带肌瘤及卵巢其他良性肿瘤;当肿瘤密度不均,内有坏死时需与卵巢恶性肿瘤及转移瘤相鉴别。(1)子宫浆膜下肌瘤及阔韧带肌瘤:一般情况下,子宫肌瘤血供丰富,明显强化,而卵巢纤维瘤增强后几乎不强化或轻度强化,与宫体强化呈明显反差,动态增强扫描的强化程度和强化峰值均低于子宫肌瘤[9]。(2)卵泡膜细胞瘤:卵泡膜细胞瘤与纤维瘤都属于卵巢的性索间质肿瘤,CT表现相似,但卵泡膜细胞瘤有内分泌功能,可分泌较多雌激素,临床多有内分泌紊乱的症状[10],子宫多较同龄组更为饱满,有助于鉴别。(3)卵巢恶性肿瘤:当卵巢纤维瘤较大,内有坏死或伴有胸腹腔积液时,要与恶性肿瘤进行鉴别。恶性肿瘤边界多不光整,明显强化,当伴有胸腹腔积液时,可有肠系膜、腹膜的结节状转移和腹膜后及盆腔的淋巴结明显增大等征象,有助于两者的鉴别。另外,卵巢上皮来源的恶性肿瘤多有CA125、CA19-9的升高[11],生殖细胞来源肿瘤常伴甲胎蛋白及绒毛膜促性腺激素水平的升高,均有助于鉴别。
综上,卵巢纤维瘤多发生于中年妇女,无明显内分泌改变,CT表现多为一侧附件区边界清楚的肿块,无明显强化,肿块也可伴钙化及囊变,当肿块较大时,内可有不规则低密度坏死区。当纤维瘤伴胸腹腔积液时,要考虑到Meigs综合征的可能性,此时肿瘤手术切除效果好,胸腹腔积液消失,且不复发。
[1]Kitajima K, Kaji Y, Sugimura K. Usual and unusual MRI findings of ovarian fibroma: correlation with pathologic findings [J]. Magn Reson Med Sci, 2008,7(1):43-48.
[2]Outwater EK, Wagner BJ, Mannion C, et al. Sex cord-stromal and steroid cell tumors of the ovary [J]. Radiographics, 1998,18(6):1523-1546.
[3]Chiou SY, Lev-Toaff AS, Masuda E, et al. Adnexal torsion: new clinical and imaging observations by sonography, computed tomography, and magnetic resonance imaging [J]. J Ultrasound Med, 2007,26(10):1289-1301.
[4]Leung SW, Yuen PM. Ovarian fibroma: a review on the clinical characteristics, diagnostic difficulties, and management options of 23 cases [J]. Gynecol Obstet Invest, 2006,62(1):1-6.
[5]Gargano G, De Lena M, Zito F, et al. Ovarian fibroma: our experience of 34 cases [J]. Eur J Gynaecol Oncol, 2003,24(5):429-432.
[6]Chen YJ, Hsieh CS, Eng HL, et al. Ovarian fibroma in a 7-month-old infant: a case report and review of the literature [J]. Pediatr Surg Int, 2004,20(11-12):894-897.
[7]俞琳玲, 潘芝梅, 楼芬兰. 卵巢纤维瘤CT诊断 (附16例分析) [J]. 实用放射学杂志, 2001,17(9):2.
[8]Benjapibal M, Sangkarat S, Laiwejpithaya S, et al. Meigs’ syndrome with elevated serum CA125: case report and review of the literature [J]. Case Rep Oncol, 2009,2(1):61-66.
[9]Thomassin-Naggara I, Darai E, Nassar-Slaba J, et al. Value of dynamic enhanced magnetic resonance imaging for distinguishing between ovarian fibroma and subserous uterine leiomyoma [J]. J Comput Assist Tomogr, 2007,31(2):236-242.
[10]Shanbhogue AK, Shanbhogue DK, Prasad SR, et al. Clinical syndromes associated with ovarian neoplasms: a comprehensive review [J]. Radiographics, 2010,30(4):903-919.
[11]Cecchi E, Lapi F, Vannacci A, et al. Increased levels of CA 125 and CA 19.9 serum tumour markers following cyclic combined hormone replacement therapy [J]. J Clin Pharm Ther, 2009,34(1):129-132.
CTFindingsofOvarianFibromain9Patients
LIU Meng-yu, XUE Hua-dan, JIN Zheng-yu
Department of Radiology, PUMC Hospital, CAMS and PUMC, Beijing 100730, China
JIN Zheng-yu Tel: 010-65295441, E-mail:jin_zhengyu@163.com
ObjectiveTo study the value of multislice spiral computed tomography (CT) in the diagnosis of ovarian fibroma.MethodThe CT findings of 9 cases with pathologically confirmed ovarian fibroma were retrospectively analyzed by two radiologists.ResultsAll of the 9 cases showed unilateral adnexal mass with demarcated boundary. There were three different types of ovarian fibroma according to the CT appearances: simple type(n=4), degeneration type(n=3) and the ovarian fibroma with ascites(n=2). The simple type showed homogeneous-density solid tumor with no enhancement; two of them diagnosed as uterine leiomyomas and the other two as benign tumor originated from the ovary. The degeneration type showed irregular or round hypodensity inside the tumor with no enhancement; one of them was diagnosed as malignant tumor and the other two as intrapelvic mass. The ovarian fibroma with ascites showed homogeneous density with no enhancement; one with ascites and pelvic effusion and the other one with pleural effusion, ascites and pelvic effusion, both of whom were diagnosed as malignant tumor that possibly originated from the ovary.ConclusionsThe ovarian fibroma has diverse CT findings. They often appear as a unilateral adnexal solid tumor without obvious enhancement. A diagnosis of Meigs’s syndrome may be made when it is accompanied with ascites and pleural effusion.
ovary tumor; fibroma; tomography, X-ray computed; Meigs syndrome
金征宇 电话:010-65295441,电子邮件:jin_zhengyu@163.com
R445.3
A
1000-503X(2012)02-0104-05
10.3881/j.issn.1000-503X.2012.02.002
2011-04-07)

