Heat-sensitive moxibustion attenuates the inflammation after focal cerebral ischemia/ reperfusion injury*☆
Aijiao Xiao, Rixin Chen, Mingfei Kang, Shenghai Tan
1 Basal Medical College of Jiangxi University of Traditional Chinese Medicine, Nanchang 330004, Jiangxi Province, China
2 Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine, Nanchang 330006, Jiangxi Province, China
3 Jiangxi University of Traditional Chinese Medicine, Nanchang 330004, Jiangxi Province, China
Heat-sensitive moxibustion attenuates the inflammation after focal cerebral ischemia/ reperfusion injury*☆
Aijiao Xiao1, Rixin Chen2, Mingfei Kang2, Shenghai Tan3
1Basal Medical College of Jiangxi University of Traditional Chinese Medicine, Nanchang 330004, Jiangxi Province, China
2Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine, Nanchang 330006, Jiangxi Province, China
3Jiangxi University of Traditional Chinese Medicine, Nanchang 330004, Jiangxi Province, China
Heat-sensitive moxibustion has neuroprotective effects against focal cerebral ischemia/reperfusion injury, however its mechanism of action remains unclear. In this study, rat models of focal cerebral ischemia/reperfusion injury were treated with suspended moxibustion at acupointDazhui(DU14) for 35 minutes. Results showed that suspended moxibustion decreased infarct volume, reduced cortical myeloperoxidase activity, and suppressed serum levels of proinflammatory cytokines in rats with focal cerebral ischemia/reperfusion injury. Our experimental findings indicated that heat-sensitive moxibustion can attenuate inflammation and promote repair after focal cerebral ischemia/reperfusion injury.
suspended moxibustion; heat-sensitive moxibustion; traditional suspended moxibustion; middle cerebral artery occlusion; cerebral ischemia/reperfusion injury; infarct volume; proinflammatory cytokines; interleukin; myeloperoxidase; traditional Chinese medicine; neural regeneration
Research Highlights
(1) Application of heat-sensitive moxibustion at acupointDazhui(DU14) for 35 minutes decreased infarct volume, reduced cortical myeloperoxidase activity, and suppressed serum levels of proinflammatory cytokines in rats with focal cerebral ischemia/reperfusion injury.
(2) Heat-sensitive moxibustion could attenuate focal cerebral ischemia/reperfusion injury.
Abbreviation
MCAO, middle cerebral artery occlusion
INTRODUCTlON
Suspended moxibustion, an indirect form of moxibustion, is when moxibustion is placed superficially over the skin without being in contact with it. The application of suspended moxibustion for 15 minutes is considered the stage of meridian-Qiexcitation. An extended period of suspended moxibustion may provide an effective treatment strategy, but traditional suspended moxibustion is usually ceased at this time point. The effect of traditional suspended moxibustion has recently been improved with the development of “heat-sensitive” suspended moxibustion. The most important feature of heat-sensitive moxibustion is that the duration (30–60 minutes) is longer than that of traditional suspended moxibustion(15 minutes), which is one of the reasons for its high efficiency[1-2]. Clinical practice has shown that heat-sensitive moxibustion has a positive effect on cerebral infarction[1]. Previously, our research group found that heat-sensitive moxibustion has a neuroprotective effect in a rat stroke model[3]. However, little is known about the mechanisms underlying this neuroprotective effect. Inflammation is known to be an important pathological mechanism of cerebral infarction[4]. A previous study reported that inflammatory cells and proinflammatory cytokines play an important role in the inflammatory response during cerebral infarction, and may contribute to cerebral ischemia/reperfusion injury[5]. Inflammatory cells (neutrophils and macrophages) and proinflammatory cytokines (interleukin-1β) are inflammation markers. Elangoet al[5]demonstrated that occlusion followed by reperfusion increased proinflammatory cytokines (interleukin-1β and tumor necrosis factor-α) and increased inflammatory cell activation and infiltration (using the myeloperoxidase activity assay) in the ipsilateral brain, which could result in the development of cerebral ischemia/reperfusion injury, while inhibiting myeloperoxidase activity and decreasing proinflammatory cytokine-ameliorated cerebral ischemia/reperfusion injury.
To verify whether the mechanism underlying the neuroprotective action of heat-sensitive moxibustion is associated with anti-inflammation after reperfusion, the present study measured the effects of suspended moxibustion for 35 minutes in focal cerebral ischemia/ reperfusion model rats that were induced for 2 hours by transient middle cerebral artery occlusion (MCAO), followed by 3 days of reperfusion. We monitored the cortical activity of myeloperoxidase and the serum levels of proinflammatory cytokines to explore the mechanisms underlying the neuroprotective effect of heat-sensitive moxibustion.
RESULTS
Quantitative analysis of experimental animals
A total of 36 rats were randomly divided into four groups: a sham-surgery group (n=6), a model group (n=10; MCAO modeling), a 15-minute moxibustion group (n=10; MCAO + 15-minute moxibustion), and a 35-minute moxibustion group (n=10; MCAO + 35-minute moxibustion). One rat from the model group, three rats from the 15-minute moxibustion group, and two rats from the 35-minute moxibustion group died of cerebral hemorrhage and subarachnoid hemorrhage after modeling and were excluded from the study. Therefore, in total, 30 rats were included in the final analysis.
Neurological deficit scores in rats with cerebral ischemia/reperfusion injury
To evaluate whether the model was successful, we examined neurological deficit scores after 2 hours of MCAO followed by reperfusion in rats according to Longaet al[6]. Results showed that the neurological deficit scores were 1–3 score(s) after 2 hours of MCAO followed by reperfusion (Figure 1), which suggested that the rat model of focal cerebral ischemia/reperfusion injury was successful.
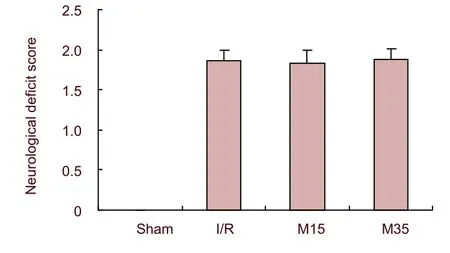
Figure 1 Neurological deficit scores in rats were evaluated after 2 hours of middle cerebral artery occlusion followed by reperfusion.
Heat-sensitive moxibustion reduced brain infarct volume
We examined infarct size after 2 hours of MCAO followed by 3-day reperfusion in rats to investigate the efficacy of 35-minute suspended moxibustion. Results revealed that moxibustion for 35 minutes significantly reduced infarct size at 3 days after reperfusion when compared with the model group (P<0.05). In contrast, the effect of traditional moxibustion for 15 minutes did not differ compared with the model group (P>0.05; Figure 2).
Heat-sensitive moxibustion decreased cortical myeloperoxidase activity
Myeloperoxidase is the most abundant enzyme in neutrophils. It is also present in monocytes, and is considered to be a primary focus of inflammatory pathologies. Myeloperoxidase assays performed on ipsilateral cortical brain samples after 3 days of reperfusion showed a significant increase in activity in the model rats compared with sham-surgery rats. Application of suspended moxibustion for 15 minutes and 35 minutes significantly decreased this activity (P<0.05; Figure 3), suggesting that brain tissue had decreased exposure to potential tissue-damaging cells, such as neutrophils or other inflammatory cells, after application of suspended moxibustion for 15 minutes and 35 minutes, particularly after moxibustion for 35 minutes.
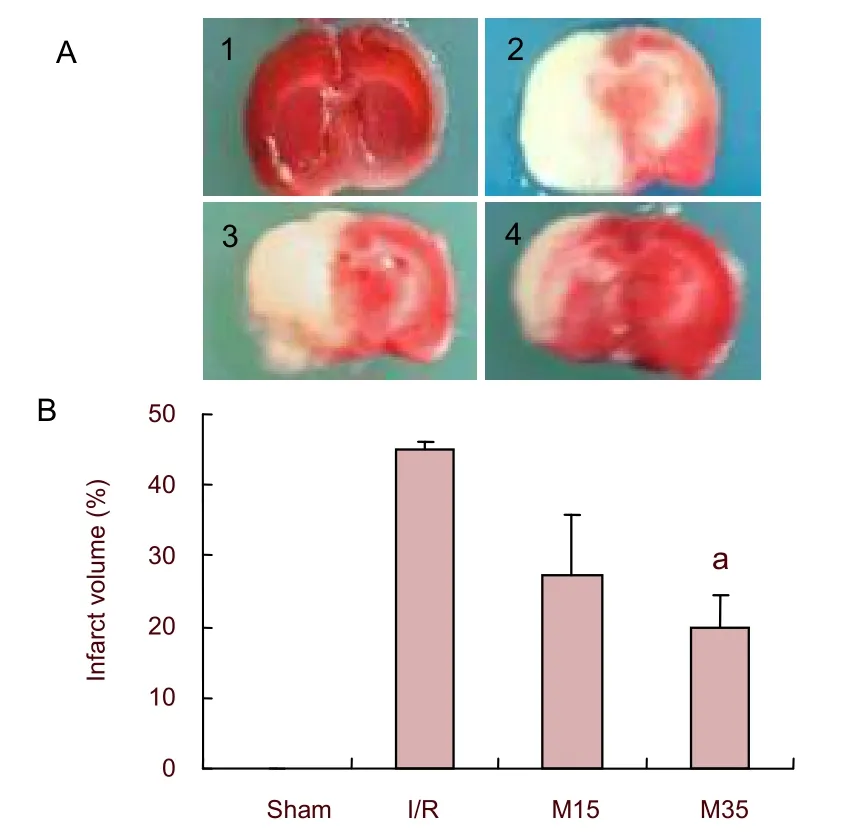
Figure 2 Effects of 35-minute suspended moxibustion on infarct volume in focal cerebral ischemia/reperfusion injury rats.
(A) Brain coronal sections were stained with 2,3,5-triphenyltetrazolium chloride; sections (1–4) represent 3 days after reperfusion. The ischemic area remained white, while the intact area stained red. 1: sham-surgery group (Sham); 2: ischemia/reperfusion injury group (I/R); 3: ischemia/reperfusion injury with 15-minute moxibustion group (M15); 4: ischemia/ reperfusion injury with 35-minute moxibustion group (M35).
(B) Infarct volume: The percentage of ischemic lesion area was calculated as the lesion area/whole brain section area. Suspended moxibustion for 35 minutes significantly protected the cerebral cortex from ischemia/reperfusion injury.aP<0.05,vs. I/R group (mean±SEM,n=6, one-way analysis of variance followed by Dunnett’s test).
Heat-sensitive moxibustion reduced the presence of inflammatory cells in the cerebral cortex
We examined brain (ipsilateral) histological structure in rats to investigate the efficacy of 35-minute suspended moxibustion. Results revealed that there were many inflammatory cells in the brain (ipsilateral) after 3 days of reperfusion in the model group when compared with sham-operated rats. However, suspended moxibustion for 15 minutes and 35 minutes significantly reduced the presence of inflammatory cells and protected the cerebral cortex from ischemia/reperfusion injury. In contrast, outcomes with 15 minutes of moxibustion were not as good as outcomes with 35 minutes of moxibustion (Figure 4).

Figure 3 Effects of 35-minute suspended moxibustion on cortical myeloperoxidase activity in focal cerebral ischemia/reperfusion injury rats.
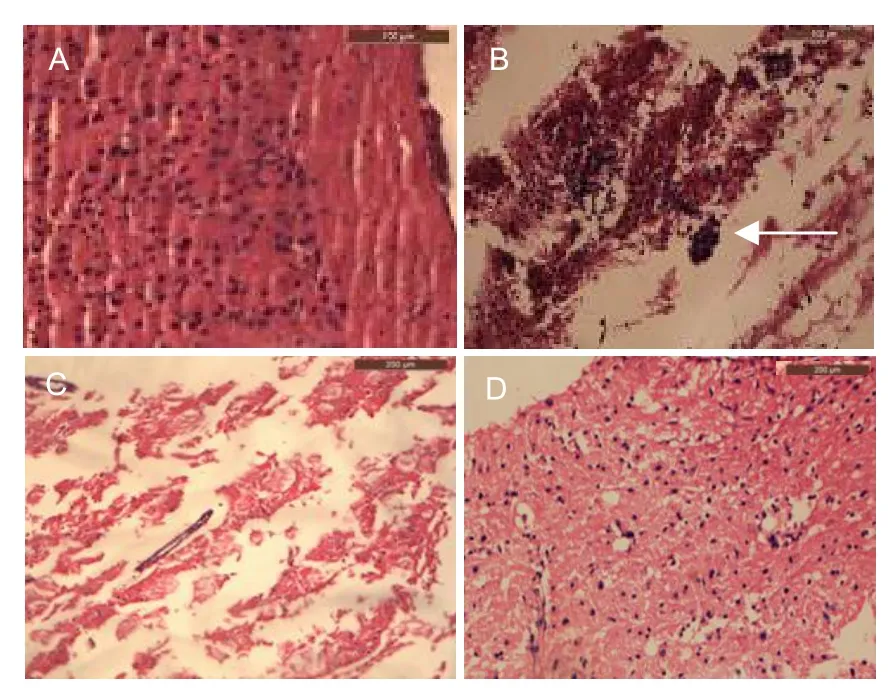
Figure 4 Effects of 35-minute suspended moxibustion on brain histological structure in rats following 3 days of focal cerebral-ischemia/reperfusion injury (hematoxylin-eosin staining).
Heat-sensitive moxibustion decreased interleukin-1β and interleukin-2 levels in serum
Both interleukin-1β and interleukin-2 are proinflammatory mediators. Our results found interleukin-1β and interleukin-2 levels to be higher in serum after 3 days of reperfusion in model rats (P>0.05) compared with sham-operated rats. However, suspended moxibustion atDazhuifor 15 minutes and 35 minutes significantly decreased interleukin-1β and interleukin-2 levels (P<0.05; Figure 5), possibly as a result of the reduced presence of inflammatory cells in the brain.
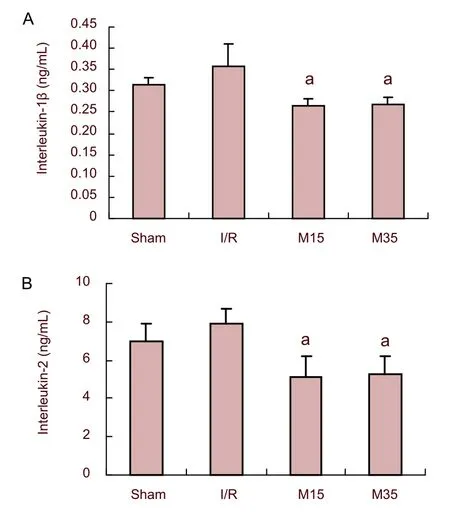
Figure 5 Effects of 35-minute suspended moxibustion on serum levels of interleukin-1β and interleukin-2 in focal cerebral ischemia/reperfusion injured rats.
DISCUSSION
The traditional duration of a moxibustion treatment is 15 minutes, and is targeted to fixed acupoints. Although some randomized, controlled trials confirmed the efficiency of traditional moxibustion[7-8], strong evidence for the therapeutic effectiveness is currently lacking. However, there is a substantial difference in treatment time between traditional moxibustion and heat-sensitive moxibustion. Previously, clinical practices and animal experiments have shown that moxibustion duration is critical for improving the efficacy of moxibustion[1,3]. Because moxibustion duration is an important factor affecting the efficacy of moxibustion, the duration of heat-sensitive moxibustion treatment is often longer than that of traditional moxibustion[1]. Therefore, this experiment employed a 35-minute moxibustion treatment period, representing the heat-sensitive moxibustion time, and applied 15 minutes as the traditional moxibustion time. The present data revealed that the application of suspended moxibustion for 35 minutes significantly reduced the infarction area at three days after reperfusion. In addition, suspended moxibustion for 15 minutes did not significantly reduce the infarct area when compared with the ischemia control group. These results suggest that prolonging the duration of moxibustion for 35 minutes improves its efficacy.
The pathological mechanism of ischemic cerebral injury is extremely complicated, involving inflammation, disruption of cellular metabolism in the brain, excitatory amino acid toxicity, intracellular calcium overload, oxidative stress injury and nerve cell apoptosis[9]. Inflammation plays a key role in ischemic injury[10], and inflammatory cells and proinflammatory cytokines are the main markers of inflammatory reactions. Here, we used the MCAO-induced cerebral ischemia/reperfusion injury model to study the inflammatory response that occurs during ischemia/reperfusion in the model group and suspended moxibustion group.
Myeloperoxidase, abundantly present in inflammatory cells (such as neutrophils and monocytes), produces hypochlorous acid from hydrogen peroxide and chloride ions during the respiratory burst of neutrophils (abundance of reactive oxygen species). Hypochlorous acid is highly cytotoxic and has been demonstrated to damage central nervous system tissue during inflammation[11]. Furthermore, the myeloperoxidase activity assay has been successfully used to confirm inflammatory cell activation and recruitment in the brain after MCAO[12]. We performed this assay to establish a relationship between the neuroprotective effect of heat-sensitive moxibustion and its anti-inflammatory properties in MCAO-induced brain ischemia/reperfusion injury (cortex) after three days of reperfusion. As expected, there was a significant increase in myeloperoxidase activity in brain of model group rats (ipsilateral cortex) when compared with the sham-surgery group. Suspended moxibustion for 35 minutes was able to reduce this activity. This indicates that there was significant suppression of inflammatory cell activation and recruitment leading to less tissue damage. We further performed hematoxylin eosin staining on brain tissue and found that after three days of reperfusion in the ipsilateral cortex of the ischemic side, a great deal of inflammatory cells were present in model group brain sections compared with the sham-surgery group, and a significant decrease of inflammatory cells in brain sections from the suspended moxibustion for the 15-minute group or suspended moxibustion for the 35-minute group. Hematoxylin eosin staining also showed that fewer nerve cells experienced necrosis in the suspended moxibustion for the 35-minute group compared with the model or suspended moxibustion for the 15-minute group.
Interleukin-1β is produced largely by activated macrophages, endothelial cells, and by vascular smooth muscle cells[13]. However, interleukin-1β can be released from microglial cells[5]. Interleukin-1β actively participates in the regulation of vascular cell functions, including the stimulation of leukocyte adhesion to endothelial cells, permeability of vessels, matrix metalloprotease production and suppression of vascular contractility[14]. It is clear that interleukin-1β levels increase during cerebral ischemia/reperfusion injury[5]. In our model, interleukin-1β was induced after three days of reperfusion in the serum of model rats, and suspended moxibustion for 15 minutes or suspended moxibustion for 35 minutes significantly decreased this induction.
Interleukin-2, a type of cytokine immune system signaling molecule, has a central role in the development of cell-mediated immunity and also serves as a key factor in the induction of a complex network of cytokines[15]. Mazzoneet al[16]showed that interleukin-2 levels increased in patients with coronary artery disease. In our study, the level of serum interleukin-2 was significantly higher in the model group than in the 35-minute moxibustion group.
In summary, inflammatory cells and proinflammatory cytokines exert important effects in cerebral ischemia/reperfusion injury, suggesting that inhibiting inflammatory cells and proinflammatory cytokines would be expected to have a neuroprotective effect[4,17]. Our results revealed that suspended moxibustion for 15 minutes or 35 minutes may reduce inflammation by reducing inflammatory cells, inhibiting myeloperoxidase activity and decreasing proinflammatory cytokines such as interleukin-1β and interleukin-2. However, the outcome of 35-minute moxibustion had a superior effect to that of 15-minute moxibustion.
MATERlALS AND METHODS
Design
A randomized, controlled, neurobiological experiment.
Time and setting
This experiment was performed at the Experimental Animal Center of Jiangxi University of Traditional Chinese Medicine, Jiangxi, China, from June to December 2011.
Materials
A total of 36 clean, adult, male Sprague-Dawley rats, weighing 220–280 g, were purchased from the Experimental Animal Center of Jiangxi University of Traditional Chinese Medicine, Jiangxi, China. Animals were housed under controlled conditions (07:00–19:00 lighting, five rats/cage before MCAO and one rat/cage after MCAO, 50–60% humidity, and about 25°C) with free access to water and food. All experimental procedures were in accordance with theGuidance Suggestions for the Care and Use of Laboratory Animals, formulated by the Ministry of Science and technology of China[18].
Methods
Preparation of focal cerebral ischemia/reperfusion injury rat models
The focal cerebral ischemia/reperfusion injury model was induced for 2 hours by MCAO followed by three days of reperfusion in spontaneously breathing rats. All animals were anesthetized with an intraperitoneal injection of sodium pentobarbital (3% (w/v)) at a dose of 40 mg/kg. Body temperature was maintained at 37.0±0.5°C using a heat lamp and heating pad. MCAO was achieved using the intraluminal filament method, as described previously[6], with minor modifications. Briefly, a midline neck incision was made, and the left common carotid artery, internal carotid artery and external carotid artery were isolated. The external carotid artery was ligated with 4-0 silk suture distal from the carotid bifurcation and the common carotid artery was ligated with 4-0 silk suture at the proximal end. Another 4-0 silk suture was tied loosely around the common carotid artery close to the carotid bifurcation. A piece of fishing line (Simago Fishing Tackle Company, Hangzhou, Zhejiang Province, China) 0.237 mm in diameter and 5 cm in length with a rounded tip was introduced into a small incision in the common carotid artery and gently advanced to the origin of the middle cerebral artery (20–22 mm from carotid bifurcation). The silk suture around the common carotid artery stump was tied tightly to prevent bleeding and to secure the fishing line. After 2 hours of occlusion, the fishing line was withdrawn to allow for reperfusion. Sham-surgery group rats were manipulated in the same way, but the middle cerebral artery was not occluded.
The following exclusion criteria are applied: (1) death within 72 hours after focal cerebral ischemia/reperfusion; (2) neurological severity score=0 (0 hour after focal cerebral ischemia/reperfusion).
Suspended moxibustion treatment
Dazhuipoints (region in C7–T1), considered to be important for brain function[19], were heated by suspended moxibustion using a moxibustion-cigar produced from mugwort (custom-made for use with animals, length 12 cm, diameter 0.6 cm, in the Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine, Jiangxi, China) at a height of approximately 3 cm over a hairless area of skin once a day for three days. Stimulation of moxibustion was performed the next day after reperfusion. Because the time of heat-sensitive moxibustion ranges from 30 minutes to 1 hour, which is usually longer than conventional moxibustion (usually around 15 minutes), this study used a duration of at least 35 minutes as the treatment time and 15 minutes as the control treatment time.
Neurological deficits scores
Neurological assessment was performed according to Longaet al[6]at 0 hour after reperfusion by an investigator who was blinded to the experimental groups, using a five-point scale: a score of 0 indicated no neurologic deficit, a score of 1 (failure to extend right forepaw fully) indicated a mild focal neurologic deficit, a score of 2 (circling to the right) indicated a moderate focal neurologic deficit, and a score of 3 (falling to the right) indicated a severe focal deficit; rats with a score of 4 did not walk spontaneously and had a depressed level of consciousness. Neurological deficit scores were graded on a scale of 0 to 4 (normal score, 0; maximal deficit score, 4).
Infarct volumes of the brain
At 3 days of reperfusion, animals were anesthetized with an intraperitoneal injection of sodium pentobarbital 3% (w/v) at a dose of 40 mg/kg, and the brains were removed after withdrawing blood. Brains were cut into 2-mm thick coronal slices at the optic chiasm level which was the coronal level at which the largest ischemic infarct was observed[20-21]. These slices were incubated for 30 minutes in 1% (w/v) 2,3,5-triphenyltetrazolium chloride and fixed in 10% (v/v) formalin. The stained slices were photographed using a Nikon COOLPIX L1 camera (Nikon, Tokyo, Japan) and measured for the ischemic lesion using INFINITY ANALYZE software (Lumenera Corporation, Ottawa, ON, Canada). The largest ischemic lesion in the brain was measured. The ischemic lesion percentage of each slice was calculated by the ratio of the infarct area to the whole slice area.
Myeloperoxidase activity in the cerebral cortex
Cerebral cortical tissue was obtained after 3 days of reperfusion. The tissue samples were homogenized and myeloperoxidase activity was performed by colorimetry according to the manufacturer’s protocol using a kit from Nanjing Jiancheng Bioengineering Institute (Nanjing, China).
Brain histological structures
After 2,3,5-triphenyltetrazolium chloride staining and lesion area analysis, the slices were embedded with paraffin. A series of adjacent 5-μm thick sections were cut in the coronal plane and stained with hematoxylin eosin. These sections were photographed with the use of image analysis system (Leica 2000 microscope, LAS V3.7 software).
Concentration of interleukin-1β and interleukin-2 in serum
We withdrew blood from the abdominal aorta at 3 days after reperfusion after rats were anesthetized with an intraperitoneal injection of sodium pentobarbital 3% (w/v)) at a dose of 40 mg/kg. The blood was centrifuged at a speed of 3 000 r/min to collect the serum. Levels of serum interleukin-1β and interleukin-2 were determined using the radioimmunoassay kit from Beijing Sino-UKInstitute of Biological Technology (Beijing, China). The manufacturer’s protocol was followed to calculate the concentration of interleukin-1β and interleukin-2.
Statistical analysis
SPSS 10.0 software (SPSS, Chicago, IL, USA) was employed for statistical analysis. Quantitative data were expressed as mean±SEM and analyzed using one-way analyses of variance followed by Dunnett’s test. A value ofP<0.05 was considered statistically significant.
Funding:This study was supported by the National Natural Science Foundation of China, No. 81060305.
Author contributions:Aijiao Xiao participated in the experimental operation, data collection, statistical analysis, and writing the paper. Rixin Chen supervised the project and provided critical comments on the manuscript. Mingfei Kang provided study guidance and coordinated the study. Shenghai Tan performed the neurological assessment and moxibustion treatment. All authors read and approved the final manuscript.
Conflicts of interest:None declared.
Author statements:The manuscript is original, has not been submitted to or is not under consideration by another publication, has not been previously published in any language or any form, including electronic, and contains no disclosure of confidential information or authorship/ patent application disputations.
[1] Chen RX, Chen MR, Kang MF. Practical Reading of Heat-sensitization Moxibustion. Beijing: People’s Medical Publishing House. 2009.
[2] Zhang B. Unblocking main and collateral channels originated by Chen RX. Jiangxi Zhongyiyao. 2006;1(1): 7-8.
[3] Chen RX, Lv ZM, Chen MR, et al. Stroke treatment in rats with tail temperature increase by 40-min moxibustion. Neurosci Lett. 2011;503(2):131-135.
[4] Jin HM. Pathophysiology. 7thed. Beijing: People’s Medical Publishing House. 2008.
[5] Elango C, Devaraj SN. Immunomodulatory effect of Hawthorn extract in an experimental stroke model. Neuroinflammation. 2010;7:97.
[6] Longa EZ, Weinstein PR, Carlson S, et al. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke. 1989;20(1):84-91.
[7] Rao P, Zhou L, Mao M, et al. A randomized controlled trial of acupuncture treatment of acute ischemic stroke. Zhongguo Zhenjiu. 2006;26(10):694-696.
[8] Zhang SH, Liu M, Asplund K, et al. Acupuncture for acute stroke. Cochrane Database Syst Rev. 2005;18(2): CD003317.
[9] Kao TK, Ou YC, Liao SL, et al. Opioids modulate post-ischemic progression in a rat model of stroke. Neurochem Int. 2008;52(6):1256-1265.
[10] Cuenca-López MD, Brea D, Galindo MF, et al. Inflammatory response during ischaemic processes: adhesion molecules and immunomodulation. Rev Neurol. 2010;51(1):30-40.
[11] Krasowska A, Konat GW. Vulnerability of brain tissue to inflammatory oxidant, hypochlorous acid. Brain Res. 2004;997(2):176-184.
[12] Liao SL, Kao TK, Chen WY, et al. Tetramethylpyrazine reduces ischemic brain injury in rats. Neurosci Lett. 2004;372(1-2):40-45.
[13] Galea J, Armstrong J, Galea J, et al. Interleukin-1 beta in coronary arteries of patient with ischemic heart disease. Arterioscler Thromb Vasc Biol. 1996;16(8):1000-1006.
[14] Oemar BS. Is interleukin-1 beta a triggering factor for restenosis. Cardiovasc Res. 1999;44(1):17-19.
[15] Simon AD, Yazdani S, Wang W, et al. Elevated plasma levels of interleukin-2 and soluble IL-2 receptor in ischemic heart disease. Clin Cardiol. 2001;24(3):253-256.
[16] Mazzone A, De Servi S, Vezzoli M, et al. Plasma levels of interleukin 2, 6, 10 and phenotypic characterisation of circulating T lymphocytes in ischemic heart disease. Atherosclerosis. 1999;145(2):367-374.
[17] Wang Q, Tang XN, Yenari MA. The inflammatory response in stroke. J Neuroimmunol. 2007;184(1-2):53-68.
[18] The Ministry of Science and Technology of the People’s Republic of China. Guidance Suggestions for the Care and Use of Laboratory Animals. 2006-09-13.
[19] Luo YF. Subject of Acupoint. 5thed. Shanghai: Shanghai Science and Technology Publishing House. 2000.
[20] Simpkins JW, Rajakumar G, Zhang YQ, et al. Estrogens may reduce mortality and ischemic damage caused by middle cerebral artery occlusion in the female rat. J Neurosurg. 1997;87(5):724-730.
[21] Bederson JB, Pitts LH, Germano SM, et al. Evaluation of 2,3,5-triphenyltetrazolium chloride as a stain for detection and quantification of experimental cerebral infarction in rats. Stroke. 1986;17(6):1304-1308.
10.3969/j.issn.1673-5374.2012.33.005 [http://www.crter.org/nrr-2012-qkquanwen.html]
Xiao AJ, Chen RX, Kang MF, Tan SH. Heat-sensitive moxibustion attenuates the inflammation after focal cerebral ischemia/reperfusion injury. Neural Regen Res. 2012;7(33):2600-2606.
Aijiao Xiao☆, M.D., Associate professor, Basal Medical College of Jiangxi University of Traditional Chinese Medicine, Nanchang 330004, Jiangxi Province, China
Aijiao Xiao, Basal Medical College of Jiangxi University of Traditional Chinese Medicine, Nanchang 330004, Jiangxi Province, China xaj527@163.com
2012-07-05
2012-10-07 (N20120305004/WJ)
(Edited by Cheng HY, Wang JM/Yang Y/Wang L)
- 中国神经再生研究(英文版)的其它文章
- Electroacupuncture improves neuropathic pain Adenosine, adenosine 5’-triphosphate disodium and their receptors perhaps change simultaneously☆
- Underlying mechanism of protection from hypoxic injury seen with n-butanol extract of Potentilla anserine L. in hippocampal neurons***☆
- Shuanghuanglian injection downregulates nuclear factor-kappa B expression in mice with viral encephalitis*★
- Antioxidant effects of the orientin and vitexin in Trollius chinensis Bunge in D-galactose-aged mice**★
- Acupuncture inhibits cue-induced heroin craving and brain activation**★
- Puerarin prevents high glucose-induced apoptosis of Schwann cells by inhibiting oxidative stress*★