急性肺栓塞合并血小板减少患者临床特点的回顾性研究
王武超 刘思齐 刘倩倩 朱继红


【摘要】 背景 急性肺栓塞(APE)是严重的心血管疾病,近年APE合并血小板减少患者的检出率不断增加,存在血栓和出血的双重问题,目前研究主要以成功的病例报道为主,存在一定的临床评估和治疗方案的研究缺口。目的 探讨APE合并血小板减少患者的临床特征和临床预后,为临床提供诊疗依据。方法 回顾性纳入2015年1月—2020年1月北京大学人民医院急诊科就诊的APE合并血小板减少患者21例为研究对象。将患者按照出血情况分为严重出血组(7例)和轻微/无出血组(14例);依据患者是否合并除肺动脉以外其他部位血栓将患者分为多部位血栓组(7例)和肺动脉血栓组(14例);依据患者死亡情况将患者分为死亡组(5例)和存活组(16例)。收集患者临床资料并进行组间比较。结果 本研究共纳入APE合并血小板减少患者21例,其中男7例,女14例,平均年龄(63.2±18.9)岁。分析病因,免疫性血小板减少性紫癜5例,抗磷脂抗体综合征4例,嗜酸性粒细胞增多症3例,药物相关血小板减少2例,系统性红斑狼疮2例,肿瘤相关性血小板减少2例,病因不明3例。19例患者进行抗凝治疗。肺动脉血栓组纤维蛋白原、纤维蛋白原/白蛋白比值高于多部位血栓组(P<0.05)。严重出血组男性比例、平均血小板体积低于轻微/无出血组,多部位血栓比例、中心粒细胞/淋巴细胞比值高于轻微/无出血组(P<0.05)。死亡组抗凝治疗比例、血小板计数低于生存组,心率、平均血小板体积/血小板比值、肿瘤相关血小板减少比例高于生存组(P<0.05)。结论 APE合并血小板减少患者存在多血栓事件风险,抗凝治疗有助于改善临床预后,依据血小板计数开展抗凝治疗与严重出血事件无相关性,血小板计数、血小板相关参数及其他凝血相关参数有助于血栓负荷、出血风险及临床预后的评估。
【关键词】 肺栓塞;血小板减少;预后;回顾性研究
【中图分类号】 R 563.5 【文献标识码】 A DOI:10.12114/j.issn.1007-9572.2023.0385
Clinical Characteristics of Acute Pulmonary Embolism Complicated with Thrombocytopenia:a Retrospective Study
WANG Wuchao,LIU Siqi,LIU Qianqian,ZHU Jihong*
Emergency Department,Peking University People's Hospital,Beijing 100044,China
*Corresponding author:ZHU Jihong,Chief physician;E-mail:zhujihong64@sina.com
【Abstract】 Background Acute pulmonary embolism(APE)is a serious cardiovascular disease. In recent years,there has been an increasing detection rate of patients with APE accompanied by thrombocytopenia,presenting a dual challenge of thrombosis and bleeding. Current research is mainly based on successful case reports,with a certain research gap in clinical evaluation and treatment options. Objective To explore the clinical characteristics and prognosis of APE patients complicated with thrombocytopenia,so as to provide a basis for clinical diagnosis and treatment. Methods A total of 21 patients with APE accompanied by thrombocytopenia who were admitted to the Emergency Department,Peking University People's Hospital from January 2015 to January 2020 were included as the study subjects and categorized into the severe bleeding group(n=7)and mild/no bleeding group(n=14)based on their bleeding conditions; as well as the multiple-site thrombosis group(n=7)and pulmonary artery thrombosis groups(n=14)based on the presence of thrombosis at sites other than the pulmonary artery; and into the death group(n=5)and survived group(n=16)based on their survival status. Clinical data were collected and compared between groups. Results A total of 21 APE patients with thrombocytopenia were included in this study,involving 7 males and 14 females,with an average age of (63.2±18.9) years. The etiologies included immune thrombocytopenic purpura(5 cases),antiphospholipid syndrome(4 cases),eosinophilia(3 cases),drug-related thrombocytopenia(2 cases),systemic lupus erythematosus(2 cases),cancer-associated thrombocytopenia(2 cases),and 3 cases of unknown etiology. Nineteen patients received anticoagulant therapy. Fibrinogen and fibrinogen/albumin ratios were higher in the pulmonary artery thrombosis group than in the multi-site thrombosis group(P<0.05). The proportion of males and mean platelet volume were lower in the severe bleeding group than in the mild/no bleeding group,and the proportion of multi-site thrombus and centrocyte/lymphocyte ratio were higher than the mild/no bleeding group(P<0.05). The proportion of anticoagulation therapy and platelet count in the death group were lower than those in the survival group,and the proportion of heart rate,mean platelet volume/platelet ratio,and cancer-associated thrombocytopenia were higher than those in the survival group(P<0.05). Conclusion APE patients with thrombocytopenia are at risk for multiple thrombotic events. Anticoagulant therapy contributes to improved clinical prognosis. Anticoagulation therapy based on platelet count is not significantly associated with serious bleeding events. Platelet count,platelet-related parameters,and other coagulation-related parameters contribute to the interpretation of thrombotic burden,bleeding risk,and clinical prognosis.
【Key words】 Pulmonary embolism;Thrombocytopenia;Prognosis;Retrospective studies
急性肺栓塞(acute pulmonary embolism,APE)是严重的心血管疾病,年发病率为39/10万~115/10万[1-3],每年可能导致30万人死亡[2],随着医疗工作者对于肺栓塞认知的不断增加,CT扫描的广泛应用,肿瘤、慢性肺疾病合并APE的检出率明显增加[4],APE合并血小板减少的病例报道也屡见不鲜[5]。血小板在止血和血栓形成过程中发挥至关重要的作用,在情况下患者会出现血小板减少和血栓形成并存的情况,有研究发现免疫性血小板减少性紫癜合并静脉血栓栓塞症(venous thromboembolism,VTE)的累计发生率为2.9%[6],血液系统恶性肿瘤VTE发生率为2%~18%,其他恶性肿瘤VTE发生率为0.6%~7.8%[7],系统性红斑狼疮合并VTE的发生率为22%[8]。在面对血栓治疗和血小板减少相矛盾的情况下,临床医生需要系统、谨慎地评估患者基础疾病、血栓严重程度、出血风险及临床预后,根据患者个体情况开展抗凝治疗及提升血小板计数(PLT)[9]。APE治疗方案中,抗凝治疗是最为重要的治疗手段,有助于改善患者临床预后[4],研究证实PLT≥50×109/L时进行标准剂量抗凝治疗是安全的,在PLT<50×109/L时需要调整抗凝治疗剂量,一般情况下选择50%标准剂量或者预防剂量进行抗凝治疗[10-12],或者考虑输注血小板的同时进行标准剂量抗凝治疗[13];在PLT<25×109/L的情况下需要权衡出血与血栓的风险进行个体化抗凝治疗[14]。APE合并血小板减少存在血栓和出血的双重问题,目前研究主要以病例报道为主,存在一定的研究缺口。为更好地了解该类患者的临床特征,进行临床风险评估及治疗方案的选择,改善患者临床预后,本研究团队对2015年1月—2020年1月北京大学人民医院急诊科接诊的APE合并血小板减少病例进行了回顾性分析。
1 对象与方法
1.1 研究对象
回顾性纳入2015年1月—2020年1月北京大学人民医院急诊科就诊的APE合并血小板减少患者21例为研究对象,APE诊断及病情分级参照欧洲心脏病协会《2019年急性肺栓塞诊断和治疗指南》[1]。入选标准:(1)年龄>16岁;(2)符合APE诊断标准;(3)入院时PLT≤100×109/L。排除标准:(1)就诊时已进行相关治疗;(2)合并肝肾功能衰竭(依据Marshall提出的MODS早期脏器功能衰竭定义[15],血肌酐>200 μmol/L,血胆红素>60 μmol/L);(3)临床研究数据缺失,不足以支持本研究;(4)非医疗因素(如放弃治疗等)导致患者临床死亡。本研究已通过北京大学人民医院伦理委员会审核(批件号:2020PHB291-01),免除知情同意。
1.2 研究方法
收集患者年龄、性别、血常规、生化全项、凝血功能分析、病因、超声心动图、CT肺血管造影、院内死亡情况等临床指标。患者PLT≥50×109/L时进行常规抗凝治疗,PLT<50×109/L时进行半量低分子肝素或者肝素抗凝治疗,并进行抗血小板减少治疗(激素和/或丙种球蛋白),临床治疗5 d后复查临床指标,计算平均血小板体积/血小板比值(MPR)、中心粒细胞/淋巴细胞比值(NLR)、纤维蛋白原/白蛋白比值(FAR)。
1.3 诊断标准与分组依据
依据欧洲心脏病协会《2019年急性肺栓塞诊断和治疗指南》将简化肺栓塞严重指数(sPESI)≥1患者定义为危重患者[1]。依据国际血栓与止血协会科学与标准化委员会标准[16],除外溶血性贫血等导致血红蛋白降低的因素,严重出血定义为致命部位出血和/或出现血流动力学变化[收缩压(SBP)≤90 mmHg或降低>40 mmHg,1 mmHg=0.133 kPa]和/或血红蛋白降低≥20 g/L和/或需要输血≥2单位;轻微/无出血定义为不符合严重出血标准,将患者分为严重出血组(7例)和轻微/无出血组(14例);依据患者是否合并除肺动脉以外其他部位血栓将患者分为多部位血栓组(7例)和肺动脉血栓组(14例);依据患者死亡情况将患者分为死亡组(5例)和存活组(16例)。
1.4 统计学方法
采用SPSS 25.0统计学软件进行数据分析,符合正态分布的计量资料以(x-±s)表示,两组间比较采用独立样本t检验,不符合正态分布的计量资料以M(P25,P75)表示,两组间比较采用秩和检验;计数资料以相对数表示,组间比较采用Fisher's确切概率法。以P<0.05为差异有统计学意义。
2 结果
2.1 患者一般情况
本研究共纳入APE合并血小板减少患者21例,其中男7例、女14例,平均年龄(63.2±18.9)岁。分析患者病因:免疫性血小板减少性紫癜5例,抗磷脂抗体综合征4例,嗜酸性粒细胞增多症3例,药物相关血小板减少2例,系统性红斑狼疮2例,肿瘤相关性血小板减少2例,病因不明3例。19例患者进行抗凝治疗(12例标准剂量低分子肝素抗凝治疗,7例患者半量低分子肝素抗凝治疗或者肝素抗凝治疗)。7例患者存在多部位血栓,7例患者出现严重出血,5例患者院内死亡(包括2例未行抗凝治疗患者)。
2.2 多部位血栓组和肺动脉血栓组患者资料比较
肺动脉血栓组纤维蛋白原(FIB)、FAR高于多部位血栓组,差异有统计学意义(P<0.05);两组性别、年龄、PLT、平均血小板体积(MPV)、国际标准化比值(INR)、活化部分凝血活酶时间(APTT)、肌酐(Cr)、总胆红素(TBil)、血清白蛋白(ALB)、MPR、NLR、危重患者比例和病因比较,差异无统计学意义(P>0.05),见表1。
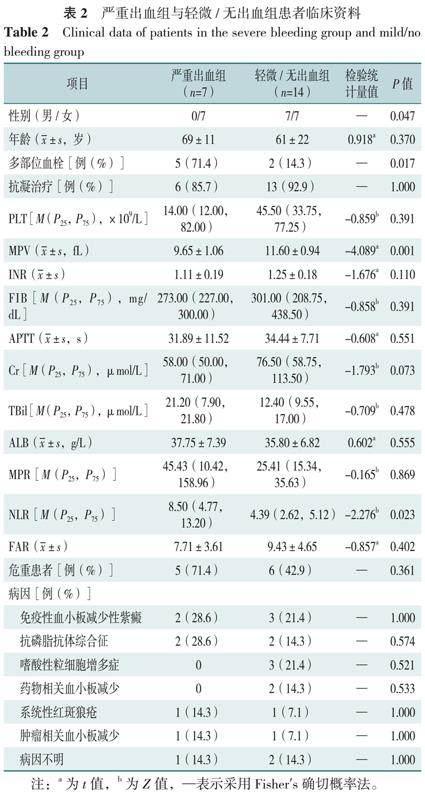
2.3 严重出血组与轻微/无出血组患者资料比较
严重出血组男性比例、MPV低于轻微/无出血组,多部位血栓比例、NLR高于轻微/无出血组,差异有统计学意义(P<0.05);两组年龄、抗凝治疗、PLT、INR、FIB、APTT、Cr、TBil、ALB、MPR、FAR、危重患者比例和病因比较,差异无统计学意义(P>0.05),见表2。
2.4 死亡组和生存组患者临床资料比较
死亡组抗凝治疗比例、PLT低于生存组,心率、MPR、肿瘤相关血小板减少比例高于生存组,差异有统计学意义(P>0.05);两组患者性别、年龄、多部位血栓占比、SBP、呼吸频率、复查血小板计数、MPV、INR、FIB、APTT、Cr、TBil、ALB、NLR、FAR、危重患者、病因比较,差异无统计学意义(P>0.05),见表3。
3 讨论
本研究发现APE合并血小板减少患者中85.7%(18/21)病因明确,考虑APE合并血小板减少患者由基础性疾病所致的可能性大,面对APE合并血小板减少的患者应该进一步查找病因。患者PLT、MPV等指标与多部位血栓事件发生无明显相关,FIB和FAR水平与多部位血栓事件发生存在相关性,多部位血栓患者FIB和FAR较低,考虑与血栓形成时血小板消耗有关。研究证实,FIB升高可以促进纤维蛋白形成,导致纤维蛋白水平升高,增加血栓强度和稳定性,增加血栓的抗溶解性[17],与心血管疾病、动脉和静脉血栓的发生有关[18-20],在疾病不同阶段,FIB可以出现动态演变,呈现先升高后降低的趋势[21],在血栓负荷过重的情况下,可能出现消耗性FIB降低[22];白蛋白可直接或间接抑制血小板和血栓的形成[23],抑制FIB活化,降低纤维蛋白聚集[24];FAR被认为是各种血栓前状态疾病(如ST段抬高型心肌梗死、慢性静脉功能不全)的标志物[23]。因此,本研究团队认为FIB与患者血栓高风险及血栓负荷相关,白蛋白存在保护性作用,FIB及FAR有助于临床医生对APE合并血小板减少患者多部位血栓事件发生的评估。
本研究发现严重出血患者女性及合并多部位血栓事件比例较高,入院时MPV较小,NLR较高,而入院时PLT、INR、APTT、FIB、抗凝治疗与患者出现严重出血表现无明显相关。研究显示MPV在一定程度上反映血小板功能情况,生理状态下MPV与PLT呈反比,以保持恒定的血小板质量,MPV增加提示大量大体积的新生血小板释放进入血液循环[25-27],研究证实MPV与止血、血栓形成相关[28],在PLT减少的患者中MPV的水平同样有助于止血情况的评估[29],MPV与血小板功能活化、炎症进程、血栓形成相关[29-32],故考虑血小板功能在一定程度上影响严重出血事件的发生。APE的严重程度与炎症状态相关[33],NLR可以作为方便获取的血常规参数以评估炎症状态,与APE的临床预后相关[34],可以影响FIB、凝血因子Ⅶ和凝血因子Ⅷ水平[35]。PLT及MPV在评估血栓和炎症反应中有着重要的作用,与炎症进程相关[30,36]。血小板与中性粒细胞协同作用,与血栓形成相关[37-39]。因此,本研究团队认为APE合并血小板减少患者严重出血风险可能与多部位血栓形成、血小板质量、炎症状态存在一定相关性,多部位血栓事件筛查、MPV、NLR等指标有助于提示严重出血事件发生的可能。本研究严重出血组与轻微/无出血组患者抗凝治疗情况无明显差异,在有效监测的情况下APE合并血小板减少患者可以进行抗凝治疗。
本研究提示肿瘤相关血小板减少及未抗凝治疗患者的院内死亡率较高,死亡组患者入院时心率较快,PLT较低、MPR较高,治疗后PLT较低。研究表明,重症患者可以出现PLT减少及MPV增高的情况,并且PLT及MPV可以作为预测ICU患者死亡风险的指标[40],MPR对疾病严重程度的评估作用已经众多研究中被证实,MPR升高可以预测严重脓毒症患者早期死亡风险,与急性心肌梗死预后情况、心肌梗死后脑卒中、VTE的发生相关[41-44],YARDAN等[45]证实MPR与APE患者右心功能和疾病的危险程度相关,MPR降低提示风险降低,本研究结果与之类似。因此,本研究团队认为APE合并血小板减少患者应当积极开展抗凝治疗,以改善患者临床预后。肿瘤相关APE合并血小板减少预后较差,监测PLT、MPR有助于进一步评估患者临床预后。
本研究存在以下局限性:本研究为单中心回顾性研究,样本量较小。单独时间点的研究可能无法全部反映患者的疾病状态,尚需进一步进行前瞻性研究。
综上所述,本研究团队认为APE合并血小板减少患者合并多部位血栓事件的比例较高,多部位血栓患者FIB及FAR水平较低,严重出血患者MPV较低,NLR较高。APE合并血小板减少患者应当积极开展抗凝治疗,院内死亡与患者多部位血栓及严重出血事件发生无明显相关。对合并相关疾病的筛查、血小板相关参数及FIB、FAR等其他凝血和炎症状态相关指标进行评估有助于对血栓发生情况、出血风险及临床预后进行预测。
作者贡献:王武超提出主要研究目标,负责研究的构思与设计,研究的实施,撰写论文;刘思齐负责数据收集、统计学分析;刘倩倩负责数据收集;朱继红负责文章的质量控制与审查,对文章整体负责,监督管理。
本文无利益冲突。
参考文献
KONSTANTINIDES S V,MEYER G,BECATTINI C,et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society(ERS)[J]. Eur Heart J,2020,41(4):543-603. DOI:10.1093/eurheartj/ehz405.
WENDELBOE A M,RASKOB G E. Global burden of thrombosis:epidemiologic aspects[J]. Circ Res,2016,118(9):1340-1347. DOI:10.1161/CIRCRESAHA.115.306841.
GARC?A-SANZ M T,PENA-?LVAREZ C,L?PEZ-LANDEIRO P,et al. Symptoms,location and prognosis of pulmonary embolism[J]. Rev Port Pneumol,2014,20(4):194-199. DOI:10.1016/j.rppneu.2013.09.006.
JIM?NEZ D,MIGUEL-D?EZ J D,GUIJARRO R,et al. Trends in the management and outcomes of acute pulmonary embolism:analysis from the RIETE registry[J]. J Am Coll Cardiol,2016,67(2):162-170. DOI:10.1016/j.jacc.2015.10.060.
DE WIT K,LINKINS L A. Challenging anticoagulation cases:a case of acute pulmonary embolism in a patient with chronic thrombocytopenia[J]. Thromb Res,2021,198:83-85. DOI:10.1016/j.thromres.2020.11.035.
SARPATWARI A,BENNETT D,LOGIE J W,et al. Thromboembolic events among adult patients with primary immune thrombocytopenia in the United Kingdom General Practice Research Database[J]. Haematologica,2010,95(7):1167-1175. DOI:10.3324/haematol.2009.018390.
KHANAL N,BOCIEK R G,CHEN B J,et al. Venous thromboembolism in patients with hematologic malignancy and thrombocytopenia[J]. Am J Hematol,2016,91(11):E468-472. DOI:10.1002/ajh.24526.
马立彬,邓刚,王鸣. 系统性红斑狼疮血栓栓塞性疾病的研究现状[J]. 中华风湿病学杂志,2010,14(9):641-644. DOI:10.3760/cma.j.issn.1007-7480.2010.09.016.
顾骋圆,王兆钺. 血小板减少患者发生血栓的机制及其治疗的研究现状[J]. 国际输血及血液学杂志,2021,44(3):185-190. DOI:10.3760/cma.j.cn511693-20200917-00209.
KHANAL N,BOCIEK R G,CHEN B J,et al. Venous thromboembolism in patients with hematologic malignancy and thrombocytopenia[J]. Am J Hematol,2016,91(11):E468-E472. DOI:10.1002/ajh.24526.
KOPOLOVIC I,LEE A Y Y,WU C. Management and outcomes of cancer-associated venous thromboembolism in patients with concomitant thrombocytopenia:a retrospective cohort study[J]. Ann Hematol,2015,94(2):329-336. DOI:10.1007/s00277-014-2198-6.
SAMUELSON BANNOW B T,LEE A,KHORANA A A,et al.
Management of cancer-associated thrombosis in patients with thrombocytopenia:guidance from the SSC of the ISTH[J]. J Thromb Haemost,2018,16(6):1246-1249. DOI:10.1111/jth.14015.
CAMPBELL P M,IPPOLITI C,PARMAR S. Safety of anticoagulation in thrombocytopenic patients with hematologic malignancies:a case series[J]. J Oncol Pharm Pract,2017,23(3):220-225. DOI:10.1177/1078155216631407.
ZANINETTI C,THIELE T. Anticoagulation in patients with platelet disorders[J]. Hamostaseologie,2021,41(2):112-119. DOI:10.1055/a-1344-7279.
MARSHALL J C,COOK D J,CHRISTOU N V,et al. Multiple organ dysfunction score:a reliable descriptor of a complex clinical outcome[J]. Crit Care Med,1995,23(10):1638-1652. DOI:10.1097/00003246-199510000-00007.
SCHULMAN S,KEARON C,Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients[J]. J Thromb Haemost,2005,3(4):692-694. DOI:10.1111/j.1538-7836.2005.01204.x.
MACHLUS K R,CARDENAS J C,CHURCH F C,et al. Causal relationship between hyperfibrinogenemia,thrombosis,and resistance to thrombolysis in mice[J]. Blood,2011,117(18):4953-4963. DOI:10.1182/blood-2010-11-316885.
KARAHAN O,ACET H,ERTA? F,et al. The relationship between fibrinogen to albumin ratio and severity of coronary artery disease in patients with STEMI[J]. Am J Emerg Med,2016,34(6):1037-1042. DOI:10.1016/j.ajem.2016.03.003.
KARAHAN O,YAVUZ C,KANKILIC N,et al. Simple blood tests as predictive markers of disease severity and clinical condition in patients with venous insufficiency[J]. Blood Coagul Fibrinolysis,2016,27(6):684-690. DOI:10.1097/MBC.0000000000000478.
GUCLU H,OZAL S A,PELITLI GURLU V,et al. Increased fibrinogen to albumin ratio in ischemic retinal vein occlusions[J]. Eur J Ophthalmol,2017,27(6):735-739. DOI:10.5301/ejo.5000942.
谢海啸,王明山,潘景业,等. 失血性休克模型中纤溶功能和抗凝血酶活性的变化研究[J]. 检验医学,2007,22(4):469-471. DOI:10.3969/j.issn.1673-8640.2007.04.031.
WADA H,MATSUMOTO T,YAMASHITA Y. Diagnosis and treatment of disseminated intravascular coagulation(DIC)according to four DIC guidelines[J]. J Intensive Care,2014,2(1):15. DOI:10.1186/2052-0492-2-15.
ACHARYA P,JAKOBLEFF W A,FOREST S J,et al. Fibrinogen albumin ratio and ischemic stroke during venoarterial extracorporeal membrane oxygenation[J]. ASAIO J,2020,66(3):277-282. DOI:10.1097/MAT.0000000000000992.
PAAR M,ROSSMANN C,NUSSHOLD C,et al. Anticoagulant action of low,physiologic,and high albumin levels in whole blood[J]. PLoS One,2017,12(8):e0182997. DOI:10.1371/journal.pone.0182997.
THOMPSON C B,JAKUBOWSKI J A. The pathophysiology and clinical relevance of platelet heterogeneity[J]. Blood,1988,72(1):1-8. DOI:10.1182/blood.v72.1.1.bloodjournal7211.
TAMELYT? E,VAI?EKAUSKIEN? G,DAGYS A,et al. Early blood biomarkers to improve sepsis/bacteremia diagnostics in pediatric emergency settings[J]. Medicina,2019,55(4):99. DOI:10.3390/medicina55040099.
尹婉宜,沈扬,张丽红. PLT、MPV、PCT与PDW在特发性血小板减少性紫癜诊断中的应用价值[J]. 中国实验诊断学,2017,21(3):420-422. DOI:10.3969/j.issn.1007-4287.2017.03.014.
CIL H,YAVUZ C,ISLAMOGLU Y,et al. Platelet count and mean platelet volume in patients with in-hospital deep venous thrombosis[J]. Clin Appl Thromb Hemost,2012,18(6):650-653. DOI:10.1177/1076029611435838.
NTOLIOS P,PAPANAS N,NENA E,et al. Mean platelet volume as a surrogate marker for platelet activation in patients with idiopathic pulmonary fibrosis[J]. Clin Appl Thromb Hemost,2016,22(4):346-350. DOI:10.1177/1076029615618023.
SCHWERTZ H,K?STER S,KAHR W H A,et al. Anucleate platelets generate progeny[J]. Blood,2010,115(18):3801-3809. DOI:10.1182/blood-2009-08-239558.
PAPANAS N,MIKHAILIDIS D P. Mean platelet volume:a predictor of mortality in diabetic and non-diabetic patients with STEMI?[J]. J Diabetes Complications,2014,28(5):581-582. DOI:10.1016/j.jdiacomp.2014.05.004.
KAMISLI O,KAMISLI S,KABLAN Y,et al. The prognostic value of an increased mean platelet volume and platelet distribution width in the early phase of cerebral venous sinus thrombosis[J]. Clin Appl Thromb Hemost,2013,19(1):29-32. DOI:10.1177/1076029612453196.
MARCHENA YGLESIAS P J,NIETO RODR?GUEZ J A,SERRANO MART?NEZ S,et al. Acute-phase reactants and markers of inflammation in venous thromboembolic disease:correlation with clinical and evolution parameters[J]. An Med Interna,2006,23(3):105-110. DOI:10.4321/s0212-71992006000300002.
WANG Q,MA J F,JIANG Z Y,et al. Prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in acute pulmonary embolism:a systematic review and meta-analysis[J]. Int Angiol,2018,37(1):4-11. DOI:10.23736/S0392-9590.17.03848-2.
BOVILL E G,BILD D E,HEISS G,et al. White blood cell counts in persons aged 65 years or more from the Cardiovascular Health Study. Correlations with baseline clinical and demographic characteristics[J]. Am J Epidemiol,1996,143(11):1107-1115. DOI:10.1093/oxfordjournals.aje.a008687.
BALTA S,DEM?RKOL S,KUCUK U. The platelet lymphocyte ratio may be useful inflammatory indicator in clinical practice[J]. Hemodial Int,2013,17(4):668-669. DOI:10.1111/hdi.12058.
SREERAMKUMAR V,ADROVER J M,BALLESTEROS I,et al. Neutrophils scan for activated platelets to initiate inflammation[J]. Science,2014,346(6214):1234-1238. DOI:10.1126/science.1256478.
LIU Z G,LI X X,ZHANG M P,et al. The role of mean platelet volume/platelet count ratio and neutrophil to lymphocyte ratio on the risk of febrile seizure[J]. Sci Rep,2018,8(1):15123. DOI:10.1038/s41598-018-33373-3.
FARAH R,NSEIR W,KAGANSKY D,et al. The role of neutrophil-lymphocyte ratio,and mean platelet volume in detecting patients with acute venous thromboembolism[J]. J Clin Lab Anal,2020,34(1):e23010. DOI:10.1002/jcla.23010.
DURAN M,ULUDA? ?. Can platelet count and mean platelet volume and red cell distribution width be used as a prognostic factor for mortality in intensive care unit?[J]. Cureus,2020,12(11):e11630. DOI:10.7759/cureus.11630.
OH G H,CHUNG S P,PARK Y S,et al. Mean platelet volume to platelet count ratio as a promising predictor of early mortality in severe sepsis[J]. Shock,2017,47(3):323-330. DOI:10.1097/SHK.0000000000000718.
BOLAT I,AKGUL O,CAKMAK H A,et al. The prognostic value of admission mean platelet volume to platelet count ratio in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention[J]. Kardiol Pol,2016,74(4):346-355. DOI:10.5603/KP.a2015.0179.
GUENANCIA C,HACHET O,STAMBOUL K,et al. Incremental predictive value of mean platelet volume/platelet count ratio in in-hospital stroke after acute myocardial infarction[J]. Platelets,2017,28(1):54-59. DOI:10.1080/09537104.2016.1203397.
HAN J S,PARK T S,CHO S Y,et al. Increased mean platelet volume and mean platelet volume/platelet count ratio in Korean patients with deep vein thrombosis[J]. Platelets,2013,24(8):590-593. DOI:10.3109/09537104.2012.748187.
YARDAN T,MERIC M,KATI C,et al. Mean platelet volume and mean platelet volume/platelet count ratio in risk stratification of pulmonary embolism[J]. Medicina,2016,52(2):110-115. DOI:10.1016/j.medici.2016.03.001.
(本文编辑:邹琳)
*通信作者:朱继红,主任医师;E-mail:zhujihong64@sina.com
引用本文:王武超,刘思齐,刘倩倩,等. 急性肺栓塞合并血小板减少患者临床特点的回顾性研究[J]. 中国全科医学,2024,27(27):3372-3377. DOI:10.12114/j.issn.1007-9572.2023.0385. [www.chinagp.net]
WANG W C,LIU S Q,LIU Q Q,et al. Clinical characteristics of acute pulmonary embolism complicated with thrombocytopenia:a retrospective study[J]. Chinese General Practice,2024,27(27):3372-3377.
? Editorial Office of Chinese General Practice. This is an open access article under the CC BY-NC-ND 4.0 license.