Insights intopostural orthostatic tachycardia syndrome afterCOVID-19 inpediatric patients
Ya-Xi Cui ·Jun-Bao Du ,2·Hong-Fang Jin
The pandemic caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) profoundly threatened human health globally and greatly impacted the world economy [1].While most patients recovered,some suff ered from chronic symptoms after the acute phase of coronavirus disease 2019 (COVID-19).The typical clinical symptoms include fatigue,exercise intolerance,dyspnea,fogginess,dizziness,headache,and tachycardia/palpitations,which are termed “post-acute COVID-19 syndrome”,“post-acute sequelae of COVID-19 (PASC)”,and “long-haul COVID”[2].The World Health Organization def nied this condition as the occurrence of symptoms in individuals with a probable or conf irmed history of SARS-CoV-2 infection,typically starting three months from the onset of COVID-19,persisting for at least two months,which is not attributable to any alternative diagnosis [3].If these symptoms coincide with abnormal tachycardia upon standing and fulf ill the diagnostic criteria for postural orthostatic tachycardia syndrome(POTS),they are referred to as “long-COVID POTS” [4 ].To diagnose pediatric POTS,there must be a sustained increase in heart rate (HR) by 40 beats per minute (bpm) or greater within the f irst ten minutes of transitioning from a lying to a standing position without the occurrence of orthostatic hypotension,and no other possible causes identif ied [5].
COVID-19 is a complex disease aff ecting multiple organ systems,with many researchers particularly focusing on its impact on the cardiovascular system,especially the prevalence of tachycardia [6].An online survey conducted to assess the prevalence of long-term COVID-19 in a sample of 2550 patients through social media revealed that a signif icant 89% of them experienced cardiopulmonary symptoms[7].POTS is a chronic form of orthostatic intolerance (OI)in pediatric and adult populations and one of the most typical PASC-related diagnoses [8].Patients with POTS have a common feature of abnormal tachycardia,which occurs as the body moves from a supine to an upright posture,accompanied by a series of discomforts such as fatigue,palpitations,dizziness,headache,chest tightness,and even syncope[9].
Recently,several case reports have documented that POTS was observed in adults and children with COVID-19 [10-16].Symptoms may progress over a few weeks to months and seriously aff ect patients’ physical quality of life and mental health [17].However,the mechanism and pathogenesis of long-COVID POTS are complex and have not yet been clarif ied.A recent study has indicated that SARS-CoV-2 infection could be one of the potential causes of POTS [10].Currently,treatment options for children and adolescents with long-COVID POTS are still based on traditional methods,including improving self-care habits,and increasing blood volume.Hence,evaluating and treating young patients with long-COVID POTS are urgent issues attracting great attention from clinicians.
Clinical evidence of long-COVID POTS in children
Although long-term COVID in adults has been reported in many studies,it remains a challenge to determine the prevalence and persistence of individual symptoms.Standardized research techniques are still lacking across different studies and the patient follow-up is insuffi cient [18].Within 6-8 months after infection,it was predicted that 2%-14% of COVID-19 survivors developed POTS [19].The UK's Offi ce for National Statistics reported an estimated prevalence of 3.4% to 15% of long-term COVID-19 in children at 4-8 weeks post-infection [20].If children exhibit symptoms related to PASC,such as headaches,fatigue,dizziness,decreased attention,abdominal pain,and tachycardia,it is advisable to conduct tests like the head-up tilt test and other autonomic nervous system examinations.The standing test is also a diagnostic procedure used to assess POTS,which monitors dynamic changes in HR and blood pressure as the child transitions from a supine to an upright standing position.The Chinese guidelines for the diagnosis and treatment of syncope in children also mention that the standing test can be used to assist in the diagnosis of POTS [21].It is important to recognize,as indicated by studies from Plash et al.[22] and Stewart et al.[23],that standing test and head-up tilt test do not give equivalent results.If these children meet the diagnostic criteria for POTS,they can be considered to have long-COVID POTS.
In contrast,there have been limited documented cases of long-COVID POTS in pediatric patients.Buchhorn et al.[12] were the f irst to report a pediatric POTS case involving a 16-year-old girl.Fourteen days after being infected with SARS-CoV-2,she began to experience dizziness and pre-syncope upon standing.During a standing test,her HR increased by more than 40 bpm.The same author subsequently reported 28 pediatric cases of dysautonomia related to COVID-19,among which 15 cases presented with inappropriate sinus tachycardia (IST) and 15 with POTS [24].Petracek et al.[13]described a 19-year-old male patient with COVID-19 who developed OI symptoms within two weeks of diagnosis.The results of his standing test were compatible with a diagnosis of POTS and the patient’s HR signif icantly increased from supine to standing by 70 bpm.Kokorelis et al.[14] reported a 16-year-old boy with signif icantly decreased exercise tolerance six weeks after infection and new-onset headache,chest pain,brain fog,dizziness,and fatigue.The standing test showed a 64 bpm rise in HR from 49 bpm in supine to 113 bpm in standing.According to the f indings of Morrow et al.[15],six out of seven pediatric patients who received standing tests exhibited OI symptoms and a change in HR greater than 30 bpm,and two of the patients experienced a change greater than 40 bpm.Drogalis-Kim et al.[16] reported that nine pediatric patients having PASC,at an average age of 14 (11-17) years,presented with persistent,debilitating dizziness for weeks to months,and f ive met the criteria for POTS as measured by the standing test.From the above case reports,it was found that children and adolescents infected with SARS-CoV-2 can experience symptoms of POTS,which may last for weeks to months (Table 1).
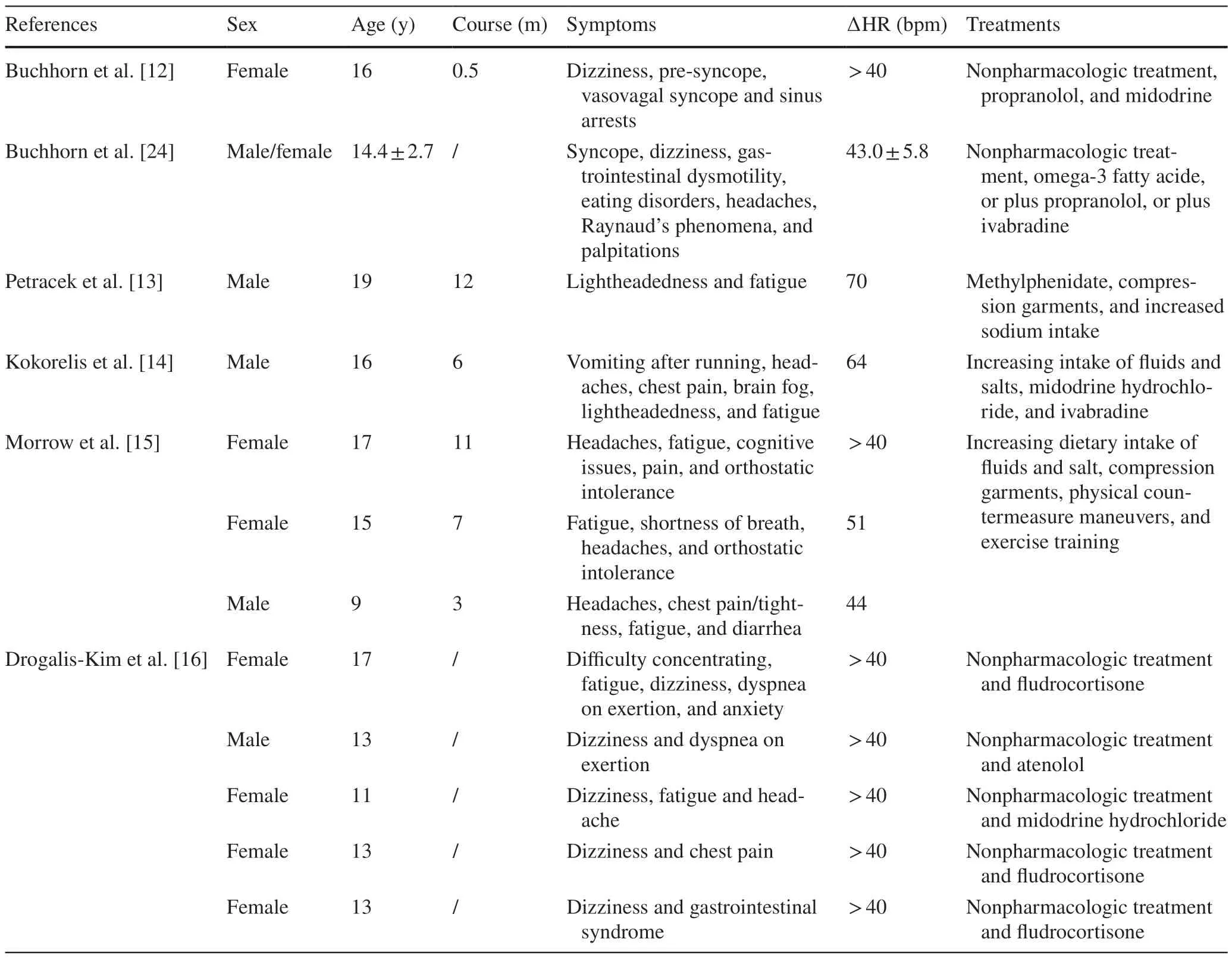
Table 1 Pediatric cases of postural orthostatic tachycardia syndrome after coronavirus disease 2019
Pathogenesis of long-COVID POTS
Autonomic dysfunction is an important pathophysiological mechanism of POTS [25].In addition,hypovolemia,imbalances in the renin-angiotensin-aldosterone system,central adrenergic hyperactivity,poor venous return,and vascular constriction disorder are also considered potential mechanisms involved in the pathogenesis of POTS [26].For example,patients with POTS may experience a reduction in stroke volume which is due to decreased systemic venous return,likely secondary to venous pooling [27].Besides the previously mentioned factors,some conditions including mast cell activation,Ehlers-Danlos syndrome,deconditioning,and gene mutations associated with the norepinephrine transporter frequently co-occur with POTS and worsen the OI symptoms [28,29].Some pediatric POTS patients are aff ected by more than one pathophysiological mechanism[18].To date,the pathogenesis of long-COVID POTS has not been clarif ied.We have summarized several pathophysiological mechanisms underlying long-COVID POTS based on the published literature.
Viral infections
Literature indicated that more than half of the patients were diagnosed with POTS after an acute viral infection,suggesting that post-viral autoimmune activation may play a role in the development of POTS [30].Yaxley et al.reported that a 17-year-old girl developed POTS complications associated with infectious mononucleosis caused by Epstein-Barr virus[31].Furthermore,Lyme disease,inf luenza virus,upper respiratory tract infections,and gastrointestinal infections can also be potential infectious triggers for the development of POTS [5,32].However,it remains to be conf irmed whether the cases of POTS that emerged after the pandemic are specif ic to COVID-19 or are simply post-viral reactions.
Post-viral neuroimmune damage
Current research has found that the coronavirus has neurotropism.Animal experiments and human brain autopsies have conf irmed the neurotropic and replicative abilities of SARS-CoV-2 [19,33].Since neurons rarely regenerate,the resulting functional impairment could be long-term sequelae,which might be the pathological basis for PASC [34].Based on the abovementioned studies,it is speculated that SARS-CoV-2 can invade the autonomic nervous system through the hematogenous or trans-neuronal route.The pre-existing or current disorders of autonomic nervous system regulation caused by acute viral infections may make patients more susceptible to POTS.Therefore,some investigators have proposed that long-COVID POTS is caused by viral infection triggering the related autonomic nervous system dysfunction [27].Buoite Stella et al.[35],using the Composite Autonomic Symptom Score 31 questionnaire,found that most post-COVID-19 patients exhibited signs of autonomic dysfunction.Additionally,Buchhorn et al.[24]discovered a reduced heart rate variability in children post-COVID-19,further suggesting the presence of autonomic dysregulation.However,it remains unclear whether this is directly caused by the impact of the virus on autonomic nerve pathways or through para-infection or post-infection immune-mediated mechanisms.Determining the most appropriate method to assess autonomic function in patients with long-COVID POTS requires attention [36].
Persistent viral presence
SARS-CoV-2 positivity in COVID-19 patients was detected for up to three months using reverse transcription polymerase chain reaction [37],and the presence of SARS-CoV-2 in the respiratory [38] and gastrointestinal tracts [39] lasted up to four months.These studies indicate that SARS-CoV-2 can persist in the body for an extended period,inducing a level of immune activation that leads to long-term infection with the virus.Doykov et al.[40] detected serum samples taken from patients who were asymptomatic or only moderately impacted by COVID-19 and found that all of the patients had a substantial remaining inf lammatory reaction.Persistent immune activation and/or inf lammation may contribute to the persistent symptoms after COVID-19.
Virus-induced microvascular damage
Wirth et al.[41] have proposed that the known microcirculatory disturbances found after COVID-19 were caused by endothelial dysfunction,microthrombus formation,and hemorheological disturbances,which would impair the function of blood vessels.Studies have shown that the level of cardiac troponin in COVID-19 patients is elevated,indicating the presence of myocardial injury,which is probably due to microvascular occlusion occurring in the myocardium [42].Autopsy studies have demonstrated this [43].The microvascular occlusion is likely due to endothelial cellular injury causing an increasing cytokine storm as well as increased platelet adherence,etc.[44,45].To compensate for vascular def icits,sympathetic hyperactivity may occur,exacerbating standing tachycardia and resulting in a vicious cycle that maintains OI symptoms [46].
Post-infectious autoimmunity
Although POTS may have several underlying mechanisms and etiologies,increasing evidence suggests that it may be related to autoimmune disease,and several autoreactive immunoglobulin G antibodies have been identif ied [47,48].When the virus enters the human body,it stimulates the body to produce some autoantibodies through molecular mimicry mechanisms,leading to autonomic nervous system dysfunction.The post-infectious autoimmunity may cause the onset of POTS [49].Patients in the recovery phase of COVID-19 may exhibit various autoantibodies after SARSCoV-2 infection,some of which might persist.Additionally,the targets of these antibodies are associated with various tissues,organs,and systems,which could lead to some of the symptoms observed in post-COVID-19 syndrome and explain the increased risks of cardiovascular complications and mortality [50].Overstimulation of the immune system during SARS-CoV-2 infection and molecular similarities between the virus and host lead to cross-reactive antibodies and autoimmune responses.The presence of antiinterferon-α2 antibodies is signif icantly associated with post-COVID-19 syndrome with respiratory symptoms,both at the initial diagnosis and 2-3 months post-infection [51].Moreover,a study reported that all surveyed COVID-19 recoverees (n=31),including those with post-COVID-19 symptoms (n=29),had at least two (up to seven) diff erent autoantibodies against G-protein-coupled receptors in their serum [52].However,these antibodies have been identif ied in POTS patients before the COVID-19 pandemic [47,48].Therefore,it is unclear whether the appearance of those antibodies is causative or a consequence of the process that causes POTS.In most patients who recover from COVID-19,the most commonly found antibodies are those with functional activity against the β2-adrenergic receptor.These antibodies have previously been reported to be associated with autonomic dysfunction,POTS,and small f iber neuropathy [53-55].
Treatment of pediatric POTS after COVID-19
It remains uncertain whether long-COVID POTS patients diff er from those with POTS unrelated to COVID-19 [4].The literature suggests that POTS often occurs after viral infections,accounting for approximately 41% of cases[56].Whether the cases of POTS that emerged after the pandemic are unique to COVID-19 or are simply post-viral reactions still requires further research to conf irm.Clarifying whether there were some unique mechanisms for long-COVID POTS holds signif icant implications for diagnosis and treatment.
Currently,there is no universally recognized treatment guideline for long-COVID POTS.Most experts recommend following the traditional treatments used for POTS patients without COVID-19.The clinical treatments of POTS include non-pharmacological and pharmacological treatments [57].Non-pharmacological treatments serve as the foundation for POTS treatment,including health education,exercise,life guidance,increasing water and salt intake,and compression garments.Fu et al.indicated that regular exercise eff ectively increased blood volume and improved physical capabilities in POTS patients [58].However,the mechanisms by which exercise improves POTS have not been clarif ied and need further studies.Pharmacological treatments include fludrocortisone,β-blockers (propranolol and metoprolol),α-receptor agonists (midodrine),selective sinus node inhibitor (ivabradine),and other drugs (paroxetine,benzodiazepine,pyridostigmine,desmopressin,and octreotide) [21,59,60].For example,Taub et al.[61] conducted a randomized clinical trial involving 22 POTS patients and found that ivabradine signif icantly improved their quality of life.Donne et al.[62] reported that the symptom improvement rate in POTS children treated with ivabradine reached up to 68%.
In Parker’s study [63],six of the seven patients did not respond to supportive care alone,and two patients failed to respond to medical therapy with ivabradine,midodrine hydrochloride,and/or metoprolol.Kokorelis et al.[14]proved that concomitant use of midodrine hydrochloride combined with ivabradine was immensely helpful in the 16-year-old patient under their care.Campen et al.[64] performed an extended observation of 29 patients affl icted with long-COVID and found that POTS symptoms disappeared after 24 months.Buchhorn et al.[24] demonstrated that treatment with omega-3 fatty acids,low-dose propranolol,and ivabradine could signif icantly reduce the standing HR in children with POTS.However,the ultimate goal of POTS treatment is to alleviate symptoms,not merely to reduce HR.It should be mentioned that a reduction in HR does not always correlate with symptomatic relief.Furthermore,individualized treatments tailored to specif ic circumstances can enhance therapeutic outcomes for patients.
Immunomodulation and therapeutic agents have not been systematically evaluated in patients with POTS.However,intravenous immunoglobulins (IVIGs) have shown potential as a possible therapeutic strategy for severe cases,particularly following COVID-19 [63].Additionally,it is advised to undergo a structured,closely monitored,and routine rehabilitation regimen for those cases.
Future prospects
At present,the duration and course of the condition varies widely among individuals,so it is still uncertain whether this is a self-limiting disease.Long-COVID POTS can lead to multiple symptoms and disabilities.In addition to physical symptoms,children and adolescents have a signif icantly high prevalence of psychological symptoms in pediatric patients with long-COVID POTS.The cooccurrence of psychological symptoms in patients with POTS needs a holistic approach to managing both physical and psychological aspects of the condition [65,66].It is imperative to establish a clear objective aimed at enhancing the comprehension of the pathophysiology of underlying long-term complications and discovering novel targets for eff ective interventions.Many studies have suggested that the pathogenesis of POTS is related to autoimmunity and thus warrants further studies on IVIG treatment [67].It is important to note that a def initive link between autoimmunity and POTS has not been conclusively established.IVIG treatment may be considered in specif ic cases where the potential benef its outweigh the risks and after careful consideration of other available treatment options.Moreover,alongside POTS,other COVID-19-related autonomic dysfunctions like IST also should be considered.Overall,in the future,investigations ought to prioritize the examination of both aspects pertinent to this recently identif ied pathological syndrome.Additionally,the scrutiny of conventional and innovative pharmacotherapeutic interventions should be pursued.
AcknowledgementsWe gratefully acknowledge all the researchers who contributed to this study.
Author contributionsCYX collected and analyzed data,drafted the initial manuscript,and revised the manuscript.DJB and JHF conceptualized and designed the study,and critically reviewed and revised the manuscript.All authors agreed to accept responsibility for this work and agreed with the f inal manuscript as submitted.
FundingThis research was funded by National High Level Hospital Clinical Research Funding (Multi-center Clinical Research Project of Peking University First Hospital;grant number: 2022CR59).
Data availabilityThe data are available from the corresponding author on reasonable request.
Declarations
Ethical approvalNot needed.
Conflict of interestNo f inancial or non-f inancial benef its have been received or will be received from any party related directly or indirectly to the subject of this article.Author Jun-Bao Du is a member of the Editorial Board forWorld Journal of Pediatrics.The paper was handled by the other editor and has undergone rigorous peer review process.Author Jun-Bao Du was not involved in the journal's review of,or decisions related to this manuscript.The authors have no conf lict of interest to declare.
 World Journal of Pediatrics2024年3期
World Journal of Pediatrics2024年3期
- World Journal of Pediatrics的其它文章
- Editors
- Information for Readers
- Instructions for Authors
- Diagnosis,treatment and prevention of severe acute respiratory syndrome coronavirus 2 infection in children: experts’ consensus statement updated for the Omicron variant
- Tribute to reviewers (January 1,2023 to December 31,2023)
- Safety and effi cacy of omalizumab for antihistamine-resistant chronic urticaria in children: a case series and literature review
