Treatment of uveitis and scleritis patients in Malaysia
Sieng Teng Seow, Iqbal Tajunisah, Fei Yee Lee, Pooi Wah Lott, Sagili Chandrasekhara Reddy
1Department of Ophthalmology, University Malaya Eye Research Centre (UMERC), Faculty of Medicine, Universiti Malaya, Kuala Lumpur 59100, Malaysia
2Clinical Research Centre, Selayang Hospital, Ministry of Health Malaysia, Selangor 68100, Malaysia
3Department of Ophthalmology, Faculty of Medicine and Defence Health, National Defence University of Malaysia,Kuala Lumpur 57000, Malaysia
Abstract
● KEYWORDS: uveitis; scleritis; ocular morbidity;blindness; aetiology
INTRODUCTION
Uveitis and scleritis are important leading causes of ocular morbidity globally[1-2], which attributes to 5%-10% of visual impairment worldwide[1,3-5].Ocular inflammation is responsible for 25% of blindness in developing countries and 5%-20% of blindness in developed countries[1,6-9].The incidence of uveitis was estimated between 17 to 52 cases per 100 000 persons per year while the prevalence was about 38 to 714 cases per 100 000 persons per year[1,10-12].Early diagnosis and timely treatment of uveitis and scleritis are imperative to reduce the risk of visual impairment[8,13].
Epidemiology of ocular inflammation is considerably diverse worldwide and various factors influence it which include host, environmental, genetic, ethnic, socioeconomic, and demographic factors[1-2,6,8,10-11,13-25].A better understanding of the demographic and causes of uveitis and scleritis in various geographic areas will prevent unnecessary laboratory testing,and the delay in commencing treatment[4].
Malaysia is a country of diversity with three large ethnic groups comprising the Malays, the Chinese and the Indians.There are numerous studies from Western and Asian countries on their epidemiology and etiology of uveitis.However,there are very few reports from our country on the causes and especially the treatment outcome of this important ocular morbidity.The present study was conducted to determine the causes and visual outcome post-treatment of uveitis and scleritis patients in a leading tertiary university hospital in Malaysia.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved by Medical Research Ethics Committee (MREC), University Malaya Medical Centre (No: 2020727-8920) as well as Malaysia National Medical Research Registry (NMRR ID-22-01261-YKU).The study was conducted in compliance with the Declaration of Helsinki and Malaysian Good Clinical Practice Guidelines.Oral informed consent was taken from each patient to allow the inclusion of their disease into study data.
In this retrospective cohort observational study, clinical records of all consecutive patients with newly diagnosed uveitis and scleritis in Ophthalmology Clinic of University Malaya Medical Centre, Kuala Lumpur, over a 4-year period from 1stJanuary 2017 until 31stDecember 2020, were reviewed and followed-up for one year.All endogenous uveitis cases including masquerades, ocular malignancies and neuroretinitis cases, were included in the study.Exogenous uveitis cases such as postoperative endophthalmitis, bleb-related, and posttraumatic including infectious keratitis, orbital inflammatory disease, and optic neuritis were excluded from the study.All patients underwent detailed history taking and comprehensive ophthalmic examination.All patients underwent visual acuity testing using Snellen acuity chart, detailed anterior segment examination with slit lamp biomicroscopy, intraocular pressure measurement by Goldmann applanation tonometry and dilated fundus examination with 90 D Volk lens.Indirect ophthalmoscopy was performed when indicated.Information regarding demographic data (age, gender, and ethnicity), as well as laterality, best corrected visual acuity at presentation,intraocular pressures, aetiology of uveitis, management,complication, and visual acuity at the end of one year were obtained from the clinical records.
The terminology and anatomical classification in this study were classified using the Standardization of Uveitis Nomenclature Working Group criteria[26].Patients were also classified based on the aetiology of uveitis whether it is idiopathic, infectious, or non-infectious.The aetiology was classified as idiopathic when there is no identifiable cause that could be identified, or when the ocular entity was unrecognizable.
Other investigations were customized according to a caseby-case basis.Ancillary ophthalmic tests, including ocular ultrasonography B scan, optical coherence tomography, visual field testing, fundus fluorescein angiography, and indocyanine green angiography were performed when needed.
The common initial investigations performed for our uveitis patients included full blood count, erythrocyte sedimentation rate, C-reactive protein, chest radiograph, Mantoux test/tuberculin skin test, Venereal Disease Research Laboratory test;Treponema pallidumhemagglutination test and enzyme-linked immunosorbent assay screens for human immunodeficiency virus.Other tests performed included autoimmune markers such as rheumatoid factor, antinuclear antibodies, anti-double stranded DNA, anti-neutrophil cytoplasmic antibody and urine biochemistry examinations (urine analysis).Laboratory tests were not performed in patients with the first episode of acute anterior uveitis that responded well to topical steroid treatment.Other specific laboratory tests ordered included human leucocyte antigen typing (HLA-B27, HLA-B51),Mycobacterium tuberculosisinterferon-γ release assays, such as QuantiFERONTB Gold assay or T-SPOT.TB assay, enzyme-linked immunosorbent assay forToxoplasmaandtoxocaraantibody,Leptospiraantibody test, and serum angiotensin-converting enzyme test.Diagnostic tests such as ocular fluid analysis(polymerase chain reaction analysis of aqueous or vitreous aspirate for genomes ofMycobacteria,herpesgroup of viruses,andToxoplasma gondii), cultured media, and cytology were performed whenever deemed necessary.
Additional radiologic investigations, such as X-ray of sacroiliac joints, lumbosacral spine to look for ankylosing spondylitis, and high-resolution computed tomography of the chest to look for pulmonary sarcoidosis were also performed in some patients.
Multidisciplinary consultations with rheumatology, infectious disease, pulmonary, oncology, dermatology, and neurology specialists were requested whenever systemic involvement was suspected.
Diagnoses such as Vogt-Koyanagi-Harada (VKH) disease,Behcet’s disease, ocular sarcoidosis, and acute retinal necrosis were made according to the standard diagnostic criteria accepted by uveitis subspecialists.Diagnosis of tuberculous related uveitis was made based on Collaborative Ocular Tuberculosis Study group recommendations.Diagnosis was made upon suggestive clinical history and signs, with at least a positive Mantoux test (>10 mm), and/or positive QuantiFERON-TB Gold assay or T-SPOT.TB assay results if a confirmatory test such as isolation ofMycobacterium tuberculosisor its DNA in ocular fluid or tissue was not available.For spondyloarthropathies, the aetiology was categorized as HLA-B27-related anterior uveitis if the clinical presentation concurs with HLA-B27-related anterior uveitis,coupled with a positive B27 confirmatory test, in the absence of other aetiologies.
Statistical AnalysisStatistical analysis was performed using Statistical Package of Social Science, version 23.0 (SPSS,Inc., Chicago, III., USA).Categorical data were presented as frequencies and percentages, while numerical data were presented as mean±standard deviation (SD) for normally distributed data and median (interquartile range, IQR) for nonnormally distributed data based on inspection of histograms.Simple and multiple logistic regression analysis were used to determine association between the visual outcomes and its variables.AP-value of <0.05 was considered statistically significant.
RESULTS
Demographic DataA total of 288 patients were recruited in this study.The mean±SD age of the population was 48.7±17.7y.Most patients were aged between 41 to 60 years old (36.1%).The youngest patient to have uveitis was a oneyear-old, whereas the oldest patient diagnosed with uveitis was 88 years old.There was a slight predominance of female gender (n=156, 54.2%).As for ethnicity, the patients were predominantly Malays (44.8%) who contributed to 129 cases,followed by the Chinese (n=83, 28.8%; Table 1).
Aetiology and Clinical PresentationTable 1 describes the clinical presentation in the study population.About half of the patients had concurrent systemic comorbidities(n=149, 51.7%), while 5.2% patients had rheumatology related diseases.The majority of patients presented with nongranulomatous type of inflammation (n=266, 92.4%), with only 22 patients (7.6%) with the granulomatous type.Anterior uveitis was the most common anatomical diagnosis (50.0%)followed by panuveitis (25.0%), scleritis (13.5%), posterior uveitis (6.9%), and intermediate uveitis (4.5%).
A large number of patients (n=119, 41.3%) had unknown or idiopathic causes for the ocular inflammation despite a thorough investigation (Table 2).In 85 (29.5%) known infectious cases,herpetic anterior uveitis was the most common cause, followed by endogenous bacterial endophthalmitis and toxoplasmosis.In non-infectious uveitis cases (n=84, 29.2%), VKH disease,sarcoidosis and HLA-B27-associated uveitis were the leading causes.Idiopathic causes were commonly seen in anterior,and intermediate uveitis, while endogenous endophthalmitis and idiopathic causes were highest for posterior uveitis.Most endogenous endophthalmitis has an identifiable organism,the most common organisms were Extended-Spectrum β-Lactamases (ESBL)Klebsiella pneumoniaefollowed by methicillin-sensitiveStaphylococcus aureus(MSSA).In 2.14% of cases of endogenous endophthalmitis, no organism was identified.
Most patients had an absence of hypopyon on presentation.Thirteen patients (n=13, 4.5%) presented with hypopyon and out of these, eight cases were infectious, four were noninfectious and one case was idiopathic in origin.
More than half of the patients had best corrected vision of the affected/worse eye at 6/12 or better (n=172, 59.7%) on presentation.Unfortunately, about 62 (21.5%) patients already had poor visual acuity of 6/60 or worse on presentation.
Type and Aetiology of ScleritisAmong the scleritis cases,anterior scleritis was more common than posterior scleritis(n=36, 92.3%vsn=3, 7.7%; Table 3).About 25.6% (n=10)of patients had an identifiable cause for the scleritis while 74.4% (n=29) had no cause found.For the identifiable cases,infectious causes and non-infectious causes had an equal distribution of (n=5, 12.8%vsn=5, 12.8%).There were two cases of surgical-induced necrotizing scleritis (SINS), that occurred post pars plana vitrectomy and cataract surgery.
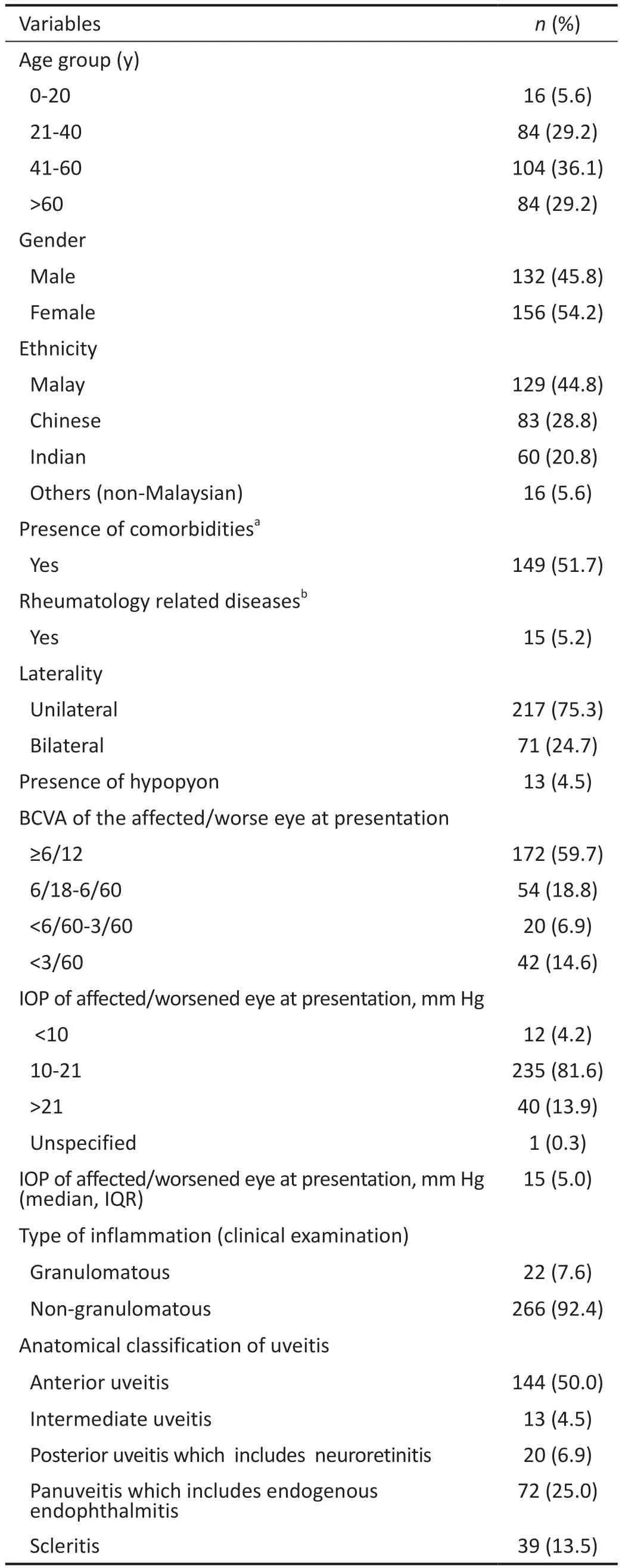
Table 1 Demographic characteristics of uveitis and scleritis patients n=288
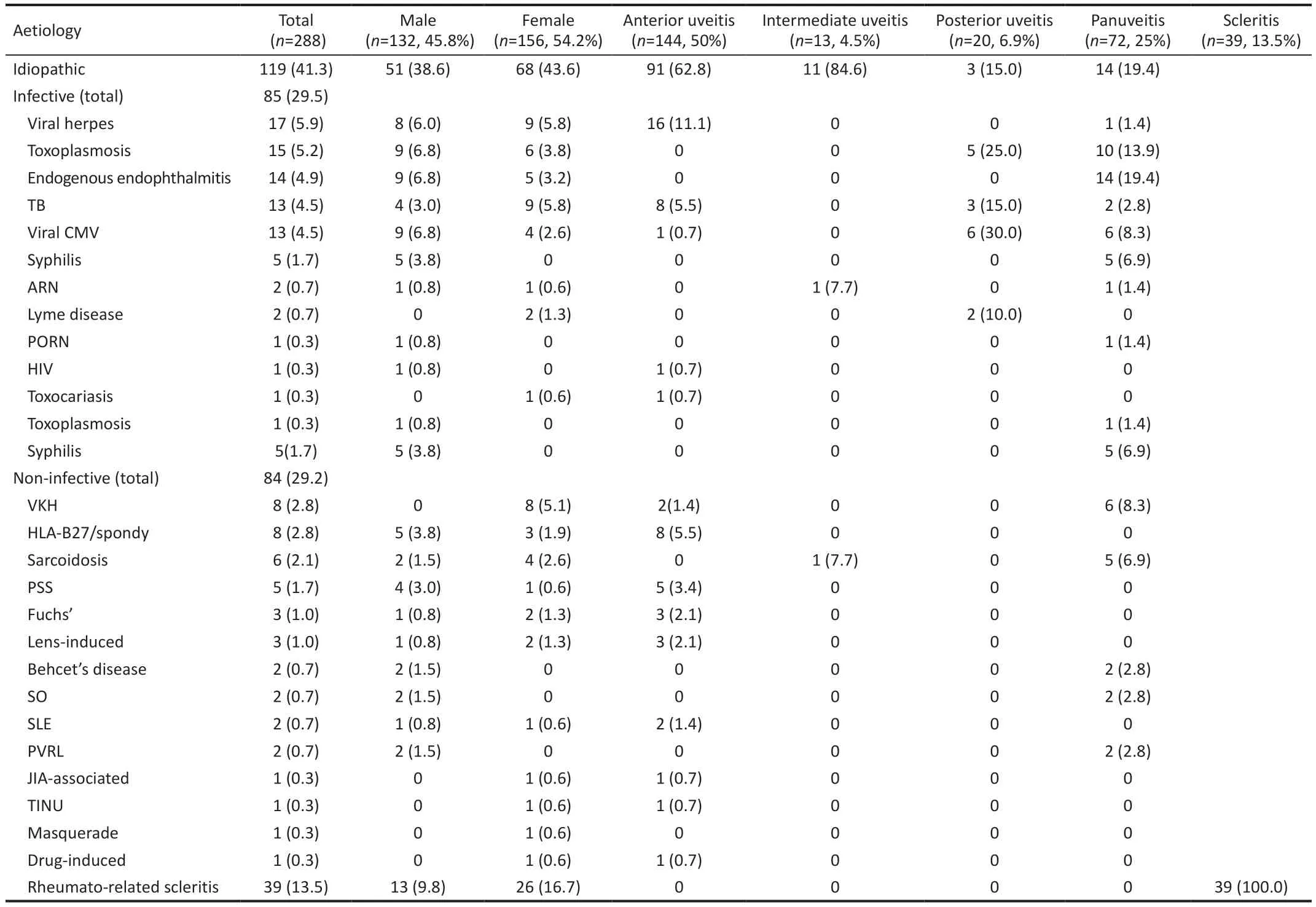
Table 2 Aetiologies according to gender and anatomical location of uveitis n (%)
Aetiologies According to Age GroupThe majority of our patients were in the productive age group ranging between 21-60 years old, accounting for 188 patients (65.3%).The older age group of beyond 60y made up 29.2% of patients,while those younger than 20y had the lowest incidence in our study (n=16, 5.6%).The incidence of toxoplasmosis and endogenous endophthalmitis were slightly higher in the older age group of more than 60y (Table 2).
Management of UveitisTable 4 shows the treatments and interventions performed in our patients.The majority of them (89.9%) were treated with topical steroids.About one quarter (24.7%) of patients required additional oral prednisolone, and 9.6% required second-line treatment with mycophenolate mofetil, methotrexate, azathioprine,cyclosporine, cyclophosphamide, or biologics.In agreement with other studies, immunosuppressive agents, as well as steroid-sparing agents, were administered to patients whose ocular inflammation was not responsive to oral prednisolone or when the side effects of systemic steroids were intolerable to the patients[26].A small group of patients (4.2%) required local steroids either in the form of intravitreal triamcinolone or dexamethasone, orbital floor triamcinolone, subconjunctival dexamethasone, or subtenon triamcinolone.About 13.9%of patients underwent ocular surgeries that included cataract extractions, pars plana vitrectomy, and glaucoma drainage procedures.
Complications of UveitisOcular complications were detected in 78 patients (27.1%); some of them had complications in both eyes (total 101 eyes).The most common complication was glaucoma (n=48, 47.5%), followed by cystoid macula oedema(n=19, 18.8%), cataract (n=14, 13.9%), posterior synechiae(n=9, 8.9%), retinal detachment (n=7, 6.9%), epiretinal membrane (n=3, 2.9%), and macular scar (n=1, 0.9%).
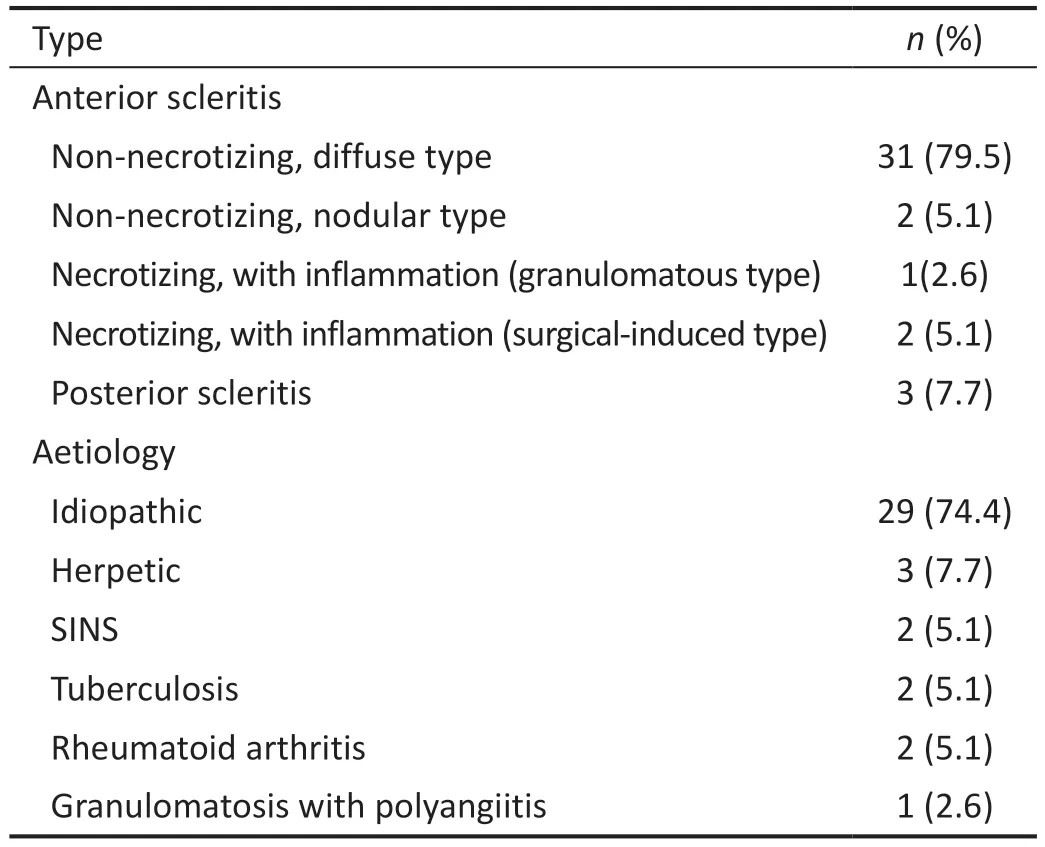
Table 3 Types and aetiology of scleritis n=39
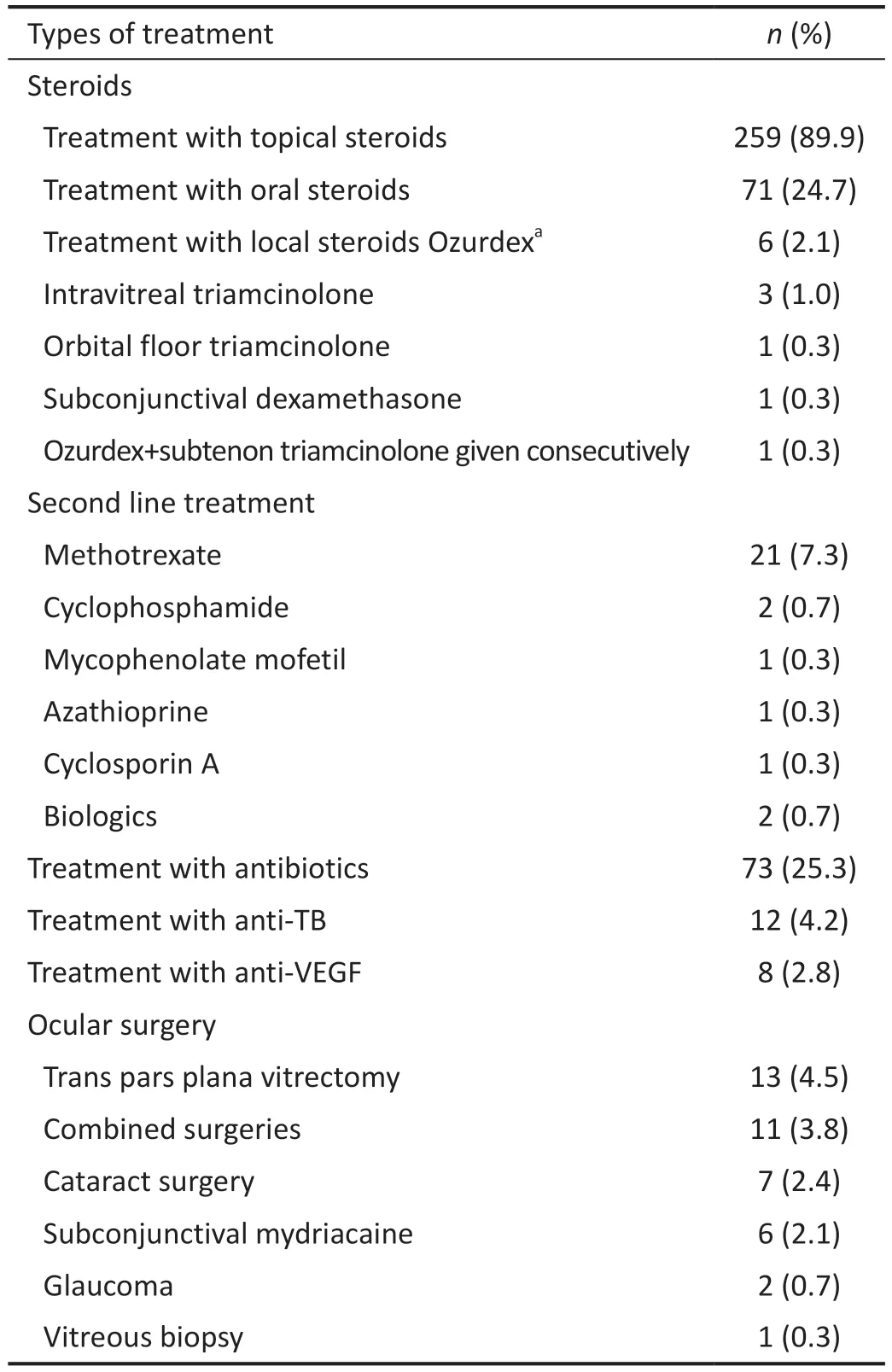
Table 4 Management of uveitis
Visual Outcome at One YearThe visual reading was recorded using the best-corrected Snellen visual acuity.Distance vision impairment was categorized according to the International Classification of Diseases—11 (Updated andRevised 2018)[27]:mild visualimpairment is defined as visual acuity worse than 6/12 to 6/18, moderate visualimpairment(visual acuity worse than 6/18 to 6/60), and severe visual impairment (visual acuity worse than 6/60 to 3/60).Blindness is defined as visual acuity of worse than 3/60, or corresponding visual field loss to less than 10 degrees, in the better eye with the best possible correction.We also recorded the vision at one year after the first presentation and treatment.Visual outcome was then categorized into good visual outcome (visual acuity of 3/60 or better) or poor (visual acuity of worse than 3/60).
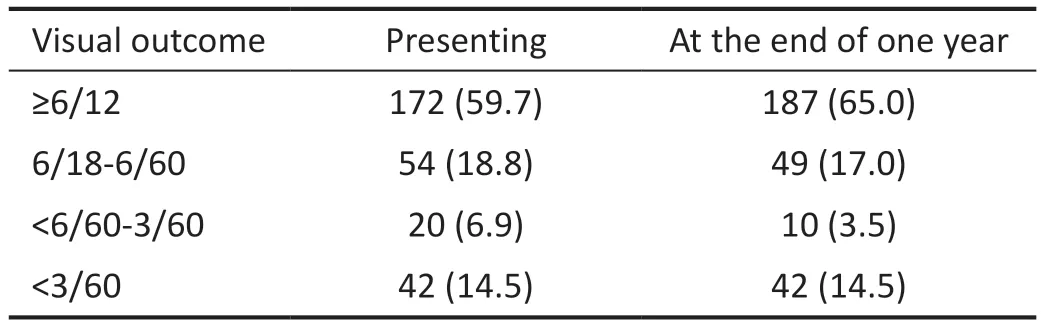
Table 5 Visual outcome of all uveitis patients at one year follow-up compared with presenting vision n (%)
The visual acuity in all uveitis patients at presentation was ≥ 6/12 in 172 (59.7%), 6/18-6/60 in 54 (18.8%), <6/60-3/60 in 20(6.9%) and <3/60 in 42 (14.5%) patients (Table 5).A total of 42 patients (14.5%) suffered from blindness at one year of follow-up.Endogenous endophthalmitis (n=12, 28.6%) was the most common reason for this.At the end of one year of follow-up, visual acuity improved in 131 patients (45.4%),remained stable in 125 (43.4%) and worsened in 32 (11.1%).
Factors of Poor Visual Outcome 5y Simple and Logistic RegressionTable 6 highlighted the factors for poor visual outcomes using simple and multiple logistic regression.Posterior uveitis and panuveitis were the types of inflammation associated with poor visual outcomes compared to the anterior uveitis type.Visual acuity of worse than 3/60 at presentation was also one of the significant prognostic factors for poor visual outcomes compared to visual acuity better than 6/12 at presentation with aP<0.001.
Other factors like age, gender, laterality, aetiology, type of inflammation, and complication were not associated with poor visual outcomes.
DISCUSSION
The present study described the causes of ocular morbidity in uveitis and scleritis patients from a leading tertiary hospital in Malaysia.The mean age of presentation in our study was 48.7y which appeared to be older than the approximate 40y reported previously[1,3].Patients younger than 20y only contributed to 5.6% of our study population as our centre is not the main paediatric referral centre for the country.Contrary to other South-East Asian countries, there was a slight female preponderance in our study that was similar to Philippines[28]whereas males were more commonly affected in Vietnam[17],Thailand[29], and Singapore[30].More female preponderance wasalso seen in other studies in Asian and Western countries like China, Italy, India, Japan, and United Kingdom(Table 7)[5,7,14,17-18,22-23,28-35].

Table 6 Factors affecting poor visual outcomes despite treatment (simple and multiple logistic regression)
Anterior uveitis was the most common anatomical type of uveitis (50.0%), followed by panuveitis (25.0%), scleritis(13.5%), posterior uveitis (6.9%), and intermediate uveitis(4.5%) in our study.Many related works of literature supported that anterior uveitis was the predominant form of uveitis similar to our study, except for Singapore[30]where intermediate uveitis is the commonest, and China[14]and Japan[32]where panuveitis predominated (Table 8)[2,5,7,14,17-18,22-24,28-32,35-38].
The comparison with other countries for the pattern of uveitis in different regions of the world is shown in Tables 7 and 8.
In our study, most cases were unilateral and non-granulomatous.Unilateral uveitis constituted 75.3% of patients while bilateral uveitis was seen in 24.7% of patients.Most previously reported uveitis cases were unilateral in origin similar to our study,except for China[14], India[31], and United Kingdom[22]where bilateral involvement was more common (Table 8).More than half of patients (59.7%) presented with a good visual acuity;better than 6/12 in the affected or the worse affected eye.This could probably be attributed to the large proportion of our study population presenting with the anterior type of uveitis with lesser degree of complications.
Most of the previously reported studies had a specific diagnosis either infective or non-infective aetiology for the uveitis cases,which is similar to our study.Exceptions were noted for uveitiscases in the Philippines[28], Nepal[37], and Sri Lanka[5]in which more than half of the cases were idiopathic.One possibility of such observation is the limited availability of various diagnostic investigations in low economic countries that might have limited their diagnostic ability.In our study, we had a nearly equal distribution of infectious and non-infectious causes (n=85,29.5%vsn=84, 29.2%) as compared to most Asian countries,except in the Philippines[28]and India[31].This was in contrast with Western countries such as Greece[36]where non-infectious causes are more common compared to infectious causes.VKH, HLA-B27 uveitis, and sarcoidosis were the most common identifiable non-infective aetiology from our study findings, which was similar to most Asian countries like Singapore, Japan, Vietnam, Philippines, China, and Bangladesh.These findings were different from the Western countries such as Italy[18]and United Kingdom[22]where the most common non-infective aetiology was reported to be Fuch heterochromic uveitis (Table 8).A high frequency of VKH has been reported in the Asian population; however,it constitutes a rare aetiology of uveitis in most Western countries.Behcet’s disease was relatively uncommon in our study when compared to Jordan[34]and this could be because our country’s geographical location is not along the ancient silk route.It is noteworthy that contrary to other published studies, aetiologies such as Birdshot chorioretinopathy,onchocerciasis, toxocariasis, Lyme disease, and presumed ocular histoplasmosis syndrome (POHS) were not seen in our population.It is well-known that the aetiology for uveitis varied depending upon epidemiology, geographical, climate variation, and disease dissemination, hence some diseases are not frequently encountered in our part of the world[13-25].
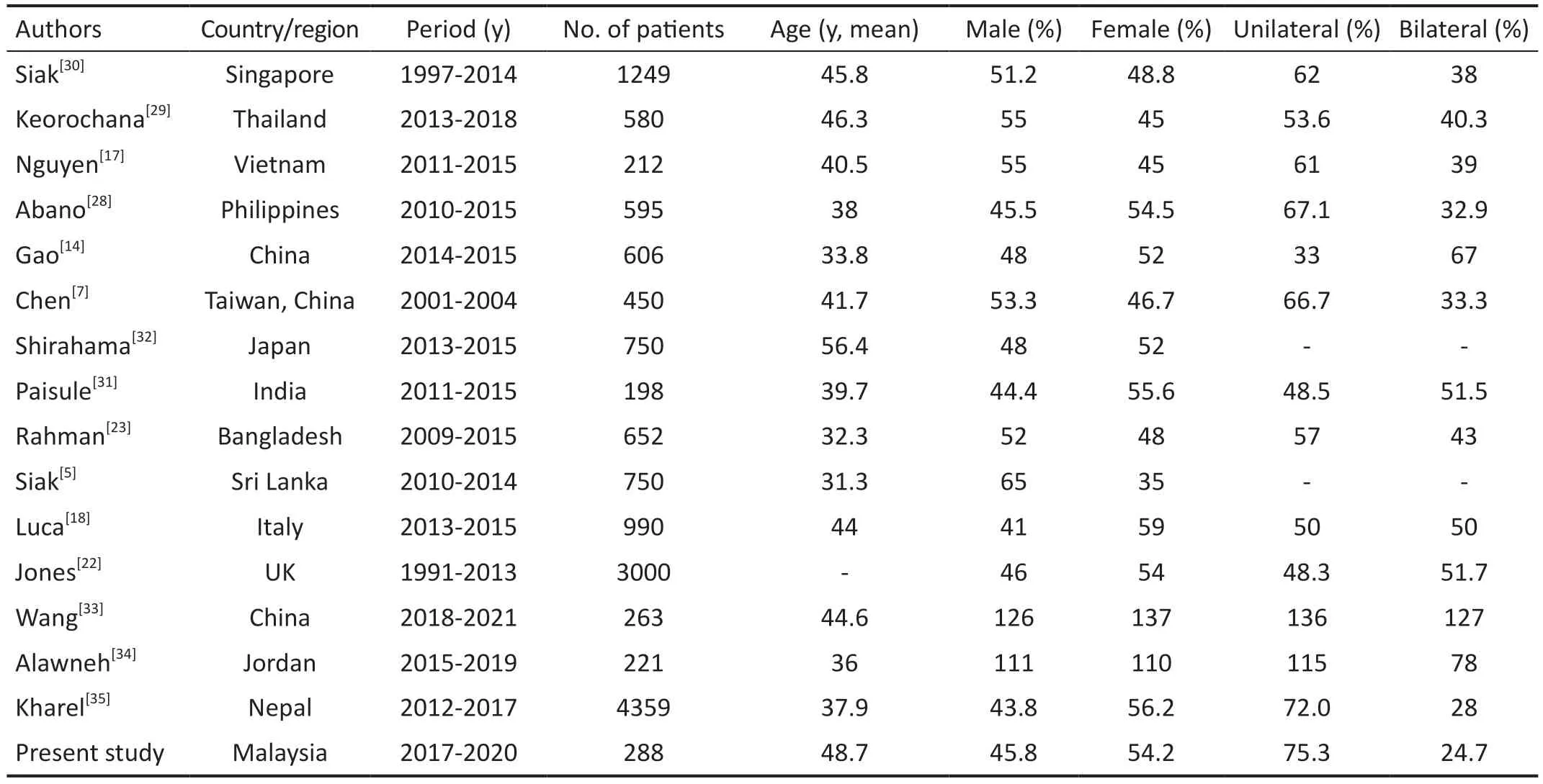
Table 7 Comparison of uveitis: demographic data
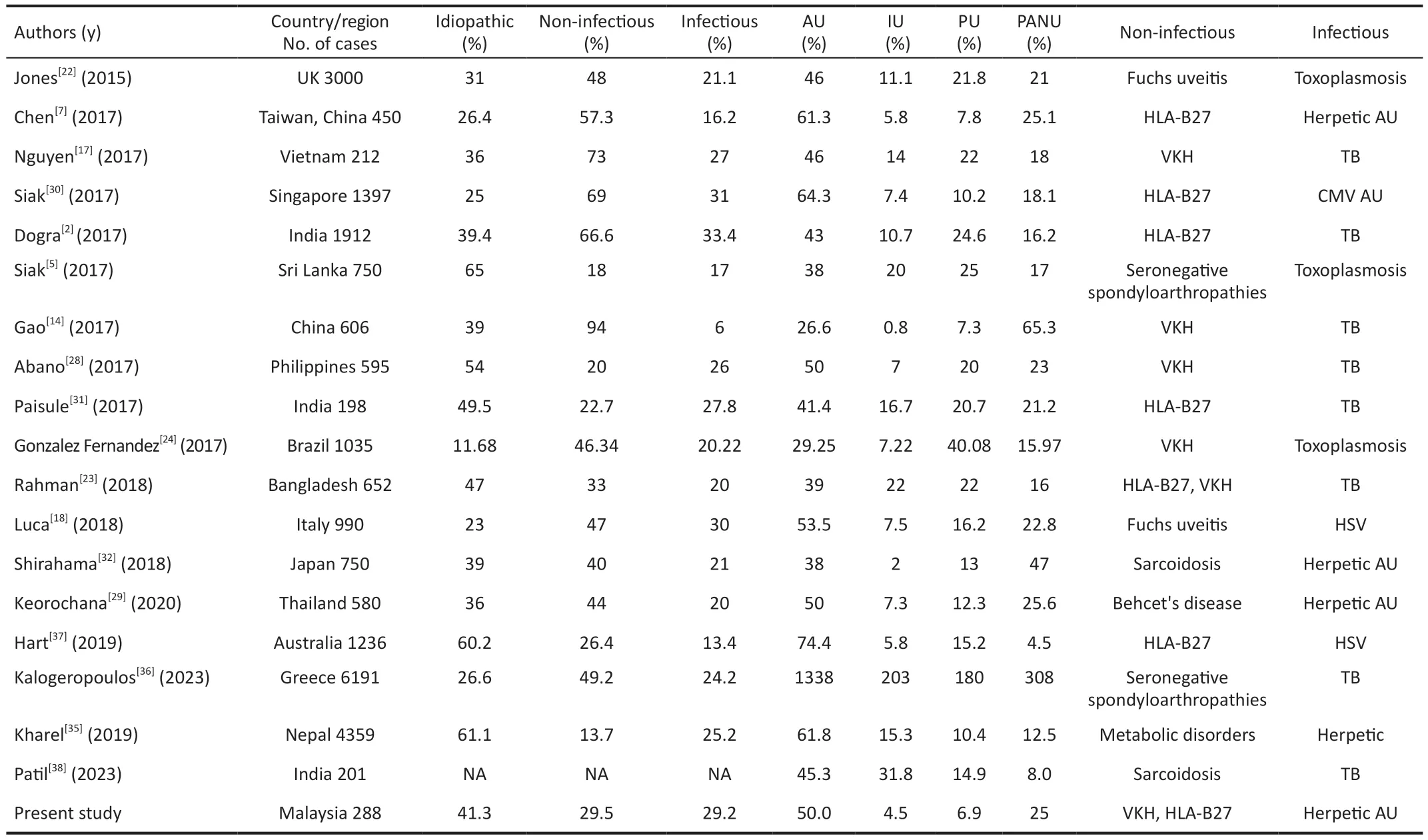
Table 8 Comparison of patterns of uveitis in different countries of the world: type, anatomical location, most common aetiology in the noninfectious and infectious groups
Herpetic iridocyclitis was the commonest infectious aetiology in our study, similar to Singapore[30], Thailand[29], Taiwan China[7], Japan[32], and Italy[18].On the other hand, ocular tuberculosis was the predominant cause in Vietnam[17],Philippines[28], China[14], India[31], and Bangladesh[23]whereas toxoplasmosis was the most common aetiology in Sri Lanka[5]and United Kingdom[22].
Interestingly, in our study, the least common uveitis was intermediate uveitis which was consistent with global data(Table 8) While idiopathic aetiology is the commonest in anterior and intermediate uveitis, Cytomegalovirus (CMV)retinitis was the commonest identifiable aetiology in posterior uveitis (Table 2).All patients with CMV panuveitis or posterior uveitis were immunocompromised due to underlying malignancies like Hodgkin lymphoma, leukaemia, severe combined immunodeficiency, post-organ transplant, systemic viremia, sepsis, and human immunodeficiency virus (HIV)infection.This suggests that advanced immunodeficiency has an elevated risk for posterior disease[11].The youngest patient with CMV panuveitis in our study was a 1-year-old boy who had mature B cell lymphoma and biliary atresia post-liver transplant.
CMV anterior uveitis was reported as a major aetiology of anterior uveitis in Singapore, where it was the second most commonly known cause of anterior uveitis among immunocompetent individuals[30].However, we found that CMV anterior uveitis is less common in our study as compared to Singapore[30].CMV anterior uveitis is possibly underrecognized in our study, as aqueous fluid polymerase chain reaction (PCR) analysis is not routinely done in our centre due to limited accessibility to these tests.However, we do perform ocular fluid molecular testing for patients with high degree of suspicion of viral uveitis such as unilateral, recurrent, acute, or chronic anterior uveitis, hypertensive uveitis, or presentations such as Posner-Schlossman syndrome or Fuchs uveitis syndrome.The tests were not done routinely for all patients due to the added costs to outsource the diagnostic tests to laboratory centres that perform them.
Surprisingly, despite tuberculosis being endemic in our population, it was less commonly encountered in our study compared to CMV uveitis.This could be attributable to the anti-tuberculous medication which is freely available in our country, and it may relate to the effectiveness of the Direct Observed Therapy Short Course (DOTS) implementation that was launched by WHO in 1995 that ensures adherence and good management practice.The challenge in diagnosing tuberculosis is exacerbated by the absence of gold-standard criteria to diagnose ocular tuberculosis, particularly among patients with latent tuberculosis.There were also difficulties in performing diagnostic investigations such as QuantiFERONTB Gold assay, T-SPOT.TB assay, or tuberculosis (TB) PCR for suspected tuberculous uveitis patients as the costs of these tests are borne by the patients and the accessibility to the test is limited.Also, these investigations need to be outsourced to specific laboratories as it is not performed in our hospital.The unavailability of nucleic acid amplification techniques for infectious uveitis such as multi-targeted PCR for TB,toxoplasmosis, and viral uveitis (CMV, varicella-zoster virus,herpes simplex virus) undoubtedly affects diagnostic abilities.Interestingly, we found toxoplasmosis as the second most common infectious aetiology in panuveitis following endogenous endophthalmitis (Table 2).A possible reason could be that toxoplasmosis has a high prevalence among the Malaysian population.It is interesting to note that the Malays ethnicity has the highest number of ocular toxoplasmosis compared to other races (Chinese and Indian).One local-based study found that the highest sero-prevalence of toxoplasmosis was in the Malays when compared with other races (Chinese and Indians)[19].This could be explained by the previous findings of Malay’s preponderance of keeping pet cats in their house where they might be more prone to be exposed to contaminated cat faeces[19].
Among the scleritis cases, the high predominance of anterior scleritis seen in our study was similar to Nepal[37](Table 3).In our study, the majority of scleritis cases were idiopathic causes,unlike in Ganet al[39]study where infectious causes such as endogenous endophthalmitis were predominant.
Complications from uveitis and scleritis were seen in 27.1%of our patients.Intra-ocular complications can arise from the intraocular inflammation itself as well as the steroid treatments[8].The most common complication was glaucoma(47.5%), followed by cystoid macula oedema (18.9%) and cataract (13.9%).These three most common complications were similar to the studies reported from China[14], Italy[18], and Thailand[29].
In our study, intraocular pressure elevation is the commonest complication in anterior uveitis followed by panuveitis,whereas cystoid macula oedema is the commonest in intermediate uveitis.Besides trabeculitis as a known cause of IOP elevation, clogging of the trabecular meshwork by trabecular precipitates such as inflammatory cells, debris, and proteins in the anterior chamber, further leads to a decrease in trabecular outflow causing IOP elevation[40].Furthermore,it can also be caused by treatment-related complications such as steroid-induced reduction in outflow through the trabecular meshwork obstruction by oedema of the trabecular meshwork cells and deposition of extracellular matrix degradation products.These steroid responders often represent a therapeutic challenge among uveitis patients.A total of 3.7% had low IOP in our study.Despite the uncertain aetiology, this may be related to the prostaglandin-mediated increase in uveoscleral outflow as well as the hyposecretion of aqueous humour[40].
Despite the majority of our patients (82%) having good visual outcome at one year of follow-up, about 14.5% of them ended up clinically blind (Table 5).Posterior uveitis, panuveitis and visual acuity worse than 3/60 at presentation were more likely associated with poor visual outcomes.Thus, prompt treatment and close monitoring for patients with poor vision at the onset especially with posterior and panuveitis might reduce the risk of poor visual outcomes.
The limitations of this study included employing a singlecentre data collection, which may not reflect population studies or actual uveitis patterns in Malaysia.A multicentre longitudinal study will give a more accurate picture on the pattern of uveitis in our setting.A longer follow-up period for such patients will also be ideal as some disease patterns may change over time and some cases of idiopathic uveitis may obtain a specific diagnosis.
In conclusion, knowledge in uveitis and scleritis epidemiology can potentially contribute to a more strategic utilization of laboratory and financial resources, which might lead to cost savings that are beneficial for patients.We hope that our work can pave the road for future epidemiologic studies to compare ocular inflammatory diseases among different countries and ethnicity.
ACKNOWLEDGEMENTS
Conflicts of Interest:Seow ST,None;Tajunisah I,None;Lee FY,None;Lott PW,None;Reddy SC,None.
 International Journal of Ophthalmology2024年3期
International Journal of Ophthalmology2024年3期
- International Journal of Ophthalmology的其它文章
- Late infection after peri-orbital autologous micro-fat graft:a case presentation and literature review
- Stromal lenticule addition keratoplasty with corneal crosslinking for corneal ectasia secondary to FS-LASlK:a case series
- Clinical features and possible pathogenesis of multiple evanescent white dot syndrome with different retinal diseases and events: a narrative review
- Utility of real-time 3D visualization system in the early stage of phacoemulsification training
- Efficacy of scleral buckling for the treatment of rhegmatogenous retinal detachment using a novel foldable capsular buckle
- Effect of navigation endoscopy combined with threedimensional printing technology in the treatment of orbital blowout fractures
