Hepatic cystic lesions mimicking liver abscess on imaging: A report of two cases
Yun-Wen Jing ,Yong-Hong Yu ,Tin-An Jing ,Shu-Yun Tin,∗
a Department of Ultrasound Medicine, Tongde Hospital of Zhejiang Province, Hangzhou 310012, China
b Department of Ultrasound Medicine, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China
Hepatic cystic lesions include congenital dysplasia,inflammatory cystic lesions,neoplastic cystic lesions and parasitic cystic lesions.As different treatment modalities can be chosen for these lesions,differential diagnosis is particularly important [1].Clinical features or imaging findings of cystic lesions of the liver are typical;for instance,liver abscess often shows thick-walled enhancement on contrast-enhanced CT,with a "target sign" or "double ring sign".Some neoplastic lesions of the liver may mimic liver abscesses on imaging,which can be easily misdiagnosed in clinical practice.Herein we reported two patients diagnosed with liver abscess on imaging without typical clinical features,which were finally confirmed to be a large cell neuroendocrine carcinoma (LCNEC) and a bile duct hamartoma (BDH) by pathology.The clinical data of these two patients are shown in Table 1.
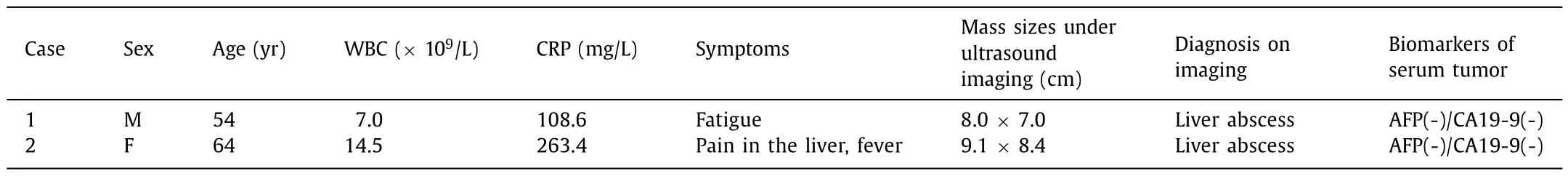
Table 1Clinical data of these two patients.
Both patients underwent abdominal ultrasonography,contrastenhanced computed tomography (CECT) and contrast-enhanced magnetic resonance imaging (CE-MRI).Abdominal ultrasonography was performed using the GE Logiq E9 ultrasonic diagnostic instrument (General Electric Company,Boston,MA,USA) with probe frequency of 3.5 MHz;CECT was performed using a dual-source CT scanner (Siemens Somaton Definition Flash,Forchheim,Germany),and contrast agent Ultravist 370 (Scherning AG,Berlin,Germany).CE-MRI was performed using a 3.0 Tesla Siemens scanner (Siemens Magnetom Verio,Erlangen,Germany),and contrast agent Gd-DTPA(Omniscan;Nycomed,Oslo,Norway).
This study was approved by the Ethics Committee of the Tongde Hospital of Zhejiang Province.Signed informed consents were obtained from the patients or families.
Case 1,a 54-year-old male,presented to our hospital because of fatigue.This patient had the past medical history of "hepatic cyst,cholecystolithiasis and acute biliary pancreatitis".There were no positive signs on physical examination.Abnormal laboratory findings included C-reactive protein (CRP): 108.6 mg/L (normal:<6 mg/L),fibrinogen: 8.64 g/L (normal: 1.9-3.9 g/L),while serum alpha-fetoprotein (AFP),carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA19-9) levels were normal.Abdominal ultrasonography revealed a round unicystic mass with no blood flow signal in segment VI/VII of the liver (Fig.1 A,B).Because the mass appeared suddenly and grew quickly,CECT was performed,which showed a low-density area with clear boundaries in the arterial phase (Fig.1 C),and thick-walled enhancement in the delayed phase (Fig.1 D).MRI showed a slightly high signal with a clear boundary in T1-weighted imaging (Fig.1 E),and a high signal in T2-weighted imaging (Fig.1 F),diffusion-weighted imaging (DWI)(Fig.1 G) and apparent diffusion coefficient (ADC) (Fig.1 H).CE-MRI showed a lesion with thick-walled enhancement (Fig.1 I,J).
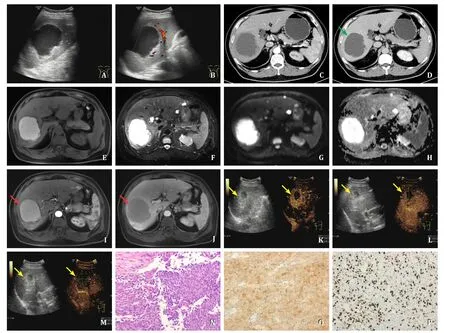
Fig.1. Abdominal ultrasonography,contrast-enhanced computed tomography (CECT),contrast-enhanced magnetic resonance imaging (CE-MRI),contrast-enhanced ultrasound(CEUS) and pathology of case 1.A: Gray scale ultrasound showed a round unicystic mass in right liver;B: color Doppler flow imaging (CDFI) showed the cystic mass with no blood flow signal;C: CECT for the mass in the arterial phase showed a low-density area with clear boundaries;D: the mass was with thick-walled enhancement in the delayed phase (green arrow);E-H: MRI showed a slightly high signal with a clear boundary in T1-weighted imaging,and a high signal in T2-weighted imaging,diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC);I-J: CE-MRI showed that the tumor had thick-walled enhancement (red arrow),and internal cystic component was not enhanced in the arterial phase and the delayed phase;K-M: peripheral solid component significantly increased after percutaneous drainage.CEUS showed hyper-enhancement in the arterial phase (K),and hypo-enhancement in the portal phase (L) and the delayed phase (M) (yellow arrow);N: tumor stained with hematoxylin and eosin (original magnification×10);O: Syn (+) was detected by immunohistochemical staining (original magnification×10);P: Ki-67 (+,60%) was detected by immunohistochemical staining (original magnification×10).
This patient did not have manifestations of a typical infection,but his medical histories about biliary system-related diseases were major risk factors for liver abscess.What is more,his imaging findings mimicked liver abscess.Thus,the preliminary diagnosis was liver abscess.
Ultrasound-guided percutaneous transhepatic puncture and drainage was performed in September 2021.Interestingly,the drainage fluid was not purulent,but was dark black.Culture of bacteria and fungi,detection of amoebas and tumor markers were carried out on the drainage fluid.Abnormal laboratory findings included AFP 7.8 ng/mL,CA19-9 58.57 U/mL,CEA 29.26 ng/mL,while the result of bacteria and fungi culture was negative,and amoebas were not detected.The drainage fluid changed from dark black to bright red after percutaneous drainage.Daily drainage volume varied from 10 to 100 mL.Repeated abdominal ultrasonography showed that the mass shrank first and then increased in size,and the solid component of the lesion significantly increased.Mass size underwent ultrasonography was 8.0×7.0 cm before drainage,4.8×4.5 cm on the 7th day after drainage,4.0×3.7 cm on the 14th day after drainage,and 5.7×5.7 cm on the 21st day after drainage.Contrast-enhanced ultrasound (CEUS) was then performed using the contrast agent SonoVue (Bracco,Milan,Italy).Peripheral solid component showed hyper-enhancement in the arterial phase (Fig.1 K),and hypo-enhancement in the portal phase(Fig.1 L) and the delayed phase (Fig.1 M).In order to confirm the diagnosis,ultrasound-guided biopsy was performed.The pathology revealed a malignant lesion.
Case 2,a 64-year-old female,presented to our hospital with pain in the liver associated with fever.This patient had the past medical history of "hepatic cyst and cholecystolithiasis".On physical examination,temperature was 37.4-38.1 °C,and the right upper abdomen was tender without rebound tenderness.Abnormal laboratory findings included white blood cell (WBC) count:14.5×109/L (normal: 3.5×109/L-9.5×109/L),CRP: 263.4 mg/L(normal:<6 mg/L),fibrinogen: 8.65 g/L (normal: 1.9-3.9 g/L),while serum AFP,CEA and CA19-9 levels were normal.An irregular multicystic mass with a small amount of scattered blood flow signal in segment VIII of the liver was found by abdominal ultrasonography (Fig.2 A,B).CECT showed an irregular multicystic lowdensity area in the arterial phase (Fig.2 C),with peripheral rim and septa hyper-enhancement in the delayed phase (Fig.2 D).MRI showed that the tumor manifested a low signal with clear boundaries in T1-weighted imaging (Fig.2 E),and a high signal in T2-weighted imaging (Fig.2 F),DWI (Fig.2 G) and ADC (Fig.2 H).CEMRI showed that the tumor had peripheral rim and septa hyperenhancement,and internal cystic component was not enhanced in the arterial phase and the delayed phase (Fig.2 I,J).
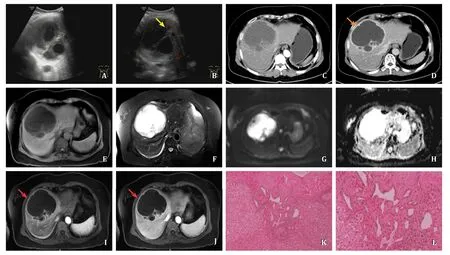
Fig.2. Abdominal ultrasonography,contrast-enhanced computed tomography (CECT),contrast-enhanced magnetic resonance imaging (CE-MRI) and pathology of case 2.A:Gray scale ultrasound showed an irregular multicystic mass in right liver;B: color Doppler flow imaging (CDFI) showed the mass with a small amount of scattered blood flow signal (yellow arrow);C: CECT for the mass in the arterial phase showed an irregular multicystic low-density area;D: the mass was with peripheral rim and septa hyper-enhancement in the delayed phase (orange arrow);E-H: MRI showed that the tumor manifested a low signal with clear boundaries in T1-weighted imaging,and a high signal in T2-weighted imaging,DWI and ADC;I-J: CE-MRI showed that the tumor had peripheral rim and septa hyper-enhancement,and internal cystic component was not enhanced in the arterial phase and the delayed phase (red arrow);K-L: regular pathology showed the hyperplasia of bile ducts,necrotic tissue,fibrous tissue and numerous inflammatory cells in the mass (K: original magnification×5;L: original magnification×10).
Based on the medical history,the manifestations of fever and typical infection,and thick-walled enhancement on contrastenhanced imaging,the preliminary diagnosis was liver abscess.
Ultrasound-guided percutaneous transhepatic puncture and drainage was performed in January 2022.The drainage fluid was yellowish with an increasing reduction in volume.A small amount ofElizabethkingiaMeningosepticumwas found after the culture of bacteria and fungi on the drainage fluid.In order to confirm the diagnosis,ultrasound-guided biopsy was performed.The pathology revealed biliary cystadenoma with moderate-severe dysplasia of the biliary epithelium.
Surgical treatment,routine histopathological examination and immunohistochemical staining were performed in both patients.The pathology confirmed that the lesion was LCNEC in case 1(Fig.1 N-P) and was BDH with cystic dilatation of the bile duct and infection in case 2 (Fig.2 K,L).
LCNECs originate from neuroendocrine cells,and mainly occur in the gastrointestinal tract or pancreas.Primary LCNECs in the liver are extremely rare [2,3].BDHs are usually benign malformations of the hepatobiliary system,mostly asymptomatic.They are infrequent anomalies in adults (5.6%),and are more common in males than in females [4,5].In the present report,the clinical features were not typical in both patients.
On imaging,typical LCNECs often shows hyperechoic lesions,and typical BDHs often shows multiple hyperechoic lesions and hypoechoic lesions less than 1 cm in diameter with multiple comet tail like echoes in the liver.A single cystic lesion in the liver which was finally confirmed to be LCNEC or BDH had rarely been reported.
Reviewing the diagnosis and treatment processes of the patients,we found that the characteristics of the drainage fluid and the changes of the lesion size after percutaneous drainage can indicate the biological characteristics of the lesion.In addition,clinicians should be alert to intrahepatic thick-walled cystic masses without extrahepatic infection.If a malignancy was suspected,ultrasound-guided biopsy should be performed as early as possible.However,when the solid component accounted for only a very small proportion of the lesion and the successful rate of immediate puncture was low,clinicians could first perform drainage and then puncture.
Acknowledgments
None.
CRediT authorship contribution statement
Yun-Wen Jiang:Data curation,Investigation,Writing– original draft.Yong-Hong Yu:Data curation.Tian-An Jiang:Conceptualization.Shu-Yuan Tian:Conceptualization,Funding acquisition,Investigation,Writing– review &editing.
Funding
This study was supported by a grant from the Exploration Project of Natural Science Foundation of Zhejiang Province(LY20H180002).
Ethical approval
This study was approved by the Ethics Committee of Tongde Hospital of Zhejiang Province.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2024年1期
Hepatobiliary & Pancreatic Diseases International2024年1期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Recent advances in promising drugs for primary prevention of gastroesophageal variceal bleeding with cirrhotic portal hypertension
- Stereotactic body radiotherapy in pancreatic adenocarcinoma
- Application of ultrasonography-elastography score to suspect porto-sinusoidal vascular disease in patients with portal vein thrombosis
- Polydatin ameliorates hepatic ischemia-reperfusion injury by modulating macrophage polarization
- Hypomethylation of glycine dehydrogenase promoter in peripheral blood mononuclear cells is a new diagnostic marker of hepatitis B virus-associated hepatocellular carcinoma
- AGK2 pre-treatment protects against thioacetamide-induced acute liver failure via regulating the MFN2-PERK axis and ferroptosis signaling pathway
