术中血糖波动和术后胰岛素抵抗对胸腔镜肺癌根治术后老年患者认知功能障碍的影响
陈慧敏 贾洪峰 江婷婷 贾耀辉


摘要:目的 分析術中血糖波动和术后胰岛素抵抗(IR)对老年全麻胸腔镜肺癌根治术患者术后认知功能障碍(POCD)的影响。方法 收集352例老年全麻胸腔镜肺癌根治术患者,分为POCD组(84例)和非POCD组(268例),利用倾向性评分匹配法(PSM)均衡2组间协变量,84例匹配成功,比较PSM前后2组资料差异。PSM后,绘制血糖波动幅度预测POCD的受试者工作特征(ROC)曲线,根据截断值分为低水平血糖波动组(97例)和高水平血糖波动组(71例),并根据术后是否发生IR分为IR组(53例)和非IR组(115例),比较组间POCD发生率。采用Logistic回归分析POCD的影响因素。结果 PSM前,POCD组的年龄、血糖波动幅度、IR比例、手术时间、麻醉时间、麻醉维持期间丙泊酚用量、瑞芬太尼用量和舒芬太尼用量大于非POCD组(P<0.05);PSM后,POCD组血糖波动幅度和IR比例大于非PCOD组(P<0.05)。PSM后,高水平血糖波动组和IR组POCD发生率分别高于低水平血糖波动组和非IR组(P<0.05)。Logistic回归显示,术中血糖波动幅度大(OR=9.140,95%CI:4.338~19.257)和术后发生IR(OR=4.034,95%CI:1.163~13.991)是POCD的危险因素。结论 术中血糖波动幅度大和术后发生IR的老年全麻胸腔镜肺癌根治术患者POCD发生风险升高。
关键词:血糖;胰岛素抵抗;胸腔镜检查;麻醉,全身;术后认知并发症;认知功能障碍;老年人;肺癌根治术
中图分类号:R614.2文献标志码:ADOI:10.11958/20230390
Effects of intraoperative blood glucose fluctuation and postoperative insulin resistance on cognitive dyfunction in elderly patients after thoracoscopic radical resection of lung cancer under general anesthesia
Abstract: Objective To analyze the influence of intraoperative blood glucose fluctuation and postoperative insulin resistance (IR) on postoperative cognitive dyfunction (POCD) in elderly patients undergoing thoracoscopic radical resection of lung cancer under general anesthesia. Methods A total of 352 elderly patients undergoing thoracoscopic radical resection of lung cancer under general anesthesia were collected and divided into the POCD group (n=84) and the non-POCD group (n=268). The covariates between the two groups were balanced by propensity score matching method (PSM). Eighty-four cases in each group were successfully matched. The data between the two groups before and after PSM were compared. After PSM, receiver operating characteristic (ROC) curve of blood glucose fluctuation amplitude for predicting POCD was drawn, and patients were divided into the low-level blood glucose fluctuation group (n=97) and the high-level blood glucose fluctuation group (n=71) according to the cut-off value. According to the existence of postoperative IR, patients were divided into the IR group (n=53) and the non-IR group (n=115). Then, incidences of POCD between groups were compared. Logistic regression was used to analyze the influencing factors of POCD. Results Before PSM, the POCD group had older age, higher blood glucose fluctuation amplitude, IR ratio, operation time, anesthesia time, propofol dosage, remifentanil dosage and sufentanil dosage in anesthesia maintenance period than those in the non-POCD group (P<0.05). The POCD group had higher blood glucose fluctuation amplitude and IR ratio than those in the non-POCD group after PSM (P<0.05). After PSM, the incidences of POCD in the high-level blood glucose fluctuation group and the IR group were higher than those in the low-level blood glucose fluctuation group and the non-IR group (P<0.05). Logistic regression analysis showed that higher intraoperative blood glucose fluctuation (OR=9.140, 95%CI: 4.338-19.257) and postoperative IR (OR=4.034, 95%CI: 1.163-13.991) were risk factors of POCD. Conclusion The risk of POCD in elderly patients undergoing thoracoscopic radical lung cancer surgery under general anesthesia is increased in patients with higher intraoperative blood glucose fluctuation and postoperative IR.
Key words: blood glucose; insulin resistance; thoracoscopy; anesthesia, general; postoperative cognitive complications; cognitive dysfunction; aged; radical lung cancer surgery
全麻胸腔镜肺癌根治术是肺癌的重要治疗手段。术后认知功能障碍(postoperative cognitive dysfunction,POCD)是全麻术后常见并发症,表现为意识混乱、记忆受损、注意力减退等症状,其发生率较高,严重影响患者生活质量[1-2]。POCD的发病机制尚不明确,既往研究多认为与手术时间、麻醉时间、麻醉药物、年龄等有关[3-4],但这些因素不能完全解释POCD的发生,有必要进一步探讨。手术患者在术中会表现出一定应激反应,分泌大量胰岛素拮抗激素,导致血糖升高,出现血糖波动[5]。围手术期胰岛素抵抗(insulin resistance,IR)是机体对胰岛素敏感性和反应性降低的一种病理状态[6]。血糖波动、IR与认知功能相关[7-8]。但术中血糖波动和术后IR对POCD的影响尚不清楚。本研究探讨了术中血糖波动和术后IR对老年全麻胸腔镜肺癌根治术患者POCD的影响,旨在为POCD的预防提供参考依据。
1 对象与方法
1.1 研究对象 选取2021年1月—2022年12月于西安交通大学医学部附属三二〇一医院进行手术治疗的352例老年肺癌患者作为研究对象。纳入标准:(1)病理学确诊为肺癌,接受胸腔镜肺癌根治术治疗。(2)年龄≥60岁,受教育程度中学及以上。(3)术前1 d行简易智力状况检查(mini-mental state examination,MMSE)量表评估提示该评分在正常范围,即27~30分。(4)麻醉方式为全麻,全麻药物给药方法一致;美国麻醉医师协会(American Society of Anesthesiologists,ASA)分级Ⅱ或Ⅲ级。(5)患者能够正常交流,配合量表评估。(6)心肺、肝肾功能无明显异常。排除标准:(1)有脑部外伤史、脑部手术史或腹部手术史。(2)脑血管疾病后遗症。(3)精神疾病。(4)长期服用精神类药物或酗酒,长期服用激素等导致血糖升高药物。(5)凝血功能障碍、自身免疫系统疾病、糖尿病。(6)手术或者麻醉禁忌证。本研究获得所有患者及家属知情同意,经医院伦理委员会审批通过(批准编号2020016)。
1.2 麻醉方法和患者自控镇痛(patient controlled analgesia,PCA) 麻醉诱导方案:先后静脉注射丙泊酚2.5 mg/kg、瑞芬太尼0.5 μg/kg、顺式阿曲库铵0.025 mg/kg,诱导结束后气管插管维持通气。麻醉维持方案:持续泵入丙泊酚5 mg/(kg·h),瑞芬太尼0.5 μg(/kg·h),间断泵入舒芬太尼0.2 μg/kg,手术结束后停止应用上述麻醉药物。麻醉过程中未应用其他药物。术后常规给予PCA镇痛。
1.3 术中血糖波动和术后IR监测 于手术开始时、术中每30 min、手术结束时监测血糖,取血糖监测值的最大值和最小值,二者之差为血糖波动幅度。于术后1~5 d抽取患者空腹静脉血,检测血糖和胰岛素水平。根据胰岛素抵抗稳态模型(homeostasis model assessment of inusilin resistance,HOMA-IR)判断是否存在IR。HOMA-IR=空腹血糖(mmol/L)×空腹胰岛素(mU/L)/22.5,HOMA-IR≥1.73为存在IR[9]。
1.4 POCD评判标准 术前1 d及术后1周,采用MMSE量表评估患者认知功能,术后1周MMSE评分较术前1 d降低超过2分则判定为发生POCD[10]。根据是否发生POCD将患者分为POCD组84例和非POCD组(非POCD组1)268例。
1.5 收集资料 收集患者性别、年龄、体质量指数(BMI)、吸烟、饮酒、合并高血压、合并高脂血症、ASA分级、术前1 d MMSE评分、术中血糖波动幅度、IR、手术时间、麻醉时间、麻醉维持期间丙泊酚用量、瑞芬太尼用量、舒芬太尼用量等临床资料。
1.6 单因素分析 使用倾向性评分匹配法(propensity score matching,PSM)1∶1匹配POCD组和非POCD组临床资料相近的患者,需要匹配的变量为年龄、手术时间、麻醉时间、麻醉维持期间丙泊酚用量、瑞芬太尼用量、舒芬太尼用量。PSM匹配后,将匹配成功的84例非COPD患者作为非COPD组2。比较PSM前后POCD组和非POCD组患者临床资料差异。
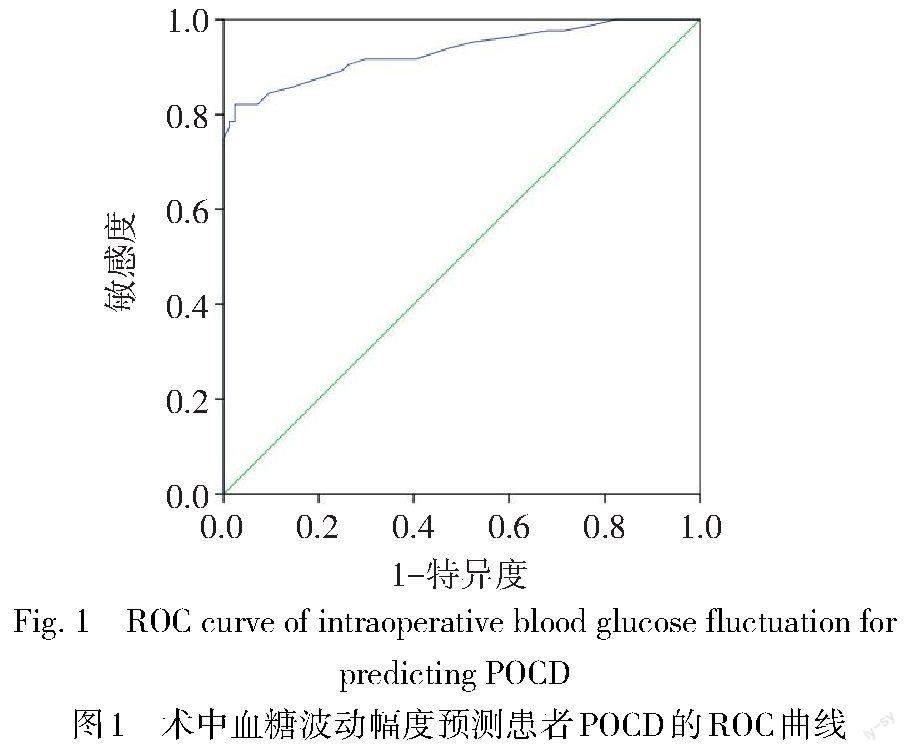
1.7 POCD发生率比较 绘制血糖波动幅度预测POCD发生的受试者工作特征(ROC)曲线,根据血糖波动幅度预测POCD发生的最佳截断值将患者分为低水平血糖波动组(血糖波动<3.15 mmol/L,97例)和高水平血糖波动组(血糖波动≥3.15 mmol/L,71例),并根据术后是否发生IR将患者分为IR组(53例)和非IR组(115例),比较低、高水平血糖波动组间及IR组、非IR组间的POCD发生率。
1.8 多因素二元Logistic回归分析 将PSM后POCD组和非POCD组差异有统计学意义的因素纳入二元Logistic回归模型,分析影响老年全麻胸腔镜肺癌根治术患者发生POCD的危险因素。
1.9 统计学方法 采用SPSS 23.0软件和R软件(R4.3.1)进行分析。计数资料以例(%)表示,组间比较采用χ2检验。计量资料以均数±标准差([[x] ±s
])表示,组間比较采用t检验。采用R软件进行PSM分析,1∶1匹配POCD组和非POCD组需要平衡的变量,选择最邻近匹配。采用ROC曲线分析血糖波动幅度对POCD发生的预测价值。采用多因素二元Logistic回归分析发生POCD的影响因素。P<0.05为差异有统计学意义。
2 結果
2.1 PSM前后患者POCD的单因素分析 PSM前,POCD组年龄、IR比例、血糖波动幅度、手术时间、麻醉时间、麻醉维持期间丙泊酚用量、瑞芬太尼用量和舒芬太尼用量大于非POCD组(P<0.05)。PSM后,POCD组仅IR比例和血糖波动幅度比例大于非POCD组(P<0.05)。见表1。
2.2 术中血糖波动幅度对患者发生POCD的预测价值 PSM后,血糖波动幅度预测患者POCD的AUC为0.933,95%CI为0.894~0.972(P<0.01),截断值为3.15 mmol/L,敏感度为82.1%,特异度为97.6%,见图1。
2.3 血糖波动幅度和IR对患者POCD的影响 高水平血糖波动组POCD发生率(97.2%,69例)高于低水平血糖波动组(15.5%,15例,χ2=109.504,P<0.01)。IR组POCD发生率(69.8%,37例)高于非IR组(40.9%,47例,χ2=12.156,P<0.01)。
2.4 患者发生POCD的影响因素分析 以是否发生POCD为因变量(是=1,否=0),以血糖波动幅度、IR(是=1,否=0)为自变量,进行多因素Logistic回归分析。结果显示,术中血糖波动幅度大和术后发生IR是老年全麻胸腔镜肺癌根治术患者POCD的危险因素(P<0.05),见表2。
3 讨论
3.1 全麻胸腔镜肺癌根治术的老年患者具有较高的POCD发生率 本研究中,接受全麻胸腔镜肺癌根治术的老年患者术后1周时的POCD发生率为23.9%,与既往数据中非心脏手术患者POCD发生率在17.1%~41.4%的结果类似[11],而低于苏容容等[12]研究中胸腔镜根治术患者37.0%的POCD发生率。分析原因,一方面可能与手术技术、围手术期管理的进步有关;另一方面可能与术后常规应用PCA镇痛减少疼痛刺激传入、降低氧化应激和中枢炎性反应有关[13]。但是,本研究中老年全麻胸腔镜肺癌根治术患者POCD的发生率仍然较高,主要与老年人生理功能逐渐减退,对手术的应激能力和药物的代谢能力下降,脑细胞代谢障碍风险明显增加等因素有关[14]。因此,识别老年全麻胸腔镜肺癌根治术患者POCD的危险因素并进行针对性干预具有重要临床意义。
3.2 术中血糖波动幅度大是POCD的危险因素 对于手术患者,一方面手术创伤会诱发机体分泌儿茶酚胺、皮质醇等多种胰岛素拮抗因子,促使血糖升高;另一方面长时间禁食可能会引起患者低血糖,可增加围手术期并发症发生风险[15]。鲁国等[16]在急性脑梗死伴糖尿病患者认知功能障碍相关研究中发现,认知功能障碍组患者的血糖波动幅度、血糖变异率等血糖变异指标高于认知功能正常组患者。Lim等[17]研究认为血糖变化在预测卒中后认知功能障碍方面具有重要价值。以上研究均提示血糖波动与认知功能有关。但关于术中血糖波动对POCD影响的研究较少。本研究显示,术中血糖波动幅度对POCD发生具有较好的预测价值,高水平血糖波动组患者POCD发生率高于低水平血糖波动组,且术中血糖波动幅度大是老年全麻胸腔镜肺癌根治术患者发生POCD的危险因素。分析原因,机体的抗氧化平衡机制在高血糖和低血糖的状态下会发生改变,导致氧化应激和炎症反应加重,从而导致神经炎症和认知功能障碍[18-19]。因此,在手术过程中,应当密切监测血糖,采取合理的控制血糖方案,保持血糖平稳,避免血糖剧烈波动。
3.3 术后发生IR是老年全麻胸腔镜肺癌根治术患者POCD的危险因素 围手术期IR是指手术患者在应激下表现出的对胰岛素的敏感性和反应性降低的一种病理状态,严重影响患者的术后恢复[20]。但术后发生IR是否会增加POCD的发生风险尚不清楚。本研究显示,IR组患者POCD发生率高于非IR组,且术后发生IR是老年全麻胸腔镜肺癌根治术患者发生POCD的危险因素。这可能与以下机制有关:(1)IR可引起血管内皮功能障碍,加重机体的炎症反应和氧化应激[21-22]。(2)IR可引起脑组织低灌注,导致脑组织缺血缺氧[23]。(3)IR导致的外周高胰岛素血症会引发海马体氧化应激反应和神经炎症,导致认知功能障碍的发生[24]。因此,应当关注围手术期IR,从减轻IR程度的角度达到预防POCD的目的。
综上所述,老年全麻胸腔镜肺癌根治术患者具有较高的POCD发生率,术中血糖波动幅度大和术后发生IR是其危险因素,应该密切监测血糖和IR,保持术中血糖平稳和减轻术后IR。但本研究中的病例均来自同一医院,在病例的选择上可能存在一定的偏倚,还需要扩大样本范围,进行多中心的研究,更深入探讨术中血糖波动幅度和术后IR对老年全麻胸腔镜肺癌根治术患者POCD的影响,为POCD的预防提供更多的参考依据。
参考文献
[1] ACKENBOM M F,BUTTERS M A,DAVIS E M,et al. Incidence of postoperative cognitive dysfunction in older women undergoing pelvic organ prolapse surgery[J]. Int Urogynecol J,2021,32(2):433-442. doi:10.1007/s00192-020-04495-y.
[2] WANG W,MA Y,LIU Y,et al. Effects of dexmedetomidine anesthesia on early postoperative cognitive dysfunction in elderly patients[J]. ACS Chem Neurosci,2022,13(15):2309-2314. doi:10.1021/acschemneuro.2c00173.
[3] ENGIN M,GUVENC O. Many factors affect postoperative cognitive functions[J]. J Card Surg,2022,37(12):5702. doi:10.1111/jocs.17034.
[4] URCUN YS,ALTUN Y,PALA A A. Early and late predictors of postoperative neurocognitive dysfunction in cardiac surgery[J]. Ideggyogy Sz,2022,75(7-08):231-240. doi:10.18071/isz.75.0231.
[5] KURRA R JR,MADHUSUDHANA R. Impact of different crystalloids on the blood glucose levels of nondiabetic patients undergoing major elective surgeries[J]. Cureus,2023,15(1):e34294. doi:10.7759/cureus.34294.
[6] CHOI Y S,CHO B W,KIM H J,et al. Effect of preoperative oral carbohydrates on insulin resistance in older adults who underwent total hip or knee arthroplasty:a prospective randomized trial[J]. J Am Acad Orthop Surg,2022,30(20):971-978. doi:10.5435/JAAOS-D-21-00656.
[7] MENG Q Z,WANG Y,LI B,et al. Relationship between glycemic variability and cognitive function in lacune patients with type 2 diabetes[J]. World J Clin Cases,2023,11(5):1019-1030. doi:10.12998/wjcc.v11.i5.1019.
[8] CUI Y,TANG T Y,LU C Q,et al. Insulin resistance and cognitive impairment:evidence from neuroimaging[J]. J Magn Reson Imaging,2022,56(6):1621-1649. doi:10.1002/jmri.28358.
[9] 劉波. 胰岛素抵抗与骨质疏松椎体性压缩骨折椎体成形术后新发骨折风险的相关性研究[D]. 泸州:西南医科大学,2018. LIU B. The correlation between insulin resistance and the risk of new fractures after vertebroplasty for osteoporotic vertebral compression fractures[D]. Luzhou:Southwest Medical University,2018.
[10] 唐东彪,田冶. Narcotrend监测下麻醉深度对老年患者胃肠道肿瘤手术后认知功能障碍的影响[J]. 中国病理生理杂志,2020,36(3):475-478. TANG D B,TIAN Y. Effect of anesthesia depth with Narcotrend monitoring on cognitive function after gastrointestinal tumor surgery in elderly patients[J]. Chinese Journal of Pathophysiology,2020,36(3):475-478. doi:10.3969/j.issn.1000-4718.2020.03.0014.
[11] TJEERTES E,VAN FESSEM J,MATTACE-RASO F,et al. Influence of frailty on outcome in older patients undergoing non-cardiac surgery:a systematic review and Meta-analysis[J]. Aging Dis,2020,11(5):1276-1290. doi:10.14336/AD.2019.1024.
[12] 苏容容,刘长红. 胸腔镜肺癌根治术后认知功能障碍对患者康复效果的影响[J]. 中国医学前沿杂志(电子版),2020,12(11):53-57. SU R R,LIU C H. Effect of postoperative cognitive dysfunction on rehabilitation of patients undergoing thoracoscopic radical resection of lung cancer[J]. Chinese Journal of the Frontiers of Medical Science(Electronic Version),2020,12(11):53-57. doi:10.12037/YXQY.2020.11-09.
[13] 魏巍,郑曦,谷宇,等. 术后镇痛策略对老年单肺通气患者术后神经认知功能及早期康复的影响:90例随机对照临床试验[J]. 南方医科大学学报,2020,40(12):1821-1825. WEI W,ZHENG X,GU Y,et al. Effects of different postoperative analgesic strategies on postoperative neurocognitive function and quality of recovery in elderly patients undergoing one lung ventilation[J]. Journal of Southern Medical University,2020,40(12):1821-1825. doi:10.12122/j.issn.1673-4254.2020.12.19.
[14] YONG R,MENG Y. Preoperative neutrophil-lymphocyte ratio,an independent risk factor for postoperative cognitive dysfunction in elderly patients with gastric cancer[J]. Geriatr Gerontol Int,2020,20(10):927-931. doi:10.1111/ggi.14016.
[15] YOU H,HOU X,ZHANG H,et al. Effect of glycemic control and glucose fluctuation on in-hospital adverse outcomes after on-pump coronary artery bypass grafting in patients with diabetes: a retrospective study[J]. Diabetol Metab Syndr,2023,15(1):20. doi:10.1186/s13098-023-00984-4.
[16] 魯国,黄新颖,刘宏伟. 血糖变异性与急性脑梗死伴糖尿病患者短期认知功能的相关性分析[J]. 中国现代医学杂志,2018,28(28):61-66. LU G,HUANG X Y,LIU H W. Association of blood glucose variability with short-term cognitive function in patients with acute cerebral infarction complicated with diabetes mellitus[J]. China Journal of Modern Medicine,2018,28(28):61-66. doi:10.3969/j.issn.1005-8982.2018.28.011.
[17] LIM J S,KIM C,OH M S,et al. Effects of glycemic variability and hyperglycemia in acute ischemic stroke on post-stroke cognitive impairments[J]. J Diabetes Complications,2018,32(7):682-687. doi:10.1016/j.jdiacomp.2018.02.006.
[18] MASCARENHAS FONSECA L,STRONG R W,SINGH S,et al. Glycemic variability and fluctuations in cognitive status in adults with type 1 diabetes (glucog):observational study using ecological momentary assessment of cognition[J]. JMIR Diabetes,2023,8:e39750. doi:10.2196/39750.
[19] 王敏,秦洁,李岚昕,等. 2型糖尿病增加帕金森病风险相关机制研究进展[J]. 中国现代神经疾病杂志,2023,23(6):566-570. WANG M,QIN J,LI L X,et al. Advance on mechanism of type 2 diabetes mellitus increasing the risk of Parkinson's disease[J]. Chin J Contemp Neurol Neurosurg,2023,23(6):566-570. doi:10.3969/j.issn.1672-6731.2023.06.016.
[20] ZHANG S,HE L,YU Y,et al. Effects of pre-operative oral carbohydrates on insulin resistance and postoperative recovery in diabetic patients undergoing coronary artery bypass grafting:study protocol for a prospective, single-blind, randomized controlled trial[J]. Trials,2022,23(1):1067. doi:10.1186/s13063-022-07042-w.
[21] MOUSA S,SAIF A,FATHY M,et al. Assessment of early vascular changes in adult females with polycystic ovary syndrome: correlation with insulin resistance[J]. Gynecol Endocrinol,2023,39(1):2210226. doi:10.1080/09513590.2023.2210226.
[22] LIU J,KONG D,AI D,et al. Insulin resistance enhances binge ethanol-induced liver injury through promoting oxidative stress and up-regulation CYP2E1[J]. Life Sci,2022,303:120681. doi:10.1016/j.lfs.2022.120681.
[23] HAN X D,LI Y J,WANG P,et al. Insulin resistance-varying associations of adiposity indices with cerebral perfusion in older adults:a population-based study[J]. J Nutr Health Aging,2023,27(3):219-227. doi:10.1007/s12603-023-1894-2.
[24] XU J,GAO H,ZHANG L,et al. Melatonin alleviates cognition impairment by antagonizing brain insulin resistance in aged rats fed a high-fat diet[J]. J Pineal Res,2019,67(2):e12584. doi:10.1111/jpi.12584.