Meta analysis and data mining of the method of yishenhuoxue in the treatment of nonproliferative diabetic retinopathy
HOU Xiao-yu, JIE Chuan-hong, WANG Jian-wei, LIU Zi-qiang, DENG Yu, LI Yuan-yuan,CAI Wen-jing
Eye Hospital China Academy of Chinese Medical Sciences, Beijing 100040, China
Keywords:
ABSTRACT Objective: To evaluate the efficacy and safety of the method of Yishen Huoxue in the intervention of nonproliferative diabetic retinopathy(NPDR) by Meta analysis and explore the medication regularity of Chinese Medicine (TCM) based on data mining.Methods: The related literature of TCM in the treatment of NPDR published in CNKI, VIP, WF, PubMed,the Cochrane Library, SinoMed, Embase were collected.The quality of the included literature was evaluated with reference to the Cochrane System Evaluators' Handbook, and statistical analysis was performed by applying Revman 5.4.1 software.After normalization of the Chinese medicine names, association rule analysis was performed by using SPSS Modeler 18,and then Cytoscape was used to produce complex network diagrams.Results: 20 RCTs were included.Meta-analysis results showed that the method of Yishen Huoxue or Yishen Huoxue combined with western medicine were better than the control group in improving the total clinical efficiency[RR= 1.21, 95% CI(1.16, 1.27), P<0.000 01], TCM symptom efficacy[RR= 1.28, 95% CI(1.18, 1.39), P<0.000 01], and visual acuity[MD = 0.11, 95% CI(0.05, 0.17), P= 0.000 1], HDL-C[MD=0.14, 95% CI(0.03, 0.25), P=0.02 ]; reducing the number of fundus hemangiomas[MD=-3.51, 95% CI(-5.73, -1.28), P=0.002], hemorrhagic spot area[MD=-0.70,95% CI(-0.95, -0.46), P<0.000 01], CMT[MD=-35.31, 95% CI(-55.47, -15.14), P= 0.000 6],FBG[MD=-0.39, 95% CI(-0.72, -0.05), P=0.02 ], LDL-C[MD = -0.36, 95% CI(-0.64, -0.08),P=0.01 ], whole high blood viscosity[MD=-0.43, 95% CI(-0.75, -0.12), P=0.006 ], plasma viscosity[MD=-0.36, 95% CI(-0.67, -0.06), P=0.02] and fibrinogen[MD=-0.50, 95% CI(-0.81,-0.19), P=0.002].The differences were statistically significant.The 20 recipes entered involved a total of 70 herbal medicines.It is analyzed that the high-frequency drugs and the core drugsare gou qi, san qi, dan shen, haung qi, sheng di huang, et al.The association rule analysis summarizes the commonly used pairs including: sheng di huang-san qi, sheng di huang - gou qi, et al.Conclusions: Compared with western medicine treatment alone, the method of Yishen Huoxue or Yishen Huoxue combined with western medicine produce better effects , but it still needs to be verified by higher quality clinical studies.
1.Introduction
Diabetic retinopathy (DR) is one of the common microvascular complications in diabetic patients and occurs in about 1/3 of diabetic patients[1].The development of DR is influenced by multiple factors and its pathogenesis is complex.Chronic inflammation, oxidative stress, late glycosylation end-product formation and protein kinase C activation are among the mechanisms that can cause alterations in microvascular function in a sustained hyperglycemic environment[2-4].In the early stage of the disease, patients may have no ocular symptoms, and with the development of lesions,clinical manifestations include decreased visual acuity, distortion of visual objects, floating black shadows in front of the eyes, flashing sensation, and in severe cases, loss of vision.Depending on the severity of the lesion, DR can be divided into nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy(PDR).clinical manifestations of NPDR include retinal microangiomas, hemorrhages, hard exudates, cotton wool spots,and intraretinal microvascular abnormalities[5].patients with NPDR,if not treated promptly, will lead to irreversible visual impairment or even blindness.How to prevent and control the progression of NPDR to PDR and maximize the protection and restoration of vision in patients with DR has been a hot issue of research in the field of ophthalmology.The main treatment strategies for NPDR are controlling risk factors and improving microcirculation, etc[5].Calcium hydroxybenzenesulfonate, one of the commonly used drugs in the treatment of NPDR, can reduce the viscosity of blood,decrease the hyperaggregation of red blood cells, and slow down the leakage of retinal microvessels[6].However, there are still some patients who are not sensitive to calcium hydroxybenzenesulfonate treatment alone[7].
DR belongs to the category of “Shizhanhunmiao”, “Xiaokemubing”and “Yunwuyijing” in Chinese medicine.DR is a disease of the pupil, which is one of the five chakras, the “water chakra”, which is dominated by the kidney.DR is a microvascular disease based on diabetes mellitus, and diabetes mellitus will damage the kidneys over time.If the kidney essence is deficient, the essence does not transform blood, the essence and blood cannot be carried upward,the eyes are not moistened, and the visual function will be affected.Kidney essence turns into kidney qi, kidney qi is divided into yin and yang, and kidney yin and kidney yang are the fundamentals of yin and yang of human internal organs.Deficiency of kidney yin leads to internal heat and depletion of fluid, resulting in blood stasis;deficiency of qi and yin leads to weak blood flow; yin loss and yang deficiency leads to internal cold, resulting in cold clotting and blood stasis, so blood stasis is a pathological factor throughout the DR.Qin Yuhui et al[9] summarized the pathogenesis of DR as “kidney deficiency as the root, yin deficiency as the basis, and blood stasis as the symptom”.Fan Yuzhu et al[10] concluded that the pathogenesis of NPDR is kidney deficiency and blood stasis.Therefore, the treatment should take into account both the symptoms and the root cause, and the main treatment should be to benefit the kidney and brighten the eyes and activate blood stasis.
Chinese medicine therapy has the advantages of multi-target modulation and holistic treatment, and many clinical studies have shown[11-30] that Chinese medicine is effective in the treatment of NPDR, suggesting the promising application of Chinese medicine therapy in the early intervention of DR.A recent Meta-analysis on the treatment of NPDR showed that TCM combined with conventional Western medicine treatment was more effective in improving retinal microangioma, hemorrhage, central macular concavity thickness (CMT), visual acuity, fasting blood glucose(FBG) and glycated hemoglobin (HbAlc) compared with conventional Western medicine treatment alone[31].However, there is no evaluation of the therapeutic efficacy and safety of the Yiku Renju method as an adjuvant treatment for NPDR.Therefore, the aim of this study was to evaluate the improvement of symptoms and signs and the safety of the Yi Kidney Blood Activation Method in patients with NPDR in order to provide high-quality evidence-based evidence to help clinicians choose a better treatment strategy.
2.Information and methods
2.1 Meta-analysis
2.1.1 Literature search
Computer search of relevant Chinese medicine for nonproliferative diabetes mellitus included in the Chinese journal fulltext database (CNKI), VIP database (VIP), Wanfang database(WF) and Chinese biomedical literature databases PubMed, the Cochrane Library, SinoMed, Embase Chinese and English medical databases The literature of retinopathy.The search period was from database creation to October 2022.The Chinese search terms included “diabetic retinopathy”, “Chinese medicine”, “Chinese herbal medicine”, “ Chinese medicine”, “benefit the kidney”,“tonify the kidney”, “invigorate blood”, “remove blood stasis”,“randomized controlled trial”; English search terms include “diabetic retinopathy”, “Tradit Chin Med”, “Bushen Huoxue”, “activating blood”, “ removing blood stasis”, “randomized controlled trials”.
2.1.2Inclusion criteria of the literature
①The type of study was a randomized controlled trial (RCT);②The study subjects were patients with NPDR who met the criteria for NPDR in the Staging Criteria for Diabetic Retinopathy[32] adopted by the Third National Ophthalmology Conference in 1985 by fundoscopy and fluorescein sodium fundus angiography;③Interventions: the test group used Chinese medicine to benefit the kidney and activate blood (Tradit Chin Med soup, Chinese medicine granules or Chinese patent medicine, etc.) oral treatment mainly combined with glucose lowering and other western medicine basic treatment, or combined with calcium hydroxybenzenesulfonate calcium benzoate capsules.In the control group, calcium benzene sulfonate capsules with calcium hydroxybenzene sulfonate combined with glucose lowering and other basic Western medicine treatment;the course of treatment for both groups 1 month.
2.1.3 Outcome index
The total clinical efficiency was the primary outcome; the efficacy of TCM symptoms, visual acuity, CMT, number of microangiomas,bleeding spot area, blood glucose index, blood rheology, lipid metabolism index and incidence of adverse reactions were secondary outcome indexes.
2.1.4 Exclusion criteria
Any of the following were excluded: (i) less than 20 cases in the clinical trial; (ii) conference and supplemental literature; (iii)the Chinese medicine compound used was not labeled with the ingredients; (iv) the combination of TCM external treatment methods such as introduction, acupressure, acupuncture, etc.or the treatment principle did not reflect the method to benefit the kidney and activate blood; (v) the use of laser treatment or surgery and other treatments;(vi) only one duplicate literature was retained.
2.1.5 Literature screening and data extraction
Duplicate literature was found and removed by 2 investigators through literature management software respectively, then the titles and abstracts of the literature were read for initial screening according to the inclusion and exclusion criteria mentioned above,and finally the full text was read for secondary censoring.The data were extracted from the included studies and an Excel database was created, including authors and publication dates, sample size,interventions, outcome indicators, adverse effects, and duration of treatment.The literature screening and data extraction process required cross-checking by 2 investigators, and any disagreement could be discussed or sought to be resolved by a third investigator.
2.1.6 Quality assessment and risk of bias assessment
The quality and risk of bias of the included studies were assessed by two investigators independently using the tools recommended in the Cochrane systematic reviewers’ handbook 5.3.Any disagreements were resolved through discussion or with the assistance of a third investigator.The main items evaluated included: ①about the randomization grouping; ②allocation concealment during randomization; ③whether blinding was used; ④ selective reporting of study results; ⑤case loss and withdrawal; and ⑥other biases.
2.1.7Statistical analysis
The data were counted and analyzed using the systematic evaluation software RevMan 5.4 from the International Collaborative Network for Evidence-Based Medicine, and forest plots were made.The relative risk ratio (RR ) or ratio of ratios (OR) was used as the effect statistic for the count data.The mean difference (MD) or standardized mean difference (SMD) was used as the effect statistic for the measurement data, both providing their 95% confidence interval CI.χ2test was first used to test for heterogeneity, and whenP>0.05 orI250%, the fixed-effect model was selected; whenP<0.05 or I2> 50%, the source of heterogeneity was analyzed, and the sensitivity of the outcome indicators was performed by excluding the single literature one by one.P<0.05 was considered a statistically significant difference.A funnel plot was also used for publication bias detection.
2.2 Data mining
2.2.1 Data extraction
The composition of the Chinese herbal compounds finally included in the literature was entered into Excel to establish a database, and the names of the Chinese herbal medicines were standardized.The names of the Chinese medicines were standardized with reference to the relevant contents of the Pharmacopoeia of the People’s Republic of China (2020 edition)[33], for example, “Shengqi” was unified as“Huangqi”; “Dried Lotus Grass For example, “Astragalus” was unified as “Astragalus”; “Dry Lotus Herb” was unified as “Mo Dry Lotus”, etc.
2.2.2 Statistical methods
SPSS Modeler 18 was used for association rule analysis, and Apriori algorithm nodes were selected for modeling, while support 0.1, confidence 0.8, and elevation 1 were set to analyze the relationship of Chinese herbal medicine pairings.Then complex network analysis was performed on the basis of association rule analysis, and the data were imported into Cytoscape to produce complex network graphs.
3.Results
3.1 Literature search results
According to the search strategy developed above, 695 relevant literature were retrieved, 450 by CNKI, 178 by WF, 36 by VIP 20 by CBM, 0 by PubMed, 0 by Embase, 11 by the Cochrane Library, and 0 by other resources.After checking, 84 literature were excluded,287 literature were deleted according to the abstract and title, 304 literature were deleted according to the inclusion and exclusion criteria, and 20[11-30] literature were finally included, with the year of publication from 2011 to 2022.The literature screening process is shown in Figure 1.

Fig 1 Flow chart of literature screening
3.2 Basic characteristics of the included literature and quality assessment results
Twenty RCTs containing 2263 patients with NPDR were finally included, with a total of 1138 cases in the trial group and 1125 cases in the control group.There were 15 papers using the Yiken method combined with calcium hydroxybenzenesulfonate [11,12,15-24,26,28,30] and 5 papers using the Yiken method alone[13,14,25,27,29],and the table of literature characteristics is shown in Table 1.bias analysis of the 20 randomized controlled trials using the Cochrane risk bias assessment tool, there were no statistically different,balanced at baseline, and comparable; 12 [11,12,14-18,22,23,25,26,28]studies utilized the randomized number table method, 1 [25] study used randomized parallel controls, and 8[13,19-21,24,27,29,30]studies mentioned randomization only; 1[25] was single-blinded; a modified version of the Jadad scale was used to score the included literature,of which 2 were of high quality (4 and above) and 18 were of low quality: 10 with a score of 3 and 8 with a score of 2; controlling for implementation bias and measurement bias, data from all studies were complete, there was no selective reporting, and no other bias possibilities were identified.The risk of bias for the included studies is shown in Figure 2.

Tab 1 Table of basic characteristics of the included literature
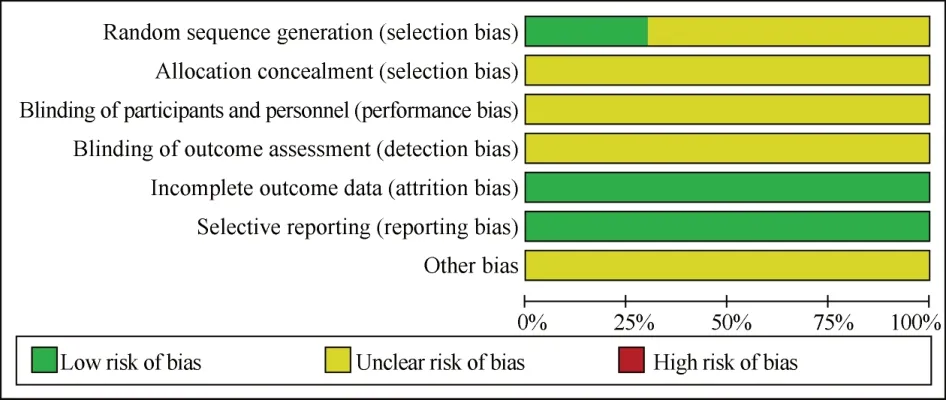
Fig 2 Percentage of items at risk of bias included in the study
3.3 Meta-analysis
3.3.1 Total clinical efficiency
A total of 14 papers[11-15,17-20,22,23,26,29,30] reported the total clinical efficiency, and the results of the heterogeneity test showed that P=0.48, I2= 0%, and the data were combined using a fixedeffects model.The results of the Meta-analysis: compared with the control group, the Yi kidney activation method alone or combined with calcium hydroxybenzenesulfonate could improve the total clinical effectiveness [RR=1.19, 95%CI(1.14, 1.25),P<0.000 01].In a subgroup analysis, 11 papers[11,12,15,17-20,22,23,26,30] showed that the combination of calcium hydroxybenzenesulfonate in the experimental group with kidney activation method was associated with higher total clinical efficiency compared with calcium hydroxybenzenesulfonate alone [RR = 1.19, 95% CI (1.14, 1.26) P<0.000 01].3 papers[13,14,29] showed that the total clinical efficiency was higher in the group treated with kidney activation method alone compared with calcium hydroxybenzenesulfonate treatment alone[RR=1.19, 95% CI (1.09, 1.30), P<0.000 01], as shown in Figure 3.5 papers[16,21,22,22] showed that the total clinical efficiency was higher in the group treated with kidney activation method combined with calcium hydroxybenzenesulfonate treatment [RR=1.19, 95%CI (1.14, 1.26),P<0.000 01].[16,21,22,24,28] reported the efficacy of TCM syndromes, and the test groups were all treated with the Beneficial Kidney Activation Method combined with calcium hydroxybenzenesulfonate, and the results of the heterogeneity test showed that P=0.67 and I2= 0%, so the data were combined using a fixed-effect model, and the results of the Meta-analysis showed that[RR=1.28, 95%CI(1.18, 1.39),P<0.000 01], and the difference was statistically significant when comparing between groups, indicating that the combination of kidney benefit and blood activation method with calcium hydroxybenzenesulfonate treatment was superior to calcium hydroxybenzenesulfonate treatment alone in improving the efficacy of TCM symptoms, as shown in Figure 4.
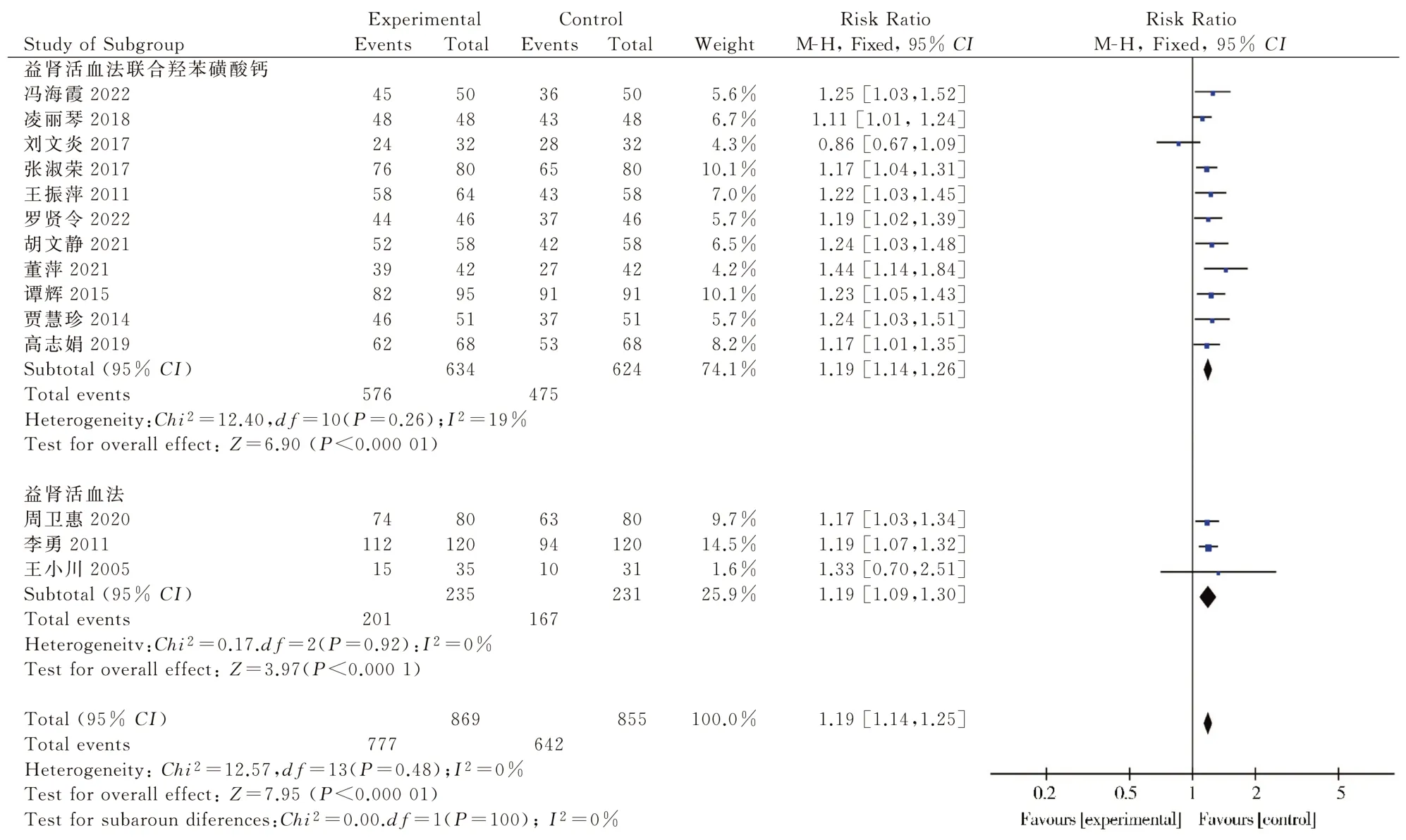
Fig 3 Forest plot of Meta-analysis of total clinical efficiency
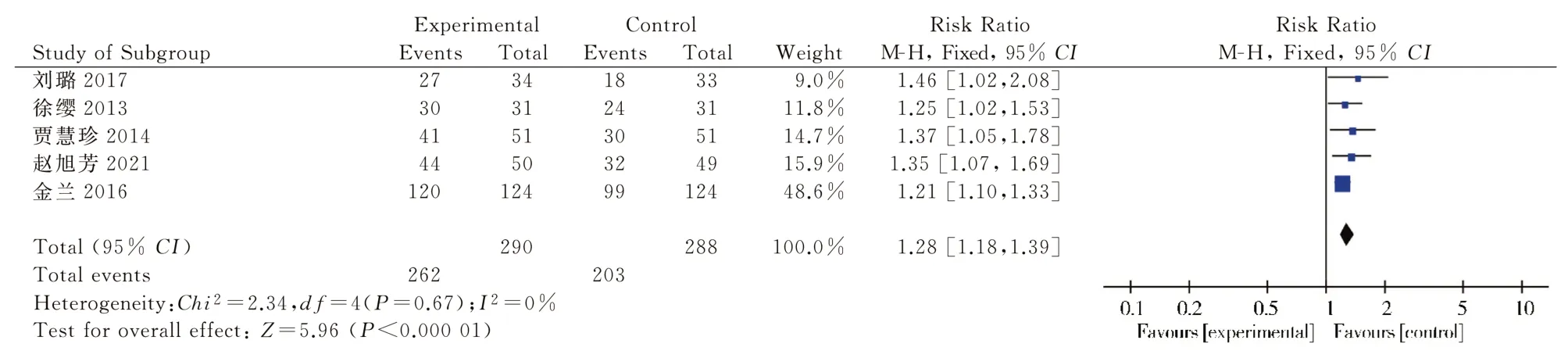
Fig 4 Meta-analysis forest plot of the efficacy of TCM syndromes
3.3.2 Visual acuity and CMT
Five[14,16,17,22,25] publications reported visual acuity, with heterogeneity test results showing P=0.01, I2=70%, and analysis of combined random-effects model data showed that Yiku Renju method alone or in combination with calcium hydroxybenzenesulfonate improved patients’ visual acuity compared with controls [MD=0.11, 95% CI (0.05, 0.17 ), P=0.000 1].A subgroup analysis showed that three[16,17,22] trial groups of the literature used the Kidney and Blood method combined with calcium hydroxybenzenesulfonate, and a random-effects model analysis of the combined data showed that the Kidney and Blood method combined with calcium hydroxybenzenesulfonate treatment was superior to the control group in improving visual acuity [MD= 0.09, 95%CI(0.05, 0.12),P<0.00001].two[14,25] trial groups of the literature used the Kidney and Blood method alone to improve visual acuity [MD=0.11, 95% CI (0.05, 0.17), P = 0.000 1].Five[12,15,17,18,22] papers reported CMT, and the trial groups were all treated with the Kidney and Blood method in combination with calcium hydroxybenzenesulfonate [MD = 0.15, 95% CI (0.02, 0.17),P=0.02].The heterogeneity test showed that P<0.000 01, I2= 99%,and the analysis of the combined random-effects model data showed that [MD=-35.31, 95% CI (-55.47, -15.14), P = 0.0006], and the difference was statistically significant when comparing between groups, indicating that treatment with the Yi Kidney Revitalization Method combined with calcium hydroxybenzenesulfonate was superior to Western medicine treatment alone, see Figure 6.
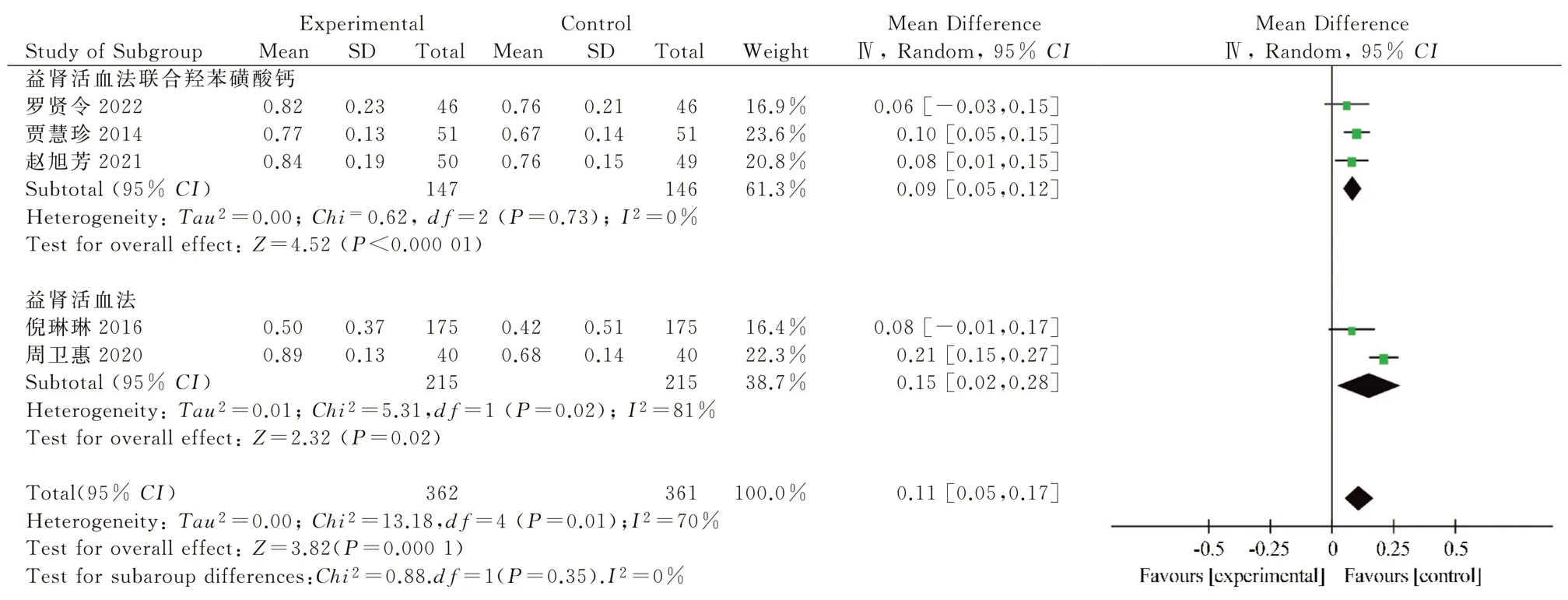
Fig 5 Meta-analysis forest plot of visual acuity

Fig 6 Meta-analysis forest plot of CMT
3.3.3 Microangiomas and hemorrhagic spots
Four[12,15,19,20] publications reported microangiomas, and all of the trial groups were treated with the Beneficial Kidney and Blood Activation method combined with calcium hydroxybenzenesulfonate,and the heterogeneity test showed thatP<0.000 01,I2=99%, and the analysis of the combined random-effects model data showed that[MD=-3.51, 95%CI(-5.73, - 1.28),P= 0.002], and the difference was statistically significant when compared between groups, see Figure 7.four[12,15,17,19] papers reported on the fundus efficacy of hemorrhagic spot area, and the test groups were all treated with the beneficial renal activation method combined with calcium hydroxybenzenesulfonate, and the heterogeneity test showed: P<0.00001,I2=97%, and the random-effects model data combined analysis showed: [MD= -0.70, 95%CI(-0.95, -0.46),P<0.000 01],and the difference was statistically significant when comparing between groups, indicating that the combination of the yi kidney and blood activation method with calcium hydroxybenzenesulfonate was superior to western drug treatment alone in reducing fundus hemangioma and hemorrhage, as shown in Figure 8.
Just in time, the grandfather stopped himself from saying there was no such thing as a doughnut seed. Looking at the unhappy little face, he suddenly got an inspiration.
3.3.4 Glucose and lipid metabolic indexes and blood rheology
The analysis showed that the test group was better than the control group in improving fasting glucose, blood rheology (high cut whole blood viscosity, fibrinogen and plasma specific viscosity), and lipid metabolism (HDL-C, LDL-C) with statistically significant differences (P<0.05), as shown in Table 2.
Fig 7 Meta-analysis forest plot of the number of microvascular tumors
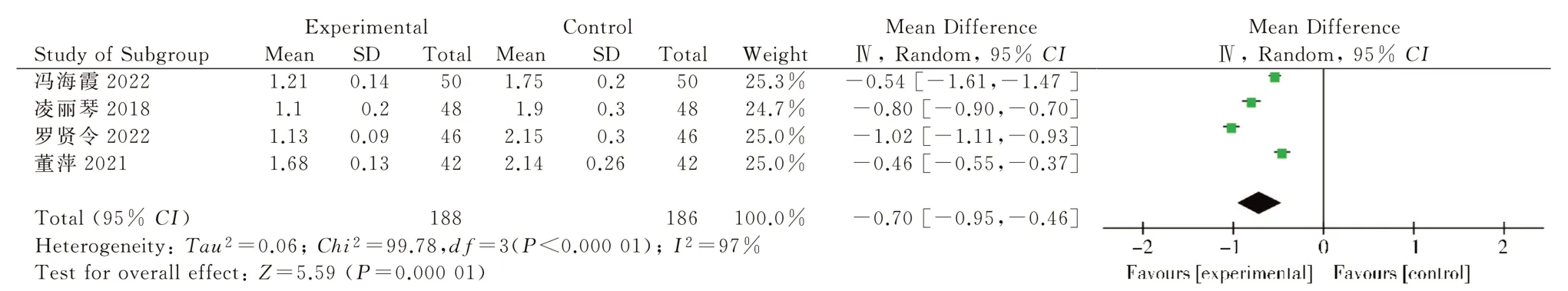
Fig 8 Meta-analysis forest plot of hemorrhagic spot area
Six[16-18,20,28,29] papers reported fasting blood glucose, and the heterogeneity test showed thatP<0.000 01,I2= 90%, and the analysis after combining data from the random-effects model showed that Yiken and Blood method alone or combined with calcium hydroxybenzenesulfonate was more effective in reducing fasting blood glucose in patients compared with controls [MD = -0.38, 95%CI(-0.70, - 0.05),P= 0.02].
Five[16,23,25,27,28] papers reported changes in HDL-C, with heterogeneity tests showing P<0.000 01, I2= 96%, and a randomeffects model for data merging showed that the beneficial kidney activation method alone or in combination with calcium hydroxybenzenesulfonate increased HDL-C levels in patients compared with controls [MD=0.14, 95%CI(0.03, Six papers[16,17,23,25,27,28] reported changes in LDL-C, with heterogeneity test results showing P<0.000 01, I2= 94%, and combined random-effects model data showed that Yixing Renal Activation Method alone or in combination with calcium hydroxybenzenesulfonate reduced LDL-C in patients compared with controls [MD =-0.36, 95% CI (-0.64,-0.08),P=0.01].
Five[11,19,26,28,30] papers reported on whole blood hyperviscosity,and the trial group was treated with the beneficial renal activation method combined with calcium hydroxybenzenesulfonate, and the results of the heterogeneity test showed that P<0.01, I2=87%, and the data were combined using a random-effects model, and the Metaanalysis showed that [MD=-0.43, 95%CI(-0.75, -0.12)P=0.006],a statistically significant difference.It indicates that the treatment with the method of revitalizing the kidney and blood in combination with calcium hydroxybenzenesulfonate is more effective in reducing whole blood hypercut viscosity compared with the treatment with western medicine alone.five[11,18,26,28,30] papers reported plasma viscosity, and the test group was treated with the method of revitalizing the kidney and blood in combination with calcium hydroxybenzenesulfonate, and the results of the heterogeneity test showed that:P<0.01,I2=97%, and the data were combined using a random-effects model.Meta-analysis showed that [MD =-0.36, 95% CI(-0.67, -0.06), P=0.02], with statistically significant differences.This indicates that treatment with the renal activation method combined with calcium hydroxybenzenesulfonate is more effective in reducing plasma viscosity compared with treatment with Western drugs alone.three[11,19,30] papers reported fibrinogen, and the trial groups were all treated with the renal activation method combined with calcium hydroxybenzenesulfonate, and the results of the heterogeneity test showed: P<0.01, I2= 94%, and the data were combined using a random-effects model, and Meta-analysis The results showed that [MD=-0.50, 95% CI(-0.81, -0.19), P=0.002], with a statistically significant difference.This indicates that treatment with the Beneficial Kidney Activation Method combined with calcium hydroxybenzenesulfonate is more effective in reducing fibrinogen compared to treatment with Western medicine alone.
3.3.5 Incidence of adverse reactions
Three papers[15,17,28] reported the occurrence of adverse reactions during the treatment process, and the test group was treated with the beneficial kidney and blood activation method combined with calcium hydroxybenzenesulfonate.1 paper reported[17] that the incidence of reactions was 8.70% in the test group and 10.87% in the control group, and the difference was not statistically significant when comparing the two groups (P>0.05).Another report[28]reported no uncomfortable reactions in the treatment group from the start of the drug to the end of the course of treatment, and one case of mild gastric discomfort in the control group patients, who did not stop the treatment, while the symptoms gradually disappeared.The results of the heterogeneity test showed that P=0.67, I2=0%,so a fixed-effects model was used, and the Meta-analysis showed that [RR=0.48, 95%CI(0.19, 1.21),P=0.12], with no statistically significant differences when compared between groups, indicating that the safety of the test and control groups was comparable and did not increase the occurrence of adverse reactions, as shown in Figure 9.
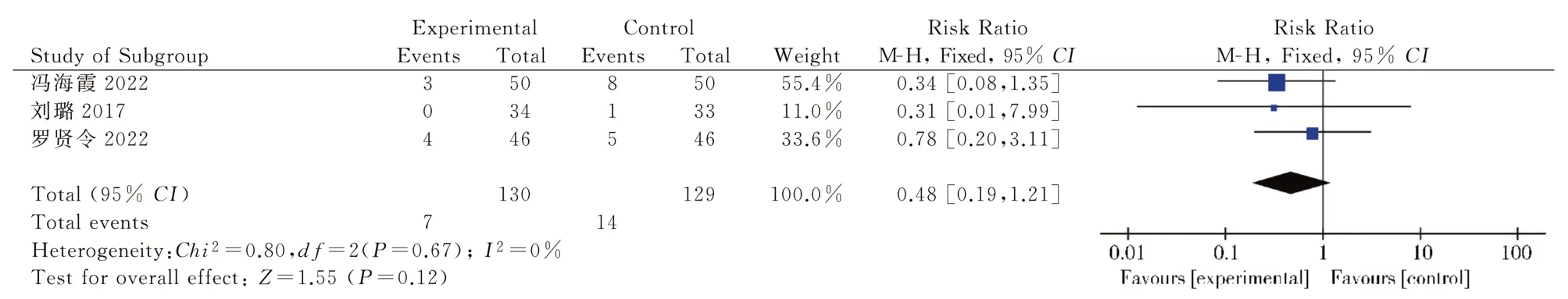
Fig 9 Meta-analysis forest plot of the incidence of adverse reactions
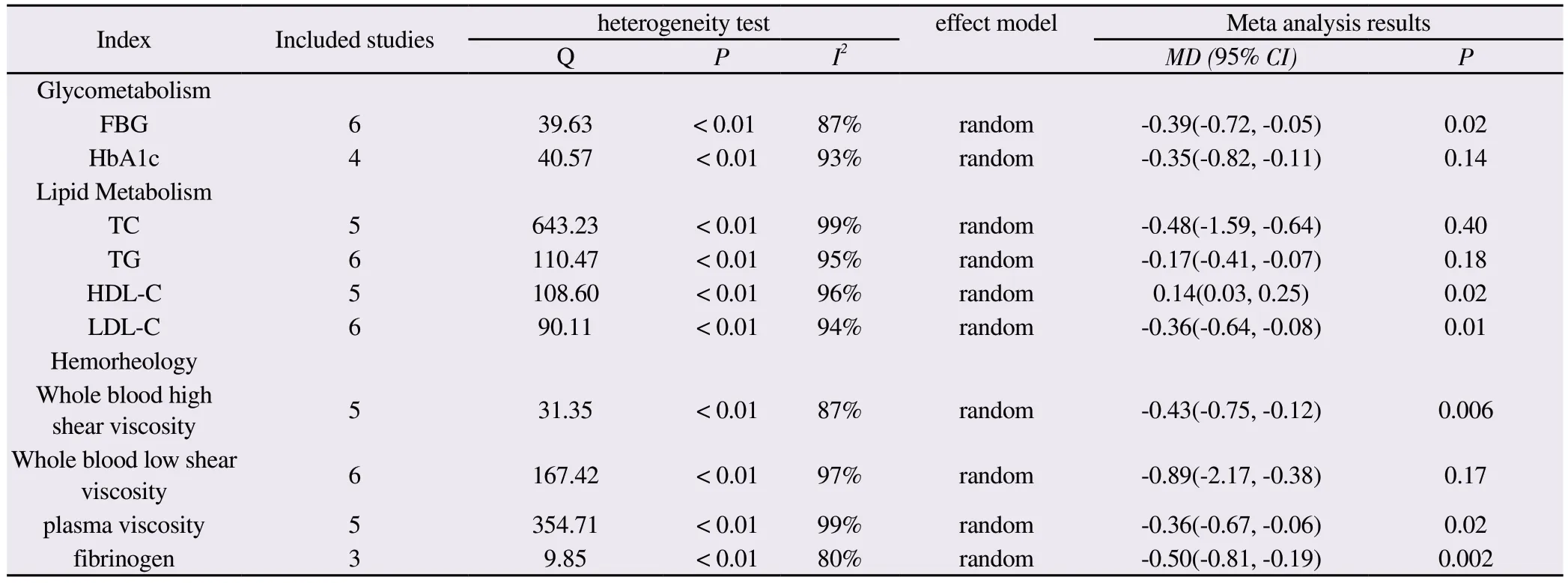
Tab 2 Meta-analysis of glycolipid metabolic indexes and blood rheology between the two groups
3.4 Publication bias analysis and sensitivity analysis
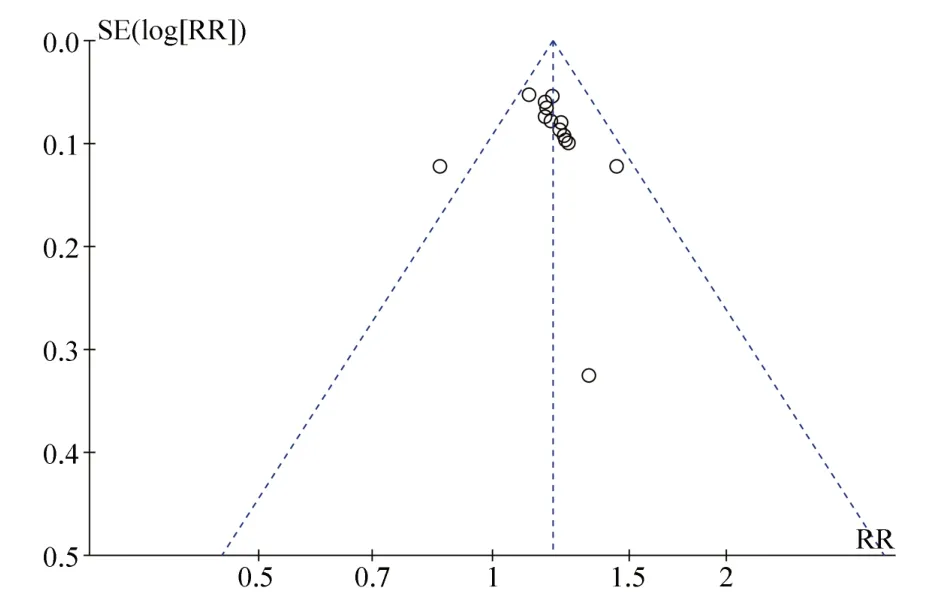
Fig 10 Publication bias funnel plot for total clinical effectiveness
3.5 Data mining
3.5.1 High-frequency drugs
The drug frequency statistics were conducted for the herbal compound prescriptions in the final 20 included papers, involving a total of 70 herbal medicines with a total of 456 occurrences.The top 12 drugs were: Fructus Lycii, Panax notoginseng, Salvia miltiorrhiza, Radix Astragali, Radix et Rhizoma Dioscoreae, Radix Angelicae Sinensis, Radix et Rhizoma Paeoniae, Radix Puerariae Sinensis, Radix cassiae Sinensis, Cornus officinalis, and Radix et Rhizoma Mojirae, which were mainly used to benefit the kidney and invigorate blood, see Figure 11.
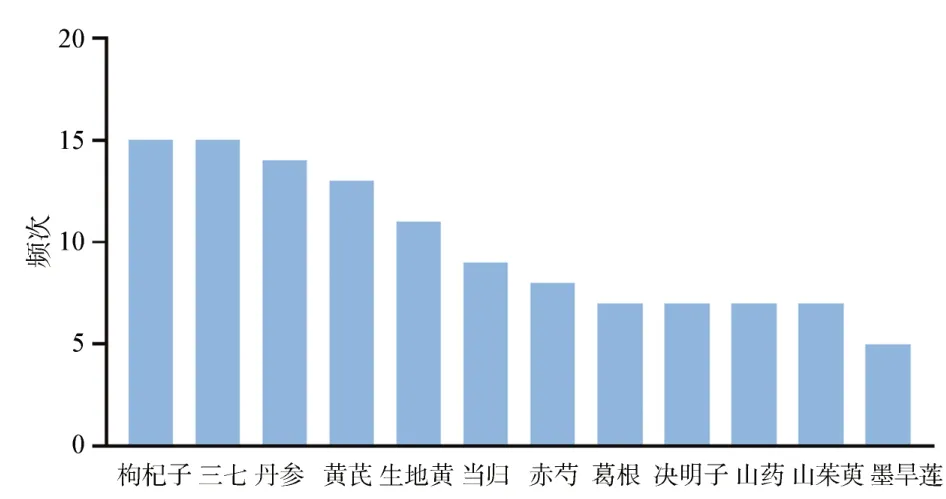
Fig 11 High frequency drug distribution map
3.5.2 Association rule analysis
The association rule analysis was performed using SPSS Modeler 18 for the high-frequency drugs involved in the literature, and the Apriori algorithm nodes were selected for modeling, while setting the support 0.1, confidence 0.8, and boost 1.10 association rules for two drugs and 18 association rules for three drugs were obtained,as shown in Table 3.
3.5.3 Complex network diagram
Based on the association rule analysis, complex network analysis was performed, and the data were imported into Cytoscape for complex network analysis to obtain the core drug groups, see Figure 12.nodes represent drugs, and lines represent the relationships between drugs.The larger the nodes and the darker the color, the higher the frequency of drug occurrence; the darker the color of the lines, the stronger the connection between drugs.
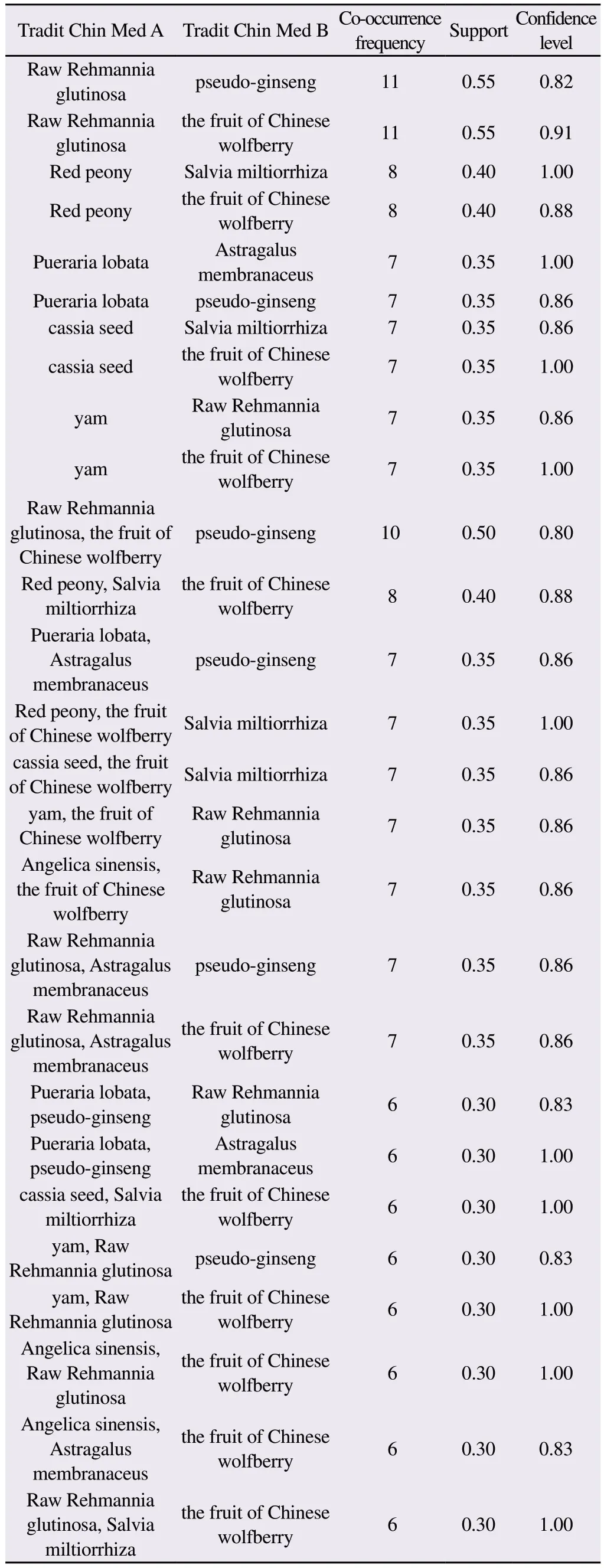
Tab 3 Chinese medicine association rule analysis table
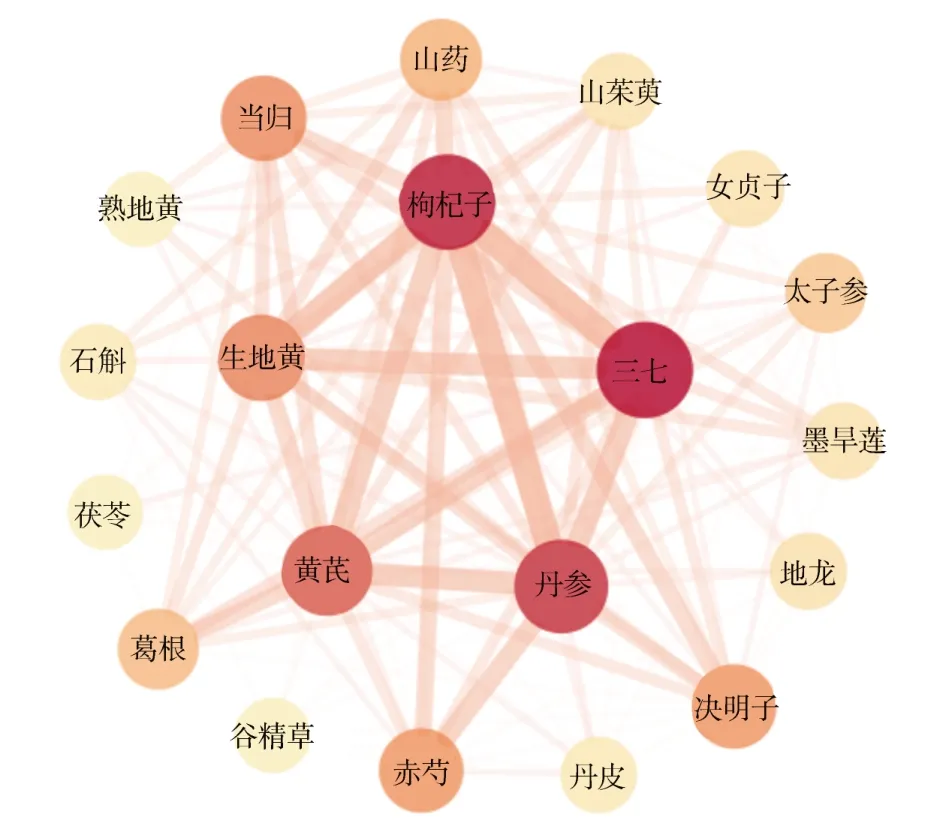
Fig 12 Complex network diagram of Chinese medicine
4.Discussion
The prevention and treatment of DR remains a global public health issue to this day.During the progression of NDPR to PDR stage, the deterioration of visual function and the consequent retinal neovascularization, vitreous hemorrhage, retinal detachment and other fundus changes not only seriously affect the quality of life of patients but also bring great economic burden to patients.In the NPDR stage, effective interventions can slow down the progression of the disease.A related clinical study[33] showed that the clinical efficacy of kidney tonifying, blood activating and eye brightening herbs in treating DR patients was significant, which could improve visual acuity, lower patients’ blood glucose, reduce inflammatory reactions and at the same time reduce the adverse effects of treatment.Xie Xuejun et al[34] found in in vitro experiments that tonic kidney and blood activating herbs may act against DR through mechanisms such as increasing the stability of cell membranes of retinal Müller cells in a high-glucose environment and inhibiting VEGF protein expression.Wang Duxin et al[35] found that in a rat model of DR, the herbal compound for tonifying the kidney and invigorating blood could alleviate retinal vascular leakage caused by damage to the blood-retinal inner barrier.
The purpose of the Meta-analysis in this study was to evaluate the efficacy and safety of the method of tonifying the kidney and invigorating blood as a treatment for NPDR, and the evaluation indexes included total clinical efficiency, visual acuity, and glycolipid metabolism.A total of 20 studies with 2263 patients were included.The results of the efficacy analysis showed that the total clinical efficacy rate of the Yiken Blood Activation Method alone or in combination with calcium hydroxybenzenesulfonate treatment was higher than that of Western medicine treatment alone, and it was effective in improving visual acuity, TCM symptoms, fundus condition, CMT, fasting glucose, blood flow,and lipoproteins.Hyperglycemia is the main causative factor of DR, and controlling blood glucose is the key link in the prevention and treatment of DR.Dyslipidemia is also one of the systemic risk factors aggravating DR.A study[36] found that early lipid-lowering drugs in diabetic patients can reduce retinal lipid accumulation,which is beneficial to reduce retinal exudation, alleviate macular edema, improve visual acuity, and delay the progression of DR.Disturbances in glucolipid metabolism can cause abnormal blood rheology and increased blood flow resistance, causing ischemia and hypoxia and microcirculatory disorders in retinal tissues[37].The improvement of blood glucose, blood lipids, and blood rheology indexes in patients treated with renal activation method combined with calcium hydroxybenzenesulfonate is beneficial to further stabilize the systemic microvascular circulation and delay the progression of NPDR.Further analysis of the dosing pattern of the beneficial kidney and blood activation method in the treatment of non-proliferative diabetic retinopathy revealed that the highfrequency drugs and core drugs include Lycium barbarum, Panax ginseng, Salvia miltiorrhiza, Radix Astragali, and Radix et Rhizoma Polygonati, and the commonly used pairs include: Radix et Rhizoma Polygonati-Sanji and Radix et Rhizoma Polygonati-Lycium barbarum.Lycium barbarum has the function of nourishing the liver and kidney, benefiting the essence and brightening the eyes.Panax ginseng and Salvia miltiorrhiza can nourish the blood and invigorate it, stop bleeding and resolve blood stasis.Astragalus has the effect of nourishing the middle and benefiting the qi, strengthening the spleen and benefiting the lung.The Tang Liquid Materia Medica says: “(Huang Qi) also treats typhoid fever, the ulnar pulse does not arrive, and nourishes the kidney vital energy.” Shengdi is a medicine for clearing heat and cooling the blood, and “Ben Cao Feng Yuan”says: “In cases of yin deficiency and fire, it is appropriate to nourish yin and subdue yang.” The combination of these drugs can benefit the essence and brighten the eyes, nourish yin and cool the blood,invigorate blood circulation and eliminate blood stasis, and achieve the treatment of both the symptoms and the root cause.
Limitations and shortcomings of this study: (1) all 20 included RCTs mentioned randomized control, only 12[11,12,14-18,22,23,25,26,28]gave specific randomization methods, none of the literature described the specific method of random assignment concealment,and only one[25] article mentioned blinded method; (2) the index detection methods used in each clinical study had some (2) the methods used in each clinical study had some deviations or were influenced by the instruments, reagents, environment, and operator proficiency, such as the detection of indicators such as blood rheology and lipid metabolism levels; (3) differences in sample size,differences in the grouping, dose, and dosage form of the Chinese medicine taken, and differences in the duration of the patient’s illness as well as the course of treatment may all have an impact on the outcome indicators.(4) The lack of long-term follow-up in the included studies led to insufficient evidence on the long-term efficacy, recurrence and safety evaluation of the drugs in question.
In conclusion, the beneficial kidney and blood activation method alone or in combination with western medicine can improve visual acuity, TCM symptoms, fundus condition, fasting glucose, blood flow and low-density lipoprotein in patients with NPDR, delay the progression of the disease, treat both symptoms and root causes,and have a good safety profile.However, due to the varying quality of the included literature and sample size differences, the evidencebased medical evidence is insufficient.In the future, we should strictly standardize the trial design and implementation of clinical trials, adopt standardized and unified diagnostic criteria and efficacy evaluation criteria, and conduct randomized double-blind controlled trials with large samples for further validation.
Conflict of interest statement
There is no conflict of interest.
Authors’ contribution
The first author, Xiaoyu Hou, was responsible for writing the article; ZQ Liu and JW Wang were responsible for literature screening; Yu Deng assisted in extracting literature information; and the corresponding author, Chuanhong Rece, was responsible for the selection, design and review of the article.
 Journal of Hainan Medical College2023年20期
Journal of Hainan Medical College2023年20期
- Journal of Hainan Medical College的其它文章
- Antibiotic resistance analysis and coping strategies of helicobacter pylori
- Evaluation of the diagnostic value of total bile acids/platelets in HBV related liver fibrosis
- Discover the key genes for glomerular inflammation in patients with type II diabetic nephropathy based on bioinformatics and network pharmacology
- Evaluation of the diagnostic efficacy of noninvasive diagnosis in patients with chronic viral hepatitis B complicated with nonalcoholic fatty liver disease and significant liver fibrosis
- Analysis of E2F3 gene variants, expression and clinical significance in melanoma based on multiple databases
- Epidemiological characteristics of hyperuricemia in metabolic syndrome and its different components in the physical examination population
