Incidence and risk factors of in-hospital venous thromboembolism in non-oncological urological inpatients: A single center experience
Zho Wng , Kixun Li , Qun Zhu , Hozhen Li ,Ziqing Wu , Xuesong Liu , Zhengyn Tng ,b,*
a Department of Urology, Xiangya Hospital, Central South University, Changsha, China
b Provincial Laboratory for Diagnosis and Treatment of Genitourinary System Disease,Changsha,China
KEYWORDS Venous thromboembolism;Non-oncological surgery;Urological inpatient;Incidence;Risk factor
Abstract Objective: To determine incidence and risk factors for venous thromboembolism(VTE) development of in-hospital VTE in urological inpatients who underwent non-oncological surgery in a tertiary hospital in China.Methods: Consecutive 1453 inpatients who were admitted to a non-oncological urological ward in the tertiary hospital from January 1,2018 to December 31,2018 were enrolled in the study,and the VTE events were diagnosed by ultrasound or computed tomographic pulmonary angiography.Patients’ occurrence of VTE and characteristics which may contribute to the development of VTE were collected and analyzed as incidence and risk factors.Results: The incidence of VTE in non-oncological urological inpatients is 2.3%.In our cohort,patients whoexperiencedpreviousVTE(adjustedoddsratios[aOR]14.272,95%CI3.620-56.275),taking anticoagulants or antiplatelet agents before admission(aOR 10.181,95%CI 2.453-42.256),D-dimer(max)≥1 μg/mL(aOR 22.456,95%CI 6.468-77.967),lower extremity swelling(aOR 10.264,95%CI 2.242-46.994),chest symptoms(aOR 79.182,95%CI 7.132-879.076),operation time of more than or equal to 180 min(aOR 10.690,95%CI 1.356-84.300),and Caprini score(max)of more than or equal to 5(aOR 34.241,95%CI 1.831-640.235)were considered as risk factors for VTE.Conclusion: In this study,we found that the incidence of VTE in non-oncological surgery was about 2.3%,which was higher than some previous studies.Risk factors could be used for early detection and diagnosis of VTE.
1.Introduction
Venous thromboembolism (VTE) consists of deep vein thrombosis (DVT) and pulmonary embolism (PE).VTE is a high-risk condition during perioperative, even 1-3 months after surgeries, which can cause adverse health results or even increase lethality [1].Recent years, attention has been paid to VTE by medical teams in many specialties,especially in the fields of orthopedics and oncology [1-4].
Urological surgeries are involved with different operative approaches and different operative positions.In addition, some surgeries,such as transurethral resection of the prostate and radical prostatectomy are more common in elderly, who are always accompanied with comorbidities.Some are secondary to previous multiple injuries or complicated surgeries, such as urethral injury or ureteral stricture.Moreover,it is difficult to balance the risk of VTE or bleeding in some urological surgeries.Therefore, it is difficult to make a decision on thromboprophylaxis or active surveillance in some conditions.
The Caprini risk assessment model (RAM) was invented by Caprini[5].It has been recommended for evaluating the risk of VTE for non-orthopedic surgical patients in 2012.The score is based on the risk of the risk factors.The cumulative score of each patient was calculated to stratify the patients for VTE risk.For patients with a very low-risk VTE (Caprini score of 0),additional prevention is not recommended.For patients with low-risk VTE (Caprini score of 1-2), mechanical or drug prevention is recommended.Patients with intermediate-risk VTE (Caprini score of 3-4) to high-risk(Caprini score of ≥5) are recommended for anticoagulant alone or combined with mechanical prevention.There are a number of assessment schemes for evaluating the risk of VTE, including Kucher score [6], Padua score [7], Wells score[8],and others.The Caprini RAM is suggested for nonorthopedic surgical patients.The Padua RAM is recommended to be used in internal medical patients for VTE risk assessment.Furthermore, several clinical studies in China demonstrated that Caprini RAM is more applicable to Chinese than other risk assessments [9].
The European Association of Urology and Canadian Urological Association published guidelines on perioperative thromboprophylaxis in recent years [10,11].These two guidelines provide some clues about procedure-specific thromboprophylaxis in oncological and non-oncological urological surgery.However, many recommendations for non-oncological urological surgeries are weak according to the guidelines [10,11].Therefore, the evidence of the incidence and risk factors of VTE in non-oncological urological procedures is desiderate to draft new recommendations for thromboprophylaxis.
Hence, this retrospective study was to preliminarily investigate the incidence of in-hospital VTE in non-oncological urological inpatients, regardless of preoperative or postoperative, and symptomatic or asymptomatic.Risk factors would also be studied in this study.
2.Patients and methods
This was a retrospective, single-center, cohort study in a tertiary hospital.It was approved by the Ethics Committee of Xiangya Hospital(2019030078).This trial was retrospectively registered at http://www.chictr.org.cn/index.aspx under the public title “The incidence, risk factors and establishment of prediction model for VTE in urological inpatients” with a code ChiCTR1900027180 on November 3,2019 (specific URL to the registration web page: http://www.chictr.org.cn/showproj.aspx?proj=44677).
There were 1453 consecutive inpatients who were admitted to a non-oncological urological ward in the tertiary hospital from January 1,2018 to December 31,2018 that were enrolled in the study.Most of the patients(92.2%)underwent surgery.In-hospital VTE events were defined as PE or DVT,which were revealed by imaging procedure(such as computed tomography pulmonary angiography and ultrasound)[1].Once the patient was diagnosed with VTE, the in-hospital VTE consultation group would comprehensively evaluate the patient to formulate a personalized treatment plan according to the guidelines.The treatment plan was generally mechanical therapy, and only a few patients would receive anticoagulants.The exclusion criteria of the study were patients: (a)with age below 18 years old;(b)that underwent surgeries to remove urological cancers during the current admission; (c)whose postoperative pathological examination showed malignancies;(d)whose medical record was incomplete.
Data were retrospectively collected from Electronic Medical Record System so the whole research is non-invasive.The following data need to be collected before surgery: gender, age, body mass index (BMI), previous medical history (such as hypertension, diabetes mellitus, history of chronic obstructive pulmonary disease,cardiovascular diseases, cerebrovascular diseases, any surgeries within 1 month,VTE history,and sepsis according to the sepsis-3 definition [11] within 1 month), whether to take anticoagulants or antiplatelet agents, D-dimer, and Caprini score.Low extremity ultrasound would be performed for whom with abnormal preoperative D-dimer or with preoperative Caprini score of more than or equal to 5.
If a patient was screened with VTE, in-hospital VTE consultation group would evaluate the condition and make the treatment plan (underwent operation or underwent anticoagulant therapy before surgery).
Other perioperative data were also collected: American Society of Anesthesiologist (ASA) classification, duration of surgery, and blood loss.Postoperative D-dimer and preoperative Caprini score were also investigated if the data could be obtained from Electronic Medical Record System.Postoperative low extremity ultrasound or lung computed tomography scan was prescribed according to operation conditions, length of bed rest time, D-dimer, Caprini score,and lower extremities and respiratory symptoms.
All statistics analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).Frequencies and percentages were applied to describe the categorical variables, and means and standard deviations were used to describe the continuous variables.Both univariate and multivariate logistic regression analyses were adopted to assess the incidence and risk factors associated in-hospital VTE in non-oncological urological inpatients.When the p-values were under 0.05 in the univariate analyses, the related factors were chosen to be evaluated by multivariate regression analysis.We carried out χ2statistic, and Fisher’s exact test to identify the differences between proportions and means under appropriate condition.For each measure, rates and 95% confidence intervals (CIs)were computed.In order to identify risk factors, odds ratios (ORs) and their 95% CIs were computed.In the univariate analyses, the unadjusted ORs (unaORs) were computed.The adjusted ORs (aORs) were computed by multivariable logistic regression.For all statistical comparisons, a p-value of less than 0.05 was considered statistically significant.
3.Results
From January 1, 2018 to December 31, 2018, 1658 patients who came to the urological non-oncological specialist consecutively were included in our study.Among them,205 (12.4%) patients were excluded due to their surgeries for malignant tumor removal or malignant pathological outcome.Therefore,a total of 1453 patients were enrolled in our study.These cases were urinary stones (832, 57.3%),benign prostate hyperplasia (124, 8.5%), benign adrenal tumor (78, 5.4%), ureteral stricture (63, 4.3%), varicocele(57, 3.9%), renal cyst (41, 2.8%), urethral stricture (35,2.4%), stress urinary incontinence (32, 2.2%), and others(190, 13.1%).There were 1340 (92.2%) patients that underwent surgery during the index admission; 44 (3.0%) patients underwent surgery in the month prior to admission;40 (2.8%) patients underwent emergency surgery.
Table 1 shows the patients’ characteristics associated with VTE.Of all the cohort, the total incidence of VTE was 2.3%, consisting of 32 (2.2%) DVT and 4 (0.3%) PE (two patients both got DVT and PE); 12 (35.3%) proximal and 23 (67.6%) distal VTE (one patient had both proximal VTE and distal VTE); and 6 (17.6%) symptomatic VTE and 28(82.4%)asymptomatic VTE.Of the 1453 patients enrolled in the study, 923 (63.5%) were male and 530 (36.5%) were female.There was no statistically significant difference between patients with VTE and those without VTE when taking gender and BMI into consideration.There was a statistically significant difference in age, and the unadjusted logistic regression analysis revealed that compared with patients younger than 40 years old,patients with older age had a higher incidence of VTE (unaOR 3.33, 95% CI 1.87-5.92), especially patients older than 66 years old(unaOR 9.94, 95% CI 2.28-43.42).
The characteristics of medical history associated with VTE are presented in Table 2.There were statistically significant differences in some medical history facts between patients with VTE and non-VTE patients,including previous VTE, history of varicose veins in the lower extremity(although the p>0.05, we calculated the OR value and it was significant), history of surgery within 1 month, and taking anticoagulants or antiplatelet agents before admission.In addition, unadjusted logistic regression analysis showed that patients who experienced previous VTE(unaOR 17.26, 95% CI 6.77-44.02), had history of varicose veins in the lower extremities (unaOR 3.62, 95% CI 1.06-12.36),received surgery within 1 month(unaOR 4.60,95% CI 1.55-13.67), and took antiplatelet agents before admission (unaOR 24.27, 95% CI 9.16-64.31) were more susceptible to VTE.
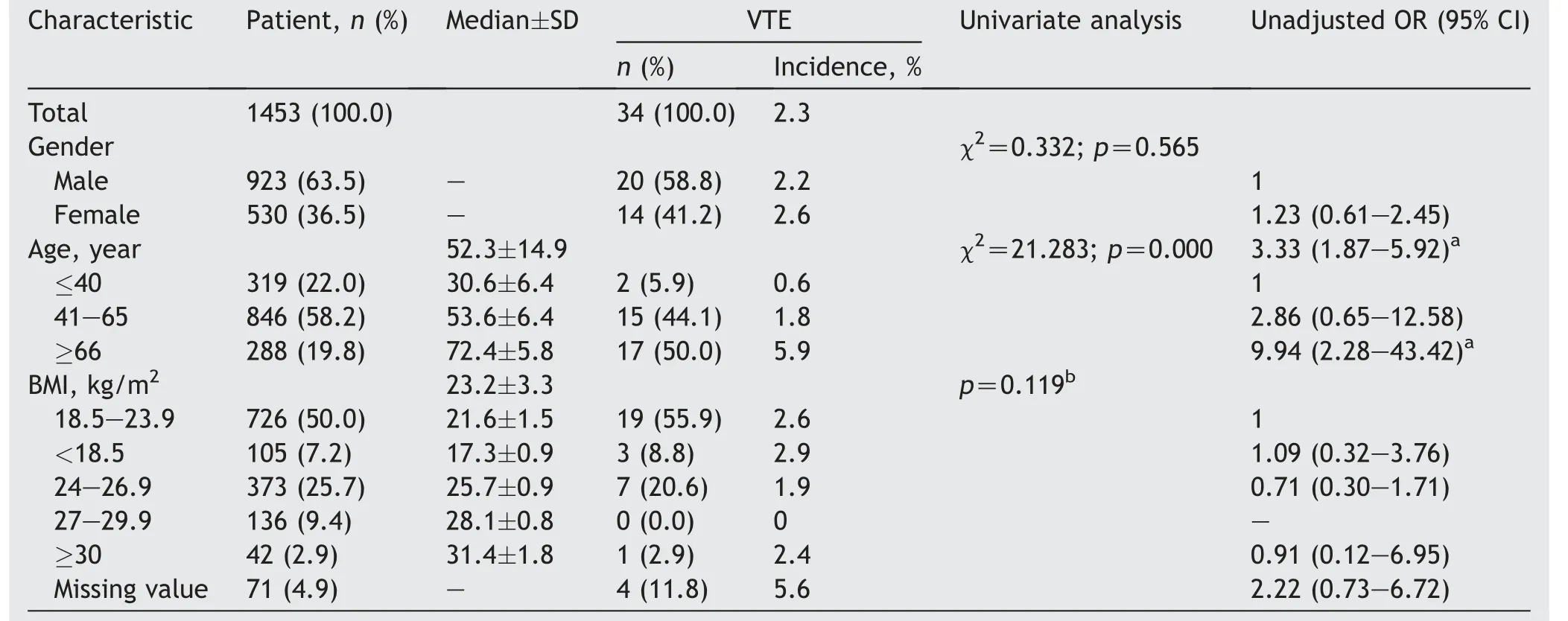
Table 1 Baseline characteristics associated with VTE.
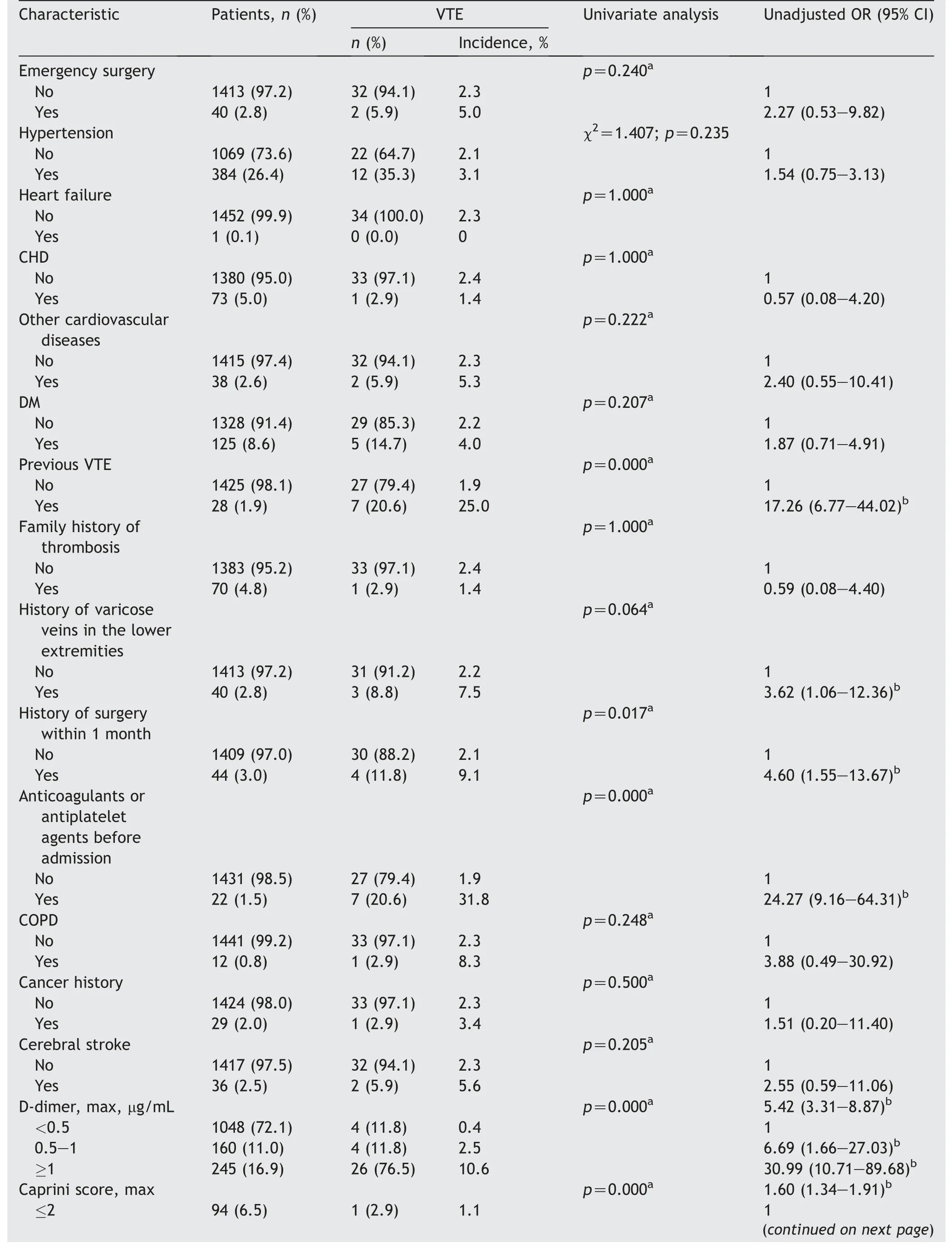
Table 2 Characteristics of medical history, D-dimer, Caprini score, and symptoms associated with VTE.
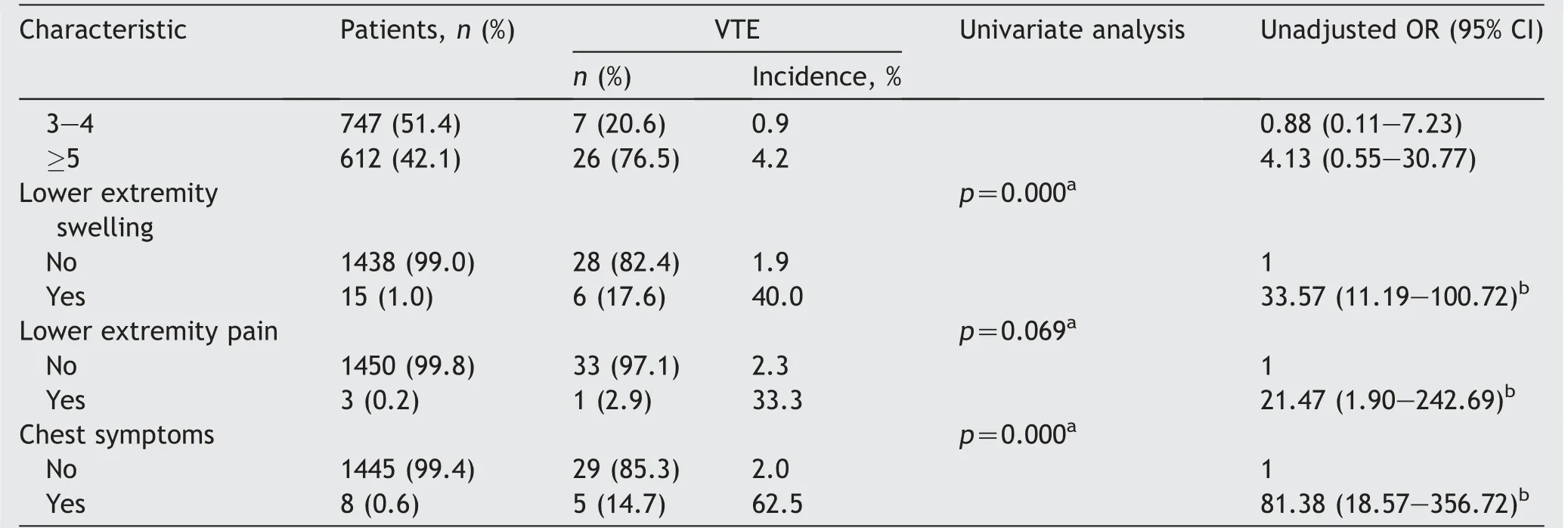
Table 2 (continued)
For D-dimer and Caprini score, they were both differed significantly between the patients with VTE and the patients without VTE (p=0.000) (Table 2).Patients with D-dimer 0.5-1 μg/mL (unaOR 6.69, 95% CI 1.66-27.03) or D-dimer ≥1 μg/mL(unaOR 30.99,95%CI 10.71-89.68)were significantly associated with a susceptibility toward VTE compared with those with D-dimer less than 0.5 μg/mL.Moreover, unadjusted logistic regression analysis suggested that patients with higher Caprini score were more likely to suffer from VTE (unaOR 1.60, 95% CI 1.34-1.91).
As for the symptom characteristics associated with VTE,the statistical differences were found in lower extremity swelling (p=0.000), and chest symptoms (including chest pain, shortness of breath, difficulty breathing, or tachycardia) (p=0.000) (Table 2).In addition, unadjusted logistic regression analysis revealed that the following factors were the potential risk factors for VTE:patients with lower extremity swelling (unaOR 33.57, 95% CI 11.19-100.72),lower extremity pain (unaOR 21.47, 95% CI 1.90-242.69),and chest symptoms (unaOR 81.38, 95% CI 18.57-356.72).
Further examination was carried out to assess the surgery-related risk factors associated with VTE.Preoperative bleeding (p=0.003), preoperative sepsis(p=0.015), higher ASA score (p=0.000), longer operation time(p=0.000),and complications including bleeding and infection (p=0.000) were perceived as risk factors of VTE according to univariate analysis (Table 3).Patients with preoperative bleeding (unaOR 8.47, 95% CI 2.75-26.08),preoperative sepsis (unaOR 6.77, 95% CI 1.91-23.98),complications (unaOR 10.07, 95% CI 4.46-22.70) were significantly associated with VTE compared with those who did not catch the symptoms mentioned above.Besides,patients with ASA score of 3 (unaOR 2.93, 95% CI 1.16-7.39) and ASA score of 4 (unaOR 6.05, 95% CI 1.22-30.16)were more susceptible to VTE compared with patients with ASA score of 1-2.When compared with patients whose duration time <60 min, patients with operation time of 60-179 min (unaOR 3.05, 95% CI 1.02-9.19) were easier to get VTE.
Multivariate logistic regression analysis was performed by including statistically significant variables in the univariate analysis to estimate the potential associations between clinical factors and VTE (Table 4).Patients who experienced previous VTE (aOR 17.056, 95% CI 3.902-74.558),taking anticoagulants or antiplatelet agents before admission (aOR 8.137, 95% CI 1.821-36.363),D-dimer (max) of more than or equal to 1 μg/mL (aOR 17.578, 95% CI 4.627-66.775), lower extremity swelling(aOR 9.188, 95% CI 1.620-52.112), chest symptoms (aOR 72.939,95%CI 6.146-865.597),and operation time of more than or equal to 180 min (aOR 17.466, 95% CI 1.952-156.253) had a positive association with a susceptibility towards VTE.
In order to further study the independence between risk factors, multivariate stepwise logistic regression analysis was carried out (Table 5).The results were similar to multivariate logistic regression analysis.However, a new risk factor, Caprini score (max) of more than or equal to 5(aOR 34.241, 95% CI 1.831-640.235), was detected by multivariate stepwise logistic regression analysis.
4.Discussion
VTE is a serious perioperative adverse event that places a heavy burden on healthcare system and may cause higher mortality with fatal PE.Identifying the incidence and risk factors of VTE is important for clinicians to apply effective strategies to prevent VTE, improve survival rates, and reduce healthcare costs.
First of all, we report the incidence and assess the risk factors of in-hospital VTE in non-oncological urological inpatients in the present population-based study.As far as we are concerned, there are few systematical large-scale researches about incidence and risk factors of urological non-cancer surgeries about VTE development, and there are few clinical trials with a sample size greater than 500 when searching the commonly used databases(PubMed,EMBASE,CNKI, Wanfang, OVID, and Springer, as of July 15, 2021).
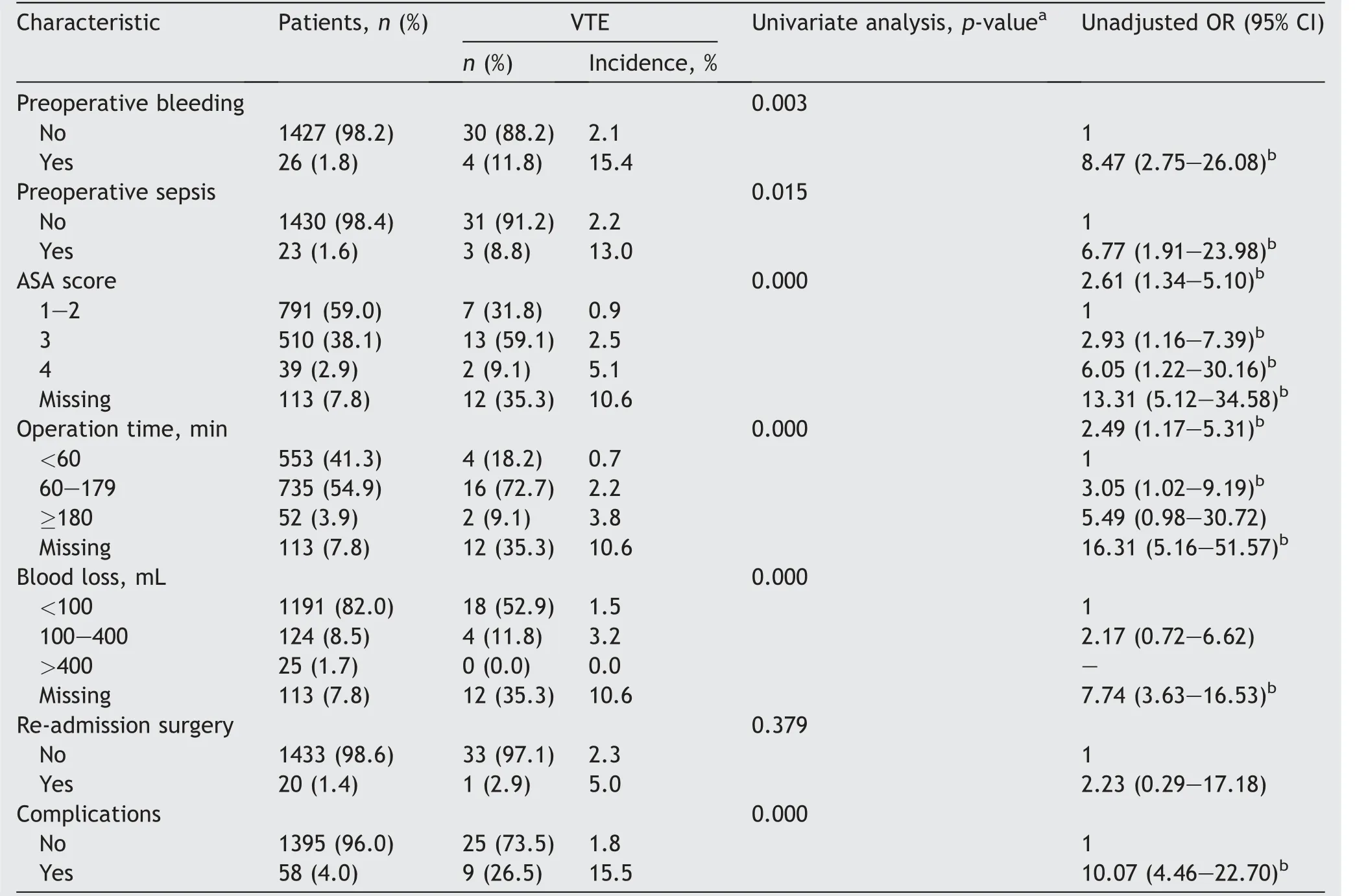
Table 3 Surgery-related characteristics associated with VTE.
Among all the patients,there was a VTE rate of 2.3%.As for other urology non-oncological surgery researches, the incidence of VTE was 1.4%for retrograde intrarenal surgery and Ho:YAG lithotripsy for renal calculi [12], 0.5% for percutaneous nephrolithotomy [13], 0.3%-7.4% for kidney transplantation [14-19], 1.9% for prolapse surgery [20],0.3%-0.7% for reconstructive pelvic surgery [21,22], and 0.5% for transurethral resection of the prostate [23] (Table 6).For the incidence in oncological urological cases, the risk of VTE in cystectomies was high (2.6%-11.6%); the incidences of prostatectomy with extended pelvic lymph node dissection were 3.9%-15.7%; and the risks of VTE following renal procedures were 0.7%-2.9% for low-risk patients and 2.6%-11.6% for high-risk patients [24].Although there is no report on the overall incidence of non-oncological surgery in urology, the results above showed that the incidence of our study was generally higher than other studies.The potential reasons are as follows:(a)the amounts of data samples studied in other literature were small,and we have conducted a more comprehensive approach to study the incidence of thrombosis; (b) urologists tend to pay more attention to the occurrence of VTE in patients with tumor surgery, while ignoring non-tumor patients in urology;(c)the way the samples we screened was different,and we had more elderly patients included in our study.
Interestingly, in our study, BMI was not a risk factor for VTE, which was consistent with the results of some urological non-cancer operations [21,25].However, BMI is clearly considered to be a risk factor stated in the European Association of Urology guidelines [10].Therefore, whether BMI is a risk factor for urinary non-tumor surgery is still a question and further prospective studies are required to clarify the fact.
We found the patients who experienced previous VTE,taking anticoagulants or antiplatelet agents before admission, D-dimer (max) of more than or equal to 1 μg/mL,lower extremity swelling, chest symptoms, operation time≥180 min,and Caprini score(max)of more than or equal to 5 were more susceptible to VTE by multivariate stepwise logistic regression analysis.In respect to current literatures, only a few studies estimated VTE risk factors in benign urological surgeries.Operation time and chest symptoms were proved to increase the risk of VTE in someurological non-oncological surgeries [21,25,26], which verified our results and the similar outcomes also happened in oncological surgeries[27,28].As for malignant urological surgeries, D-dimer level of more than or equal to 1 μg/mL was independently associated with VTE and this proved to be a good prediction for VTE [29].Some studies revealed that higher Caprini score was associated with higher rates of VTE [5,30], suggesting that Caprini score is suitable for urological surgery due to its ability to stratify patients into an appropriate risk groups [31].Pedersen et al.[32] foundthat previous VTE was an independent risk factor for VTE after Achilles tendon rupture,and similar results have been reported in other diseases [33,34].

Table 4 Clinical factors associated with VTE based on multivariate logistic regression analysis.
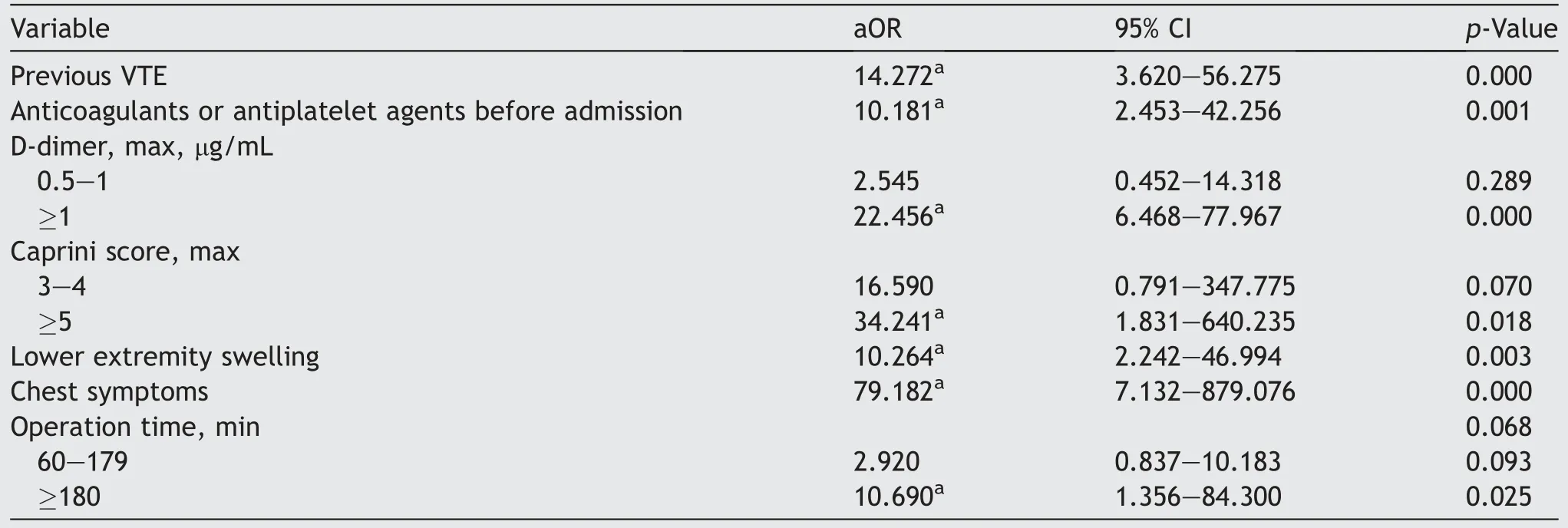
Table 5 Clinical factors associated with VTE based on multivariate stepwise logistic regression analysis.
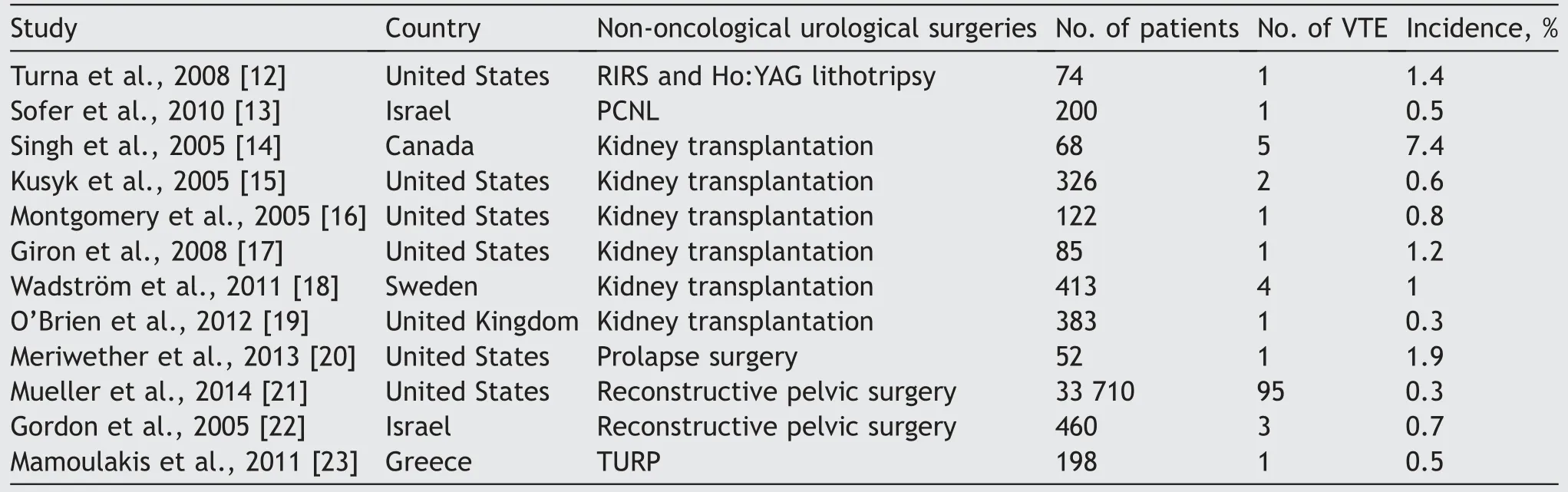
Table 6 Incidence of VTE in major non-oncological urological surgeries.
In the absence of thromboprophylaxis, the risk of thrombosis is inconsistent in various urological procedures, and different types of surgeries require different anticoagulation regimens[35].Unfortunately,there are currently no definite guidelines for urological non-oncological surgery including the European Association of Urology guidelines in urological surgery[10].In the present study,we found risk factors similar to guidelines and also some risk factors that look quite different.Thus although the current guidelines are positive progress,the call for a consensus should be taken seriously,especially for urological non-oncological surgeries.
Our research does have limitations as follows.The existing clinical screening methods are not clear so there will be some VTE patients missed, which decrease the sample of VTE patients, resulting in statistical bias.In addition, this is a single center, retrospective analysis,which may be restricted by retrospective bias.Although this limits the availability of data, its data integrity is excellent for most clinically significant variables.Therefore, we plan to design a multi-center, prospective cohort study to assess the incidence and risk factors for VTE.We also did not stratify by type of operations, including percutaneous nephrolithotomy, ureteroscope lithotripsy,retrograde intrarenal surgery, transurethral resection of the prostate, or urethroplasty.The fundamental differences in the disease processes for each of these procedures above may affect the incidence of VTE.We only stated the risk factors for VTE and did not make guidelines to predict the occurrence of VTE.Therefore, we plan to establish a predictive model for predicting VTE and screening for high-risk patients.Despite these limitations, we suppose that the data provide a comprehensive assessment of the incidence and risk factors of VTE after urological non-oncological surgeries.
5.Conclusion
In this study, we found that the incidence of VTE in non-oncological surgery was about 2.3%, which is generally higher than previous studies and the incidence of VTE in non-oncological urological inpatients has been greatly underestimated.Therefore,more researches are needed to clarify the incidence of VTE in such urologic operations.We also studied the risk factors and found that previous VTE,taking anticoagulants or antiplatelet agents before admission, D-dimer (max) of more than or equal to 1 μg/mL,lower extremity swelling, chest symptoms, operation time of more than or equal to 180 min, and Caprini score (max)of more than or equal to 5 are independent risk factors for urological non-oncological surgeries in accordance with multivariate stepwise logistic regression analysis,which can be used for early detection and diagnosis of VTE.
Author contributions
Study concept and design: Zhengyan Tang, Zhao Wang.
Data acquisition:Kaixuan Li,Quan Zhu,Haozhen Li,Ziqiang Wu, Xuesong Liu.
Data analysis: Zhao Wang, Kaixuan Li.
Drafting of manuscript: Zhao Wang, Kaixuan Li.
Critical revision of the manuscript: Zhengyan Tang.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
The authors thank the 12th ward in Xiangya Hospital,Changsha,China,for providing a platform for this research,all nurses in 12th ward for their help and cooperation in data collection, and Prof.Jiabi Qin for his statistical guidance.
 Asian Journal of Urology2023年4期
Asian Journal of Urology2023年4期
- Asian Journal of Urology的其它文章
- Arterioureteral fistula: An unusual cause of haematuria 10 years after the implantation of a synthetic iliac-femoral stent
- Utility of three-dimensional virtual reconstruction for robotic-assisted partial nephrectomy using the IRIS™
- Robotic surgery in urology: Recent advances
- Right versus left fully robotic live donor nephrectomy and open kidney transplantation: Does the laterality of the donor kidney really matter?
- Contemporary outcomes of patients undergoing robotic-assisted radical cystectomy:A comparative analysis between intracorporeal ileal conduit and neobladder urinary diversions
- Unilateral post-chemotherapy robot-assisted retroperitoneal lymph node dissection in Stage II non-seminomatous germ cell tumor:A tertiary care experience
