Implementation and achievements of enhanced recovery after surgery program in perioperative management of gastric cancer patients†
Ya-Min Yan,Yan Hu,Jing-Jing Lu,Jia-Wen Yuan,Xiao-Hong Ni,Li-Rong Shi,Zheng-Hong Yu
Nursing Department, Zhongshan Hospital, Fudan University, Shanghai 200032, China
Abstract: Objective:The enhanced recovery after surgery (ERAS) program is less implemented in gastric cancer patients.The purpose of this survey is to investigate the implementation status of ERAS in perioperative period in gastric cancer.Methods:This clinical observational study enrolled 329 patients between January 2020 and August 2020 in a single gastric cancer center.The questionnaire consisted of 4 parts: basic information,preoperative status,intraoperative status,and postoperative status of ERAS implementation in gastric cancer surgery.Results:In the preoperative period,patients’ education and counseling (100%) were well adopted.Smoking cessation (34.6%),drinking cessation (36.9%),avoidance of preoperative mechanical bowel preparation (24.3%),respiratory function training(11.2%),and administration of carbohydrate-rich drink before surgery (0.6%) were relatively not well adopted.During the operation,maintenance of intraoperative normothermia and fluid management (100%),as well as epidural analgesia (81.5%),were well adopted.Thromboprophylaxis was performed in 133 (40.4%) patients.In the postoperative period,early active mobilization was implemented about 9.5 h,and early ambulation was implemented about 39.5 h,after surgery.A total of 140 (42.5%) patients received prolonged prophylactic antibiotics;268 (81.5%) patients were provided diet upon gas passage;and 320 (97.3%) patients received intravenous fluid administration more than 5 d after surgery.The practice rate of early removal of urinary catheter (0%) and nasogastric tube(15.5%) was relatively low.A total of 11 (3.3%) patients experienced postoperative complication,and 1 (0.3%) patient received unplanned reoperation.The average costs were ¥59,500,and the average hospital stay was 12 (5,36) d.Conclusions:Standard perioperative management of ERAS program in gastric cancer surgery in China still requires improvement.
Keywords: achievement • enhanced recovery after surgery • gastric cancer • program management • surgery
1.Introduction
Gastric cancer remains an important global health problem since it is the second leading cause of cancer-related death,responsible for almost 800,000 deaths every year.1Although the treatment combination of minimally invasive surgery and chemotherapy can improve the survival of patients,gastric cancer surgery is still associated with a high risk of mortality,up to 4%.2The enhanced recovery after surgery (ERAS)program,also known as fast-track surgery,was first proposed by Prof.Henrik Kehlet in 1997.3It attempts to maintain physiological function,reduce postoperative complications,shorten the duration of hospitalization,and promote rapid postoperative recovery.4,5The ERAS program encompasses more than 20 issues associated with the entire process of perioperative management,including preoperative education and counseling,fasting,perioperative fluid management,anesthesia and analgesia,operation management,nutrition,early ambulation,drainage tube management,and hospital discharge.6,7With the development of technique in the past decades,ERAS has been applied to different fields of surgeries because of its significant benefits and safety.8
More recently,several reports demonstrated the benefits of ERAS in gastric cancer surgery.9–11However,its implementation in clinical practice is limited,and some elements are still not issued.There still remained numerous controversies,limitations,and difficulties in ERAS practice after gastrectomy,mainly because of limitations in institutional experience and conventional concept,lack of strong evidence data,and low level of awareness about ERAS.6,12Currently,there are seldom reports focusing on the implementation status of the ERAS program in gastric cancer surgery in China.To standardize ERAS protocols in gastric cancer surgery,we carried a survey to investigate the current status of the ERAS program in a large gastric cancer center in China.
2.Patients and methods
This is a prospective,clinical observational study conducted between January 2020 and August 2020 in a single gastric cancer center in Shanghai,China.This surgery was intended for gastric cancer patients.The inclusion criteria were as follows: (1) age between 18 years and 80 years;(2) gastric cancer diagnosed by preoperative gastroscopic biopsy;and (3)non-emergency surgery.The exclusion criteria were as follows: (1) inability to cooperate with the ERAS protocols (e.g.,mental disorder and paraplegia);and (2)severe organ dysfunction,such as heart,brain,and liver dysfunction.Patients could also be dropped from the study after enrollment if any of the following conditions occurred: (1) only received exploratory laparotomy,laparoscopic exploration,intraperitoneal perfusion biopsy,or palliative surgery;(2) serious complications occurred and required rescue measures in the perioperative period;and (3) the patients or their family requested withdrawal from this study.
The questionnaire of this survey consisted of 4 parts:basic information,preoperative status of ERAS implementation,intraoperative status of ERAS implementation,and postoperative status of ERAS implementation in the patients undergoing gastric cancer surgery.The data collected from the respondents,for each patient,included but were not limited to gender,age,body weight,body height,disease history,American Society of Anesthesiologists (ASA) grade,type of gastrectomy,operation time,intraoperative blood loss,multivisceral resection,and whether or not a blood transfusion had been performed.The ERAS program included 33 items in this study.The sample size was calculated as 10 times of the number of items investigated.Considering invalid samples,a total of 350 patients were investigated and received,and 329 questionnaires were valid,with an effective rate of 94.0%.
The primary endpoint was the duration of hospital stay,measured from the day of admission to discharge.Before discharge,the date associated with ERAS outcomes,such as hospital stay,costs,complications,and passage of flatus,was collected.All the enrolled patients or their families signed the informed consent,which is maintained as medical history.Patients’ basic information was anonymized during data analysis.The procedures mentioned in this study were performed in accordance with the standards of the Ethics Committee on Human Experimentation of Zhongshan Hospital,Fudan University (No.B2020-271R).
3.Results
Patients’ characteristics are summarized in Table 1.The mean age of the patients is 63.8 ± 10.6 years.Most patients still suffer from complications,such as hypertension (38.6%),diabetes mellitus (10.3%),and heart disease (6.7%).A total of 139 (42.2%) respondents had experienced previous surgeries,and 13 (4.0%) patients had family history of gastric cancer.Out of the respondents,5 (1.5%) patients received radiotherapy and 22(6.7%) patients received chemotherapy.Further,133(40.4%) patients smoked and 103 (31.3%) drank.

Table 1.Characteristics of the gastric cancer patients.
The implementation of the ERAS programs in the preoperative period is summarized in Table 2.All the patients (100%) received preoperative education and counseling in conformity with the ERAS protocols.A total of 46 (34.6%) patients implemented smoking cessation 8 weeks before surgery,and 38 (36.9%)patients implemented drinking cessation 4 weeks before surgery.Only 80 (24.3%) patients avoided preoperative mechanical bowel preparation.Most patients (61.4%)fasted for 12–24 h before surgery,while only 2 (0.6%)patients received administration of carbohydrate-rich drink before surgery.A total of 124 (37.7%) patients received nutritional support before surgery;additionally,133 (40.4%) patients received thromboprophylaxis before surgery,including the wearing of compression stocking (35.0%) and subcutaneous injected low-molecular-weight heparin (5.4%),and 37 (11.2%) patients received respiratory function training before surgery.
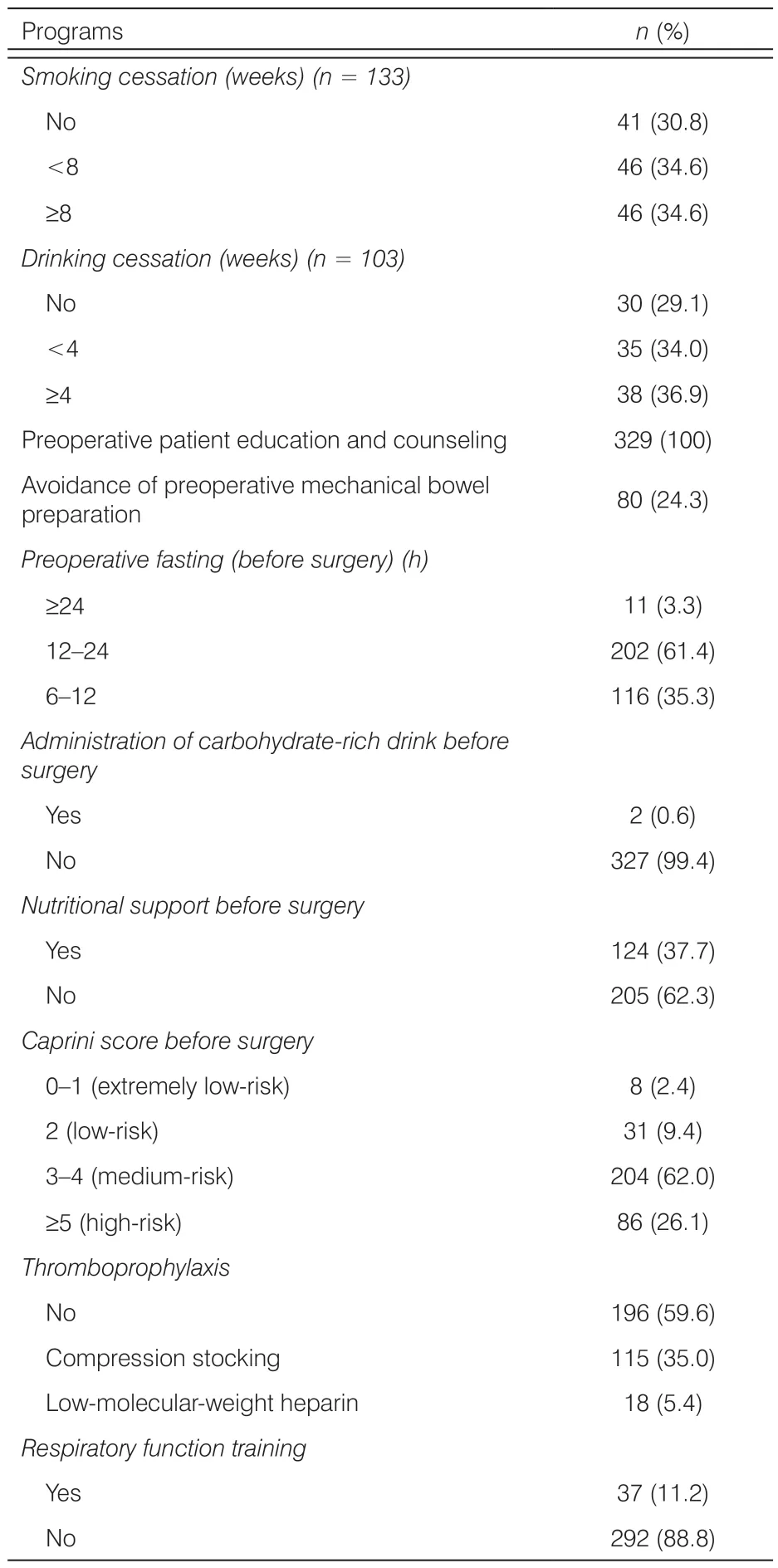
Table 2.Implementation of ERAS programs during preoperative period.
The implementation of the ERAS programs in the intraoperative period is summarized in Table 3.During the operation,100% patients ensured maintenance of intraoperative normothermia and fluid management.A total of 38 (11.6%) patients received prophylactic antibiotics.All the patients (100%) used nasogastric tube,abdominal drainage tube,and urinary drainage tube.For pain control,epidural analgesia was the most common method (81.5%),while intravenous analgesia was performed only in 61 (18.5%) patients.Thromboprophylaxis was performed in 133 (40.4%) patients.
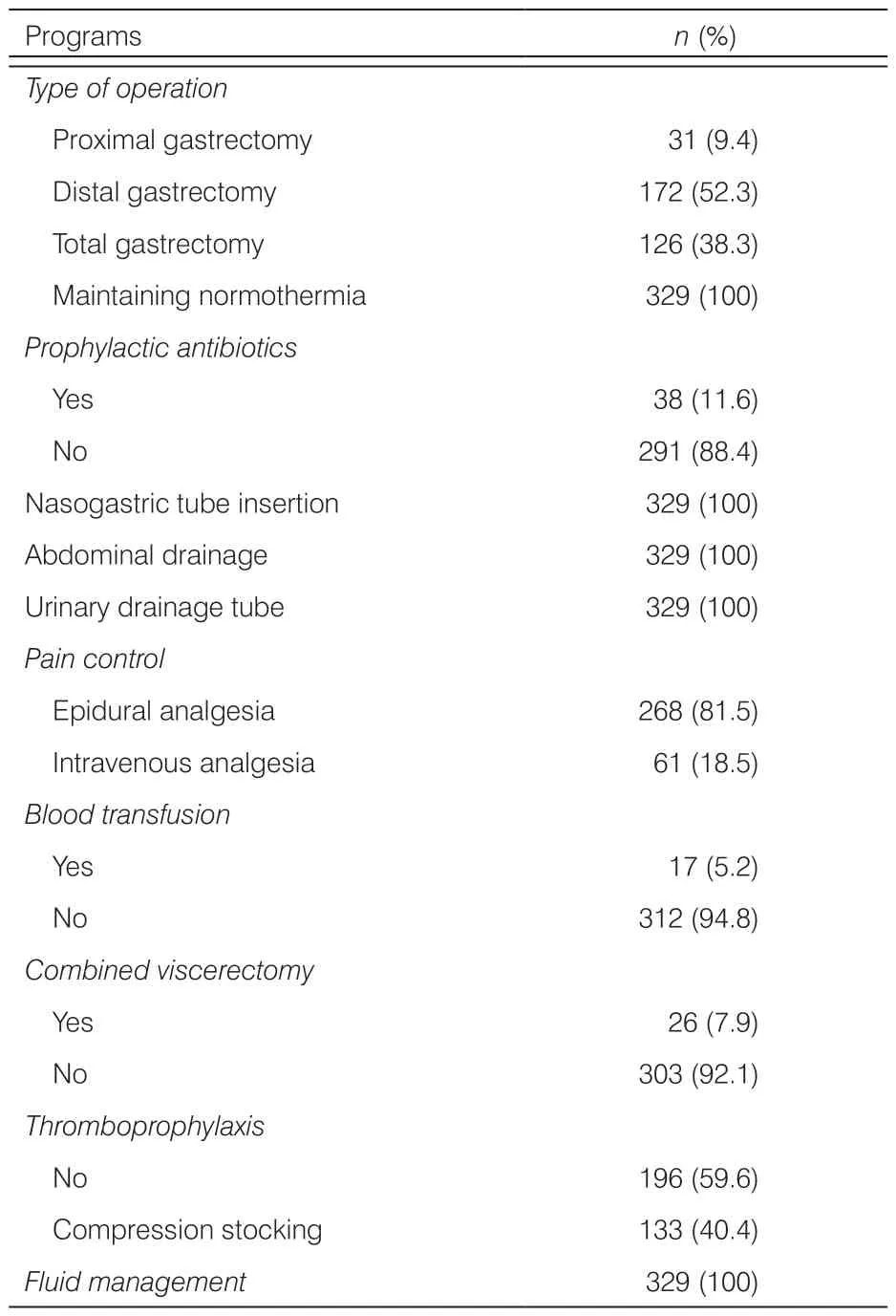
Table 3.Implementation of ERAS programs during operation (N=329).
The implementation of the ERAS programs in the postoperative period is summarized in Table 4.A total of 140 (42.5%) patients received prolonged prophylactic antibiotics after surgery;268 (81.5%) patients were provided diet upon gas passage;and 320 (97.3%) patients received intravenous fluid administration more than 5 d after surgery.Early active mobilization on the bed was implemented about 9.5 h after surgery,and early ambulation was implemented about 39.5 h after surgery.The practice rates of removal of urinary catheter (0%) and nasogastric tube (15.5%) in day 1 postoperatively were relatively low.
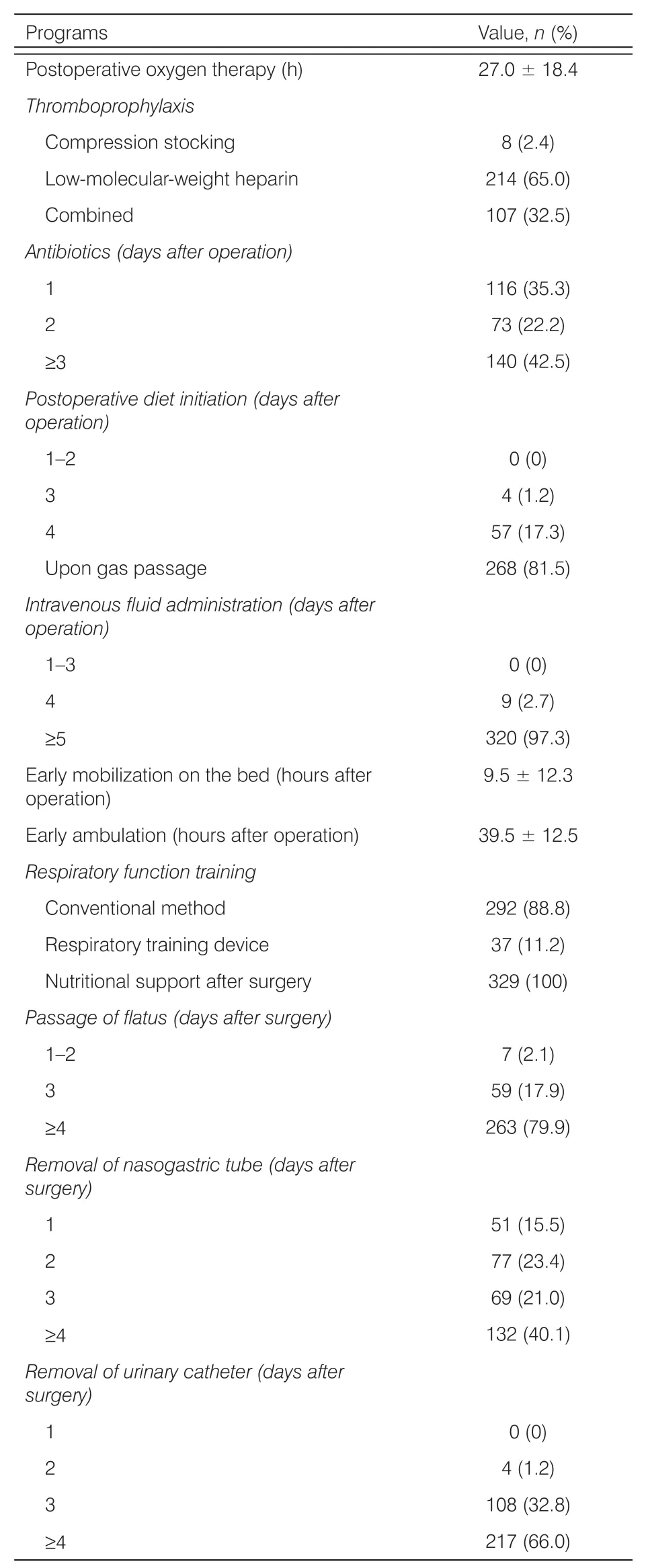
Table 4.Implementation of ERAS protocols during postoperative period (N=329).
The postoperative outcomes are summarized in Table 5.A total of 11 (3.3%) patients experienced postoperative complication,including gastroplegia(n=8),pulmonary complication (n=1),anastomotic leakage (n=1),and bleeding (n=1),and 1 (0.3%)patient received an unplanned reoperation.The average cost was ¥59,500,and average hospital stay was 12 (5,36) d.
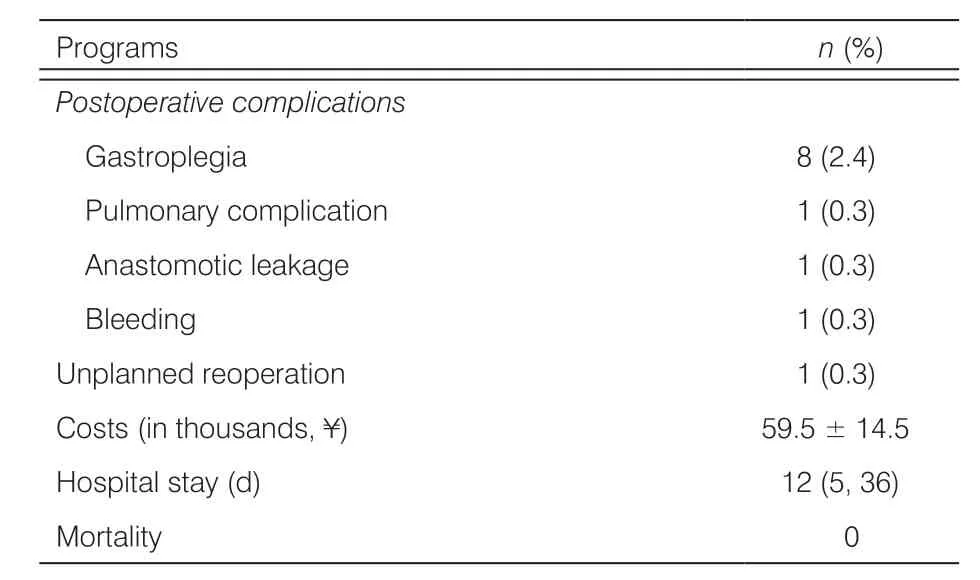
Table 5.Postoperative outcomes.
4.Discussion
ERAS programs have been gradually accepted as a proper measure to optimize clinical outcomes,thereby improving hospital experience for patients with gastric cancer.13–15The main mechanism of ERAS is through implementation of multimodal interventions,thus leading to reduction of surgery injury.There is mounting evidence to indicate that ERAS played an important role in alleviating the surgical stress response and improving the return to baseline in colorectal cancer surgery,which was afforded powerful proof in gastric cancer surgery.16,17Furthermore,Wang et al.’s study12suggested that the serum albumin level in ERAS patients was significantly higher,which demonstrates that the ERAS program could improve the nutritional status of patients with gastric cancer;additionally,it further indicates that ERAS approaches reduced the concentration of C reactive protein (CRP) and Interleukin-6 (IL-6)on days 1,4,and 7 after gastrectomy for gastric cancer,which is noteworthy because these play an important role in inflammatory response after surgery.12
Although an increasing number of surgeons are coming to greatly recognize the benefit of ERAS programs,in practice,many ERAS protocols are still not well adopted.Our results showed that among the ERAS programs,preoperative patient education and counseling,maintaining normothermia and fluid management during operation,and nutritional support after surgery were relatively well adopted in perioperative care.However,other programs,such as avoidance of preoperative mechanical bowel preparation,administration of carbohydrate-rich drink before surgery,thromboprophylaxis and respiratory function training before surgery,avoidance of routine abdominal drainage,early postoperative diet,early mobilization on the bed,and early ambulation were less well adopted.Therefore,proper solutions should be considered to overcome the obstacles of ERAS implementation.
Based on the investigation,we observed that several evidence-based practices,such as avoidance of mechanical bowel preparation,avoidance of abdominal drainage,early oral nutrition,early removal of urinary catheter,and early removal of nasogastric tube,were not implemented in real practice,with an implementation rate of only 0%–24.3%.This indicated that many unnecessary traditional practices are still being adopted.The identified factors in our previous study acting as barriers to the implementation of ERAS mainly include the following: (1) influenced by clinical experience,the clinician has still maintained the previous practice,and did not remove the drainage tube as required;(2) nurses did not perform optimal management for the patient;(3)nurses lacked knowledge of the ERAS program;and (4)there was no written information outlining the required goal implementation.18
One major concern about the ERAS program is the association with postoperative complications.In this study,11 (3.3%) patients experienced postoperative complication,gastroplegia occurred in 8 patients(2.4%),and 1 patient (0.3%) received unplanned reoperation because of anastomotic leakage.According to a meta-analysis of ERAS protocols implemented in patients undergoing colorectal surgery,the complication rates were reduced by up to 50% when ERAS principles were used.19Furthermore,the studies highlighted the importance of compliance,indicating that the better the compliance with the programs,the better the outcomes related to complications,length of hospital stay,and readmission.20,21However,a meta-analysis focusing on gastric cancer patients showed that ERAS programs appeared to be associated with increased readmission rates.12Therefore,more high-quality,large-sample,multicenter Randomized Clinical Trials (RCTs) with longterm follow-up are still needed to precisely evaluate the effectiveness of ERAS programs in gastric cancer surgery.
The results indicate that more efforts are still needed to improve the generalization of ERAS,and,once convincing evidence has been obtained for its efficacy,a greater extent of educational programs should be undertaken to encourage the implementation of ERAS in real practice.In the future,the following measures can be taken to improve the implementation of ERAS programs: (1) establish ERAS working groups,including doctors,nurses,managers,nurse navigators,and others,so as to monitor and promote the implementation of ERAS programs;(2) pain management and drainage tube management;(3) nursing staff training;(4) establish activity diary and early exercise health education prescription for the patients;and (5) early observation and management of adverse reactions.
There are several limitations characterizing the present study.First,it was conducted in a single gastric cancer center,and although this center has many gastric surgeons and patients,it is still not enough to represent the real implementation condition of ERAS programs in China.Second,we did not listen to the gastric surgeons’perspective on ERAS programs in this study,and doing so can certainly facilitate us to understand the implementation condition of ERAS programs.Against this backdrop,we are able to infer the present study’s ability to demonstrate the problems of heterogeneity of surgical care in gastric cancer patients.Third,this study only investigated the implementation condition of ERAS programs.We did not pay attention to the influencing factors and the impact the programs conveyed,such as readmission,which will be investigated in our future studies.
5.Conclusions
This study showed that,since the implementation of ERAS programs is relatively low in practice in many protocols,there is large room to improve perioperative care and facilitate the implementation of ERAS programs in gastric cancer surgery in China.
Author contributions
Conception and design: Zhenghong Yu,Yamin Yan;Administrative support: Zhenghong Yu;Provision of study materials or patients: Yan Hu,Xiaohong Ni;Collection and assembly of data: Jingjing Lu,Lirong Shi,Jiawen Yuan;Data analysis: Yamin Yan,Yan Hu;Manuscript writing: All authors;Final approval of manuscript:All authors.
Availability of data and material
The datasets generated and/or analyzed during the present study are not publicly available due to ownership by the Surgery Department,Zhongshan Hospital,Fudan University,Shanghai,China,but are available from the corresponding author on reasonable request.
Ethical approval
The procedure mentioned in this prospective,clinical observational study was in accordance with the standards of the Ethics Committee for Human Experimentation of Zhongshan Hospital,Fudan University.
Conflicts of interest
All contributing authors declare no conflicts of interest.
- Frontiers of Nursing的其它文章
- Impact of work environment on job satisfaction and stress among hemodialysis staff in Klang Valley
- Physical activity levels and predictors in patients following percutaneous coronary intervention: a cross-sectional study
- Validity and reliability of the evaluation tool of TCM confidence in students with TCM learning experience
- Knowledge,attitude,and practices related to medication errors among nursing professionals: a questionnaire-based study in a tertiary care hospital
- Factors related to self-management behavior among persons with mildto-moderate chronic obstructive pulmonary disease in Wenzhou,China
- Dietary adherence and the associated factors among Indonesian patients with type 2 diabetes: what should we be concerned about?†