Ambient Temperature and Risk of Outpatient Chronic Pharyngitis Visits: A Time-series Analysis in Xinxiang, China*
LIANG Wen Juan, CHAO Ling, ZHAO Xiang Mei, ZHANG Rong Guang,ZHAO Rui Qing, WU Wei Dong, and SONG Jie,#
Chronic pharyngitis (CP) is a prevalent medical condition in the field of otorhinolaryngology characterized by persistent inflammation of the pharyngeal mucosa, submucosa, and lymphoid tissue.The etiology of CP is multifactorial, with noninfectious factors such as personal habits (e.g.,smoking and drinking), allergic factors, voice overuse, and gastric reflux, as well as infectious agents such as bacteria and viruses playing a significant role[1].The clinical presentation of CP varies among individuals but commonly includes various uncomfortable symptoms, such as recurrent hoarseness, irritating cough, and sore throat.Despite not being lethal, CP is a stubborn, recurrent, and difficult-to-cure disease that seriously affects the patients’ quality of life.
Atmospheric temperature is an important meteorological factor that plays a critical role in human health.In recent years, a substantial body of literature has emerged, linking ambient temperature to an elevated risk of upper respiratory diseases,including bronchiectasis and allergic rhinitis[2,3].Our previous study demonstrated a positive correlation between air pollutants, such as SO2and NO2, and an increase in the number of daily outpatients with CP[4].However, the effect of ambient temperature on outpatients with CP has yet to be fully understood.Therefore, this study aimed to develop a time-series model to assess the influence of ambient temperature on outpatients with CP in Xinxiang, China.In addition, we assessed the effects of ambient temperature across different subpopulations.
Daily data on outpatient visits for CP were collected from January 1, 2015 to December 31,2018, at four hospitals in Xinxiang: Xinxiang Central Hospital, Third Affiliated Hospital of Xinxiang Medical University, Xinxiang First People’s Hospital, and Xinxiang Second People’s Hospital.These hospitals are geographically distributed across the four administrative areas of Xinxiang, providing comprehensive coverage of the local population.Hence, the data collected on CP were deemed representative.The diagnosis of CP was made by physicians at these hospitals and was encoded as J31.2 in the electronic medical records, in accordance with theInternational Classification of Diseases, tenth revision (ICD-10).During the aforementioned timeframe, the China Meteorological Data Sharing Service System (http://data.cma.cn/) was used to obtain the daily mean temperature and relative humidity readings for Xinxiang, and the daily levels of air pollutants (SO2and NO2) were gathered from four predetermined monitoring stations situated throughout the region.The geographical distribution of the four hospitals,fixed monitoring stations, and detailed data-cleaning procedures have been previously described[4].
To account for the impact of ambient temperature on health outcomes, particularly with respect to its lag and non-linear effects, a distributed lag non-linear model (DLNM) was employed to establish a cross-basis for temperature at varying lag days.This approach has been widely used to study meteorological factors affecting health outcomes[5].In addition, a generalized additive model (GAM) was employed to evaluate the association between ambient temperature and outpatients with CP.Given the low incidence rate of the disease and the overdispersion of daily outpatient values, we utilized a quasi-Poisson regression.The present study’s model accounts for the influence of long-term trends, the day of the week, and humidity.Additionally, a study by Zhao established a clear association between air pollutants, specifically SO2and NO2, and an increased outpatient risk of CP[4].The current study incorporated these pollutants into the model to control for potential confounding effects.The fundamental formula for the model is as follows:
Log[E(Yt)] =α+cb(temperature, 5, lag, 3) +ns(humidity, 3) +ns(time, 7/year) +ns(SO2, 3) +ns(NO2, 3) + DOW + holiday
Ytsignifies the total number of CP outpatient visits from the four hospitals at daytand E(Yt) signifies the estimated CP outpatient visits at dayt, andαmeans the intercept.cb represents the cross-basis function for daily ambient temperature and the degree as 5;the degrees of freedom (df) for lag space is 3; ns indicates a natural cubic spline for non-linear variables: humidity and air pollution (SO2, NO2) with the df is 3; 7 df/year was used to control for longterm trends and seasonality.Furthermore, DOW refers to the day of the week, and holiday refers to a public holiday.After establishing the final model, the relative risks and 95% confidence intervals (CIs) were calculated using the P50temperature as the reference.Additionally, we defined temperatures below the 1stpercentile as cold, above the 99th percentile as heat, and the 25thand 75thpercentiles as moderate cold and moderate heat, respectively.Previous studies used a maximum lag of 21 days to simultaneously estimate the non-linear and delayed effects of ambient temperature on respiratory diseases[5].We also selected a maximum lag of 21 days to explore the acute and long-term effects of ambient temperature on CP.Then, the immediate and cumulative lag relative risks (RR) and 95%confidence intervals (CI) of 0–7 days, 0–14 days, and 0–21 days for CP were calculated.Finally, stratified analysis by sex (male, female) and age (< 15, 15–65,and ≥ 65 years) was also performed in our study.In addition, we conducted sensitivity analyses: (1) we selected longer lag times of up to 28 days to evaluate the stability of our model, and (2) for the smoothness of time trends, we chose alternative df values from six to ten per year.All statistical analyses were performed using the R statistical project(‘mgcv’ package for GAMs and ‘dlnm’ package for DLNMs).A two-sidedP-value < 0.05 was considered statistically significant.
A total of 62,823 CP hospital outpatient records were collected from January 1, 2015, to December 31, 2018.The statistical descriptions of the daily CP outpatient visits are presented in Supplementary Table S1 (available in www.besjournal.com).The average number of daily CP outpatient visits was 43(21 males and 22 females).The outpatients were categorized into those aged < 15 (young), 15–64, and≥ 65 (old) years old, with 15, 32, and 4 cases per day,respectively.Supplementary Table S1 presents the meteorological factors and air pollutants (NO2and SO2) in Xinxiang during the study period.The daily average temperature and relative humidity were 16 °C and 60%, respectively.The percentiles of temperature, specifically the 1st, 25th, 75th, and 99thpercentiles, are denoted as P1, P25, P75, and P99,respectively.These percentiles correspond to temperature values of -2, 7, 25, and 32 °C.The annual average concentrations of NO2and SO2were 48 µg/m3and 33 µg/m3, respectively.
Table 1 shows the relative risks of CP visits corresponding to ambient temperature at different lag times (0, 0–7, 0–14, 0–21, and 0–28 days).Figure 1 presents the exposure-response curves between the temperature andRRof CP visits with different lag times.There was a significant statistical effect of moderate cold (25thpercentile, 7 °C) and heat (99thpercentile, 32 °C) on outpatient visits for CP with a lag of 0–7 days.In contrast to the median temperature (17 °C), the moderate cold (7 °C)increased the risk of CP visits (RR: 1.17, 95%CI:1.01–1.34).These results are consistent with those of previous studies.Makinen reported that cold temperatures were associated with increased pharyngitis in Finland[6].Another study conducted in Shanghai showed that low temperatures increased the incidence of acute pharyngitis[7].Short-term exposure to low temperatures has also been linked to increased respiratory diseases such as allergic rhinitis and chronic bronchitis[2,3].However, the mechanisms underlying the influence of low temperatures on chronic pharyngitis remain unclear.One possible reason is that low temperatures are more suitable for bacterial and viral infections.In addition, viral cultivation studies have confirmed that respiratory viruses replicate better at cooler temperatures.
In addition, we also found that the heat (32 °C)had a reduced risk (RR: 0.79, 95%CI: 0.65–0.97)compared to the median temperature (17 °C).However, evidence linking ambient temperature to chronic pharyngitis is scarce, and we compared our findings with those for other respiratory diseases.In studies conducted in Lanzhou, extreme heat has been associated with an increased risk of pneumonia and COPD[5].However, another study conducted in Shanghai found no positive association between hospital visits for chronic bronchitis and heat[2].It was difficult to elaborate on the exact reason for this heterogeneity.The most likely reasons for this may be the disease type and age-group composition ratio.Naina et al.reported that the mean age of patients with CP was 34.8 years (range, 18–65 years)[8]; however, it is plausible that older people have a high prevalence of lower respiratory diseases,such as COPD and pneumonia, and are thus more susceptible to extreme temperatures[5].In addition,the average annual temperature, relative humidity,and socioeconomic status in Xinxiang, which is in the hinterlands of China, were significantly different from those in Shanghai and South India.Further studies are required to investigate the underlying mechanisms.
Figure 2 shows the exposure-response curves stratified by age and sex in a lag of 0–7 days.Females were sensitive to heat; that is, our results demonstrated that females were more protected from heat-associated visits than males.Given that few studies have investigated this relationship, we compared our findings with those of other respiratory diseases.However, these results are inconsistent with our findings.One study in Beijing observed that heat waves introduced an additional risk to respiratory emergency department visits in females (RR= 1.166, 95%CI: 1.007–1.349)[9].Chai et al.also found that females with respiratory diseases were more susceptible to extreme temperatures than males[5].Diverse climatic conditions may affect the relationship between temperature and disease.Furthermore, we speculate that geographical conditions may contribute to this variance.In addition, the 15–64 age group had a significant statistical differenceaccording to heat temperature compared to the < 15 and ≥ 65 age groups.Few studies have examined the influence of temperature on CP visit effects based on age group.Thus, we compared our findings with those of other respiratory diseases.However, the study results have been inconsistent.Chai et al.showed that high temperatures displayed significant acute and short-term harmful effects on respiratory diseases in patients aged 15–59 years in Lanzhou[5].Anderson et al.reported a positive effect of heat on respiratory hospitalization in older individuals in the US[10].Further research is required to explore these potential differences.
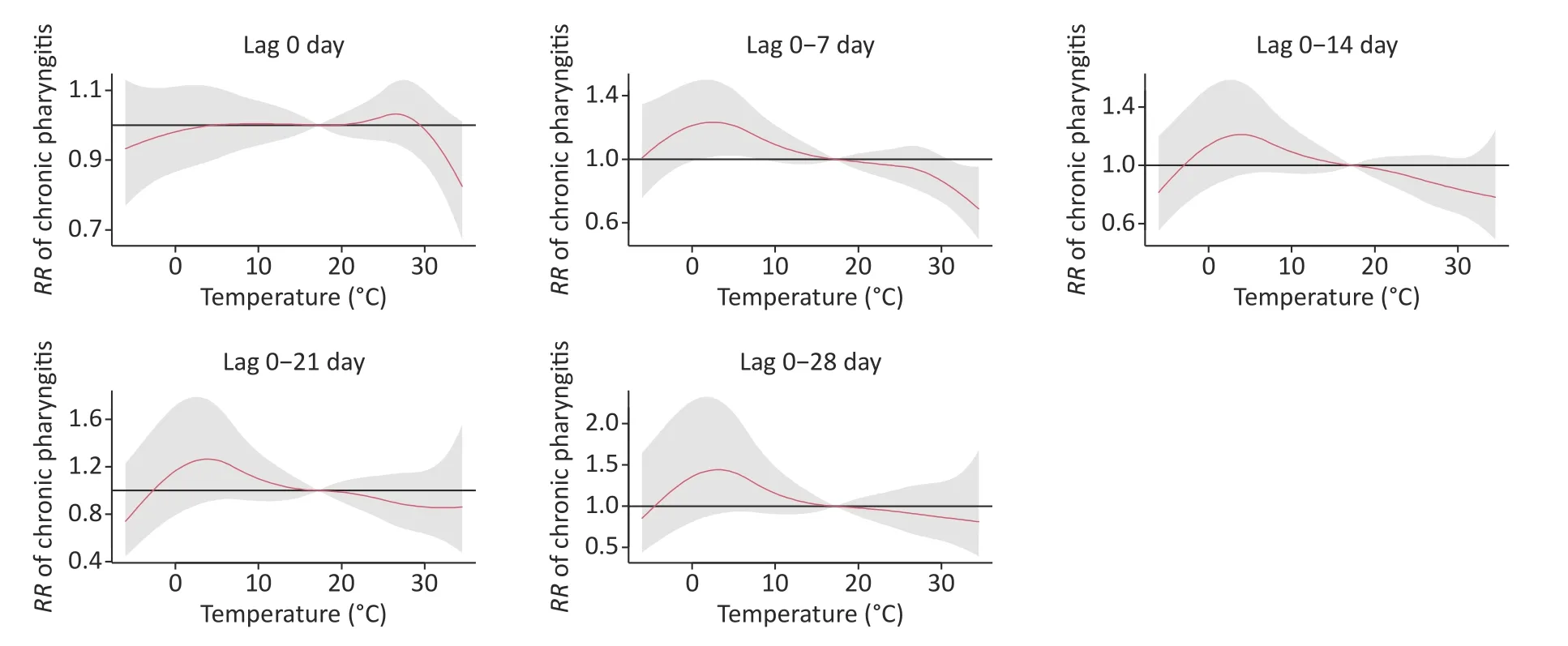
Figure 1.The exposure–response curves between the temperature and the RR of CP visits with different lag 0–28 (reference temperature at 17 °C).
For the sensitivity analysis, we constructed a model with longer lag times of up to 28 days and examined the effects of various dfs ranging from 6 to 10 each year on the smoothness of seasonality.The results were not substantially changed (data not shown), indicating the robustness of the model.
Our study has several limitations.First, we obtained the records of CP outpatients from four hospitals in Xinxiang; therefore, the CP diagnosis criteria might have been slightly different, and there might have been misdiagnosed records.In addition,climatic data for the CP population exposure were obtained from only one fixed meteorological monitoring station; thus, exposure measurement errors are inevitable.Third, we did not consider etiological data at the individual level, which might have affected the temperature exposure levels and health outcomes.Fourth, the conclusions may only be representative of a single city; hence, more work involving more cities is needed to verify the effect of temperature on CP.Finally, we investigated the correlation between chronic pharyngitis and temperature using the GAM and DLMN models.Further validation of the actual impact of population exposure and animal experimentation is warranted in future research.
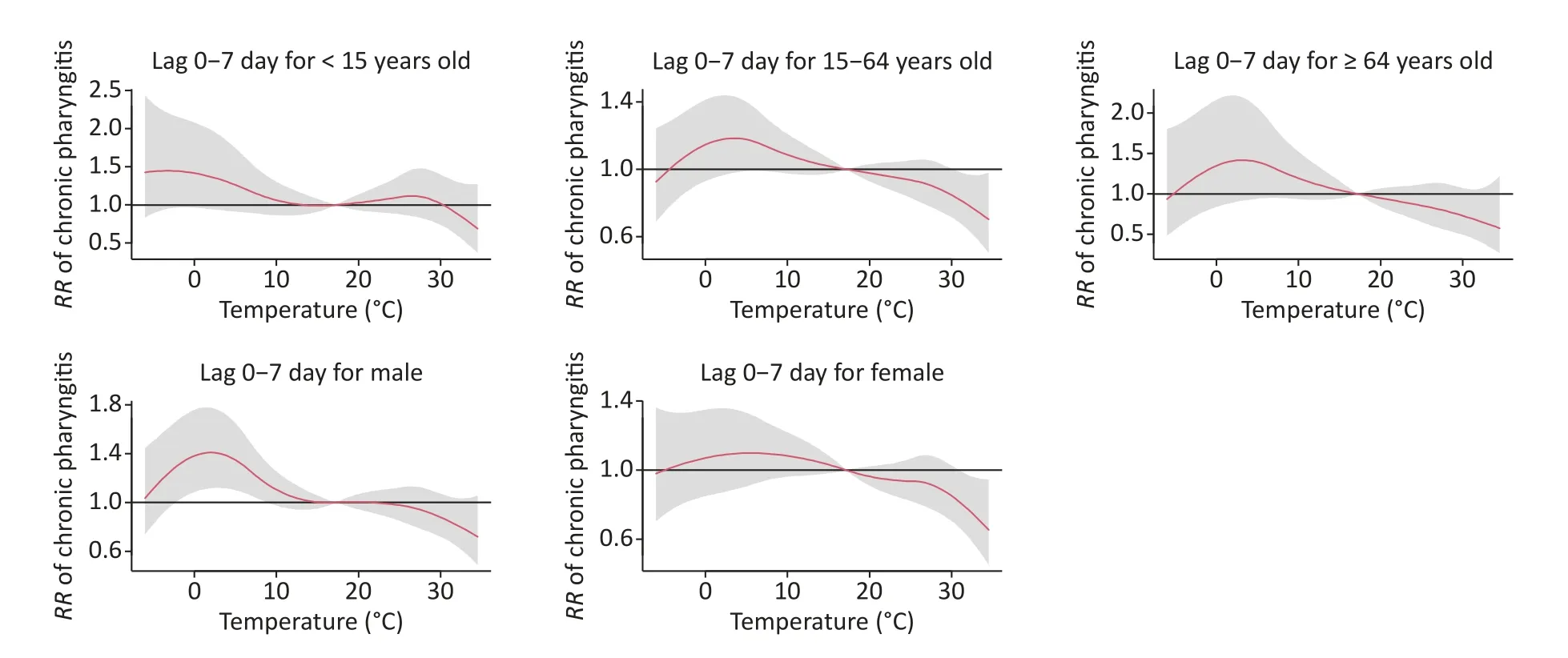
Figure 2.The exposure-response curves between daily ambient temperature and RRs of daily outpatient visits stratified by age and gender.
In summary, our analysis has demonstrated a significant correlation between moderate cold (7 °C)and an elevated risk of CP outpatient visits, while high temperatures (32 °C) are associated with a reduced risk.These findings have substantial implications for formulating efficient cold riskmanagement strategies from a public health perspective.To the best of our knowledge, this study represents one of the few investigations that have directly examined the relationship between ambient temperatures and CP outpatient visits.Consequently, our results provide novel evidence of the impact of temperature on human health.
Competing InterestsThe authors declare no conflict of interest.
ContributionsLIANG Wen Juan: Investigation,writing the original draft, and funding acquisition;CHAO Ling: Methodology and data Validation; ZHAO Xiang Mei: Methodology, software, and visualization;ZHANG Rong Guang: Writing-review; ZHAO Rui Qing:Investigation, methodology, and validation; WU Wei Dong: Writing-review; SONG Jie: Funding acquisition,supervision writing, editing, and project administration.
Ethics Approval and Consent to ParticipateThis study was an observational study.The Research Ethics Committee of the Xinxiang Medical University confirmed that no ethical approval was required.
AcknowledgmentsI would like to thank all the participants in this study.
Availability of Data and MaterialsAll data in the study can be accessed from the corresponding author (songjie231@126.com) after the application.
Consent for PublicationNot applicable
#Correspondence should be addressed to SONG Jie,Professor, E-mail: songjie231@126.com; Tel: 86-373-3831646.
Biographical note of the first author: LIANG Wen Juan, female, born in 1983, PhD, majoring in prevention and control of infectious disease.
Received: May 7, 2023;
Accepted: August 24, 2023
 Biomedical and Environmental Sciences2023年10期
Biomedical and Environmental Sciences2023年10期
- Biomedical and Environmental Sciences的其它文章
- Treatment Outcomes in COVlD-19 Patients with Brucellosis:Case Series in Heilongjiang and Systematic Review of Literature*
- Value of Pretreatment lnflammation-nutrition Score to Predict Non-response to Neoadjuvant Chemotherapy in Locally Advanced Rectal Cancer*
- A Comprehensive View on the Progress of Organoid Research with an Emphasis on its Relevance to Disease Characterization
- Altered Expression of COMP, Collagen 1, and MMP9 in Pelvic Organ Prolapse*
- Synthesis of TiO2 Nanospikes for Dual Antibacterial Activity*
- Aurora A Kinase Plays a Key Role in Mitosis Skip during Senescence lnduced by lonizing Radiation*
