Observation on Therapeutic Effect of Erxian Decoction on Relieving Low Back Pain after PVP of PMOP-derived Vertebral Fracture
Xianda ZHANG, Guoqiang LIANG, Jianxiong MO, Yujiang LIU, Xiaofeng SHEN*
1. Anhui University of Chinese Medicine, Hefei 230031, China; 2. Suzhou TCM Hospital Affiliated to Nanjing University of Chinese Medicine, Suzhou 215009, China
Abstract [Objectives] To explore the clinical effect of Erxian decoction on relieving low back pain after percutaneous vertebroplasty (PVP) of vertebral compression fracture caused by postmenopausal osteoporosis (PMOP). [Methods] Ninety patients who were treated in Suzhou TCM Hospital from September 2021 to January 2023 were randomly divided into three groups: traditional Chinese medicine group (n=30), western medicine group (n=30) and blank group (n=30). The patients in all the three groups were treated with basic anti-osteoporosis drugs. The patients in the traditional Chinese medicine group were treated with Erxian decoction after PVP, and those in the western medicine group were treated with celecoxib to relieve pain after operation. The visual analogue (VAS) score, Oswestry dysfunction index (ODI) score, TCM syndrome score and serum indexes such as interleukin-6 (IL-6) and estrogen E2 were recorded before treatment and 2 weeks, 1 month and 3 months after treatment. [Results] (i) In terms of pain relief, the VAS score of the western medicine group was lower than that of the traditional Chinese medicine group after 2 weeks of treatment, but there was no significant difference in VAS score between the two groups after 1 month and 3 months, and the pain improvement of the two groups was better than that of the blank group. (ii) After 3 months of treatment, the ODI score in the traditional Chinese medicine group was lower than that in the western medicine group, and the improvement of TCM syndrome in the traditional Chinese medicine group was better than that in the other two groups 1 and 3 months after treatment (P<0.05). (iii) The level of IL-6 in the western medicine group was lower than that in the other groups after 2 weeks, and there was no significant difference between the two groups after 3 months of treatment. After 3 months of treatment, the level of E2 in the traditional Chinese medicine group was higher than that before treatment and higher than that in the western medicine group and the blank group, but there was no significant difference between the two groups (P>0.05). [Conclusions] Both Erxian decoction and non-steroidal anti-inflammatory drugs can relieve residual low back pain after PVP, and their long-term effects are similar, but Erxian decoction has more advantages in alleviating pain, muscle and joint pain and sensory abnormalities in postmenopausal women. Moreover, it is safe and reliable, and is worthy of clinical application.
Key words Postmenopausal osteoporosis, Vertebral fracture, Erxian decoction, Pain
1 Introduction
Osteoporotic vertebral compression fracture (OVCF) is a common complication of postmenopausal osteoporosis(POMP), and percutaneous vertebroplasty (PVP) is an important method for the treatment of OVCF. It can partially restore vertebral height and correct local kyphosis while stabilizing vertebral body and relieving pain. However, some patients still have persistent pain around the injured vertebrae and lower waist after operation, which affects the prognosis and quality of life of the patients. The reason lies in the biological factors of osteoporosis and the biomechanical changes after PVP[1]. The residual low back pain in PMOP patients after PVP can be classified as "bone impotence and low back pain" in Chinese medicine according to its etiology and corresponding symptoms.SuWenmentioned that "all strains injure the kidneys and damages the hyperactivity of yin and yang… when yin and yang are out of harmony, the bone marrow is not nourished, resulting in bone atrophy, which will easily lead to fractures, and if the muscles and tendons are not moistened, they will be painful." Above, the causes of pain after PVP in PMOP patients are both deficiency and excess, mainly based on the decline of kidney, liver and spleen viscera function, imbalance of yin and yang, qi stagnation and blood stasis. As the empirical prescription of professor Zhang Bona at Shanghai University of Traditional Chinese Medicine, Erxian decoction is widely used in the treatment of various diseases caused by postmenopausal osteoporosis. In this paper, Erxian decoction was used to treat postmenopausal osteoporotic vertebral fracture patients with residual pain after PVP, receiving good curative effect. The report is as follows.
2 Clinical data and methods
2.1 Clinical data
2.1.1General information. The patients who were hospitalized in Suzhou TCM Hospital from September 2021 to January 2023 were taken as the objects of this study. All patients with postmenopausal osteoporotic vertebral compression fractures were treated with PVP operation.
2.1.2Diagnostic criteria. Diagnostic criteria of western medicine referred to OVCF diagnostic criteria inChineseGuidelinesforDiagnosisandTreatmentofOsteoporoticFractures-principlesforDiagnosisandTreatmentofOsteoporoticFractures[2]: (i) There was persistent low back pain, which can be accompanied by chest and flank pain; the pain can be relieved when lying on the back, aggravated when the posture changes, and the visual analog score (VAS) was ≥4; (ii) Physical examination showed limited movement of the chest and waist, tenderness and percussion pain in the responsible vertebrae of the fracture, and no nerve damage in the lower extremities; (iii) The responsible vertebra of pain was determined combined with imaging examination; (iv)Tvalue ≤-2.5.SD was determined by dual energy X-ray absorptiometry (DXA).
Diagnostic criteria of traditional Chinese medicine referred toTheGuidelinesforDiagnosisandTreatmentofPostmenopausalOsteoporosis(BoneImpotence)ofTraditionalChineseMedicine(2019Edition)[3]. Diagnostic criteria of kidney yin and yang deficiency type were: low back pain, sore waist and knees as the main symptoms; both dizziness and tinnitus, upset and lack of sleep, limb tiredness, initial cold and fever, nocturnal urination frequency, light tongue, thin coating, weak pulse.
2.1.3Inclusion criteria. (i) Meet the above diagnostic criteria and syndrome differentiation criteria before operation; female patients over 60 years old; (ii) One week after PVP, there was still low back pain, and the visual analogue scale (VAS) score was 2-5; (iii) No history of low back pain before fracture; (iv) Complete clinical data, volunteer to participate in the study and sign the informed consent form.
2.1.4Exclusion criteria. (i) Serious underlying diseases such as heart, brain, liver and kidney; (ii) Low back pain caused by lumbar disc herniation, lumbar spinal stenosis or low back fasciitis; (iii) Long-term use of hormones or other drugs that affect bone metabolism; (iv) Secondary to OP caused by other diseases.
2.1.5Shedding standard. (i)Those who do not meet the criteria of this study and are mistakenly included; (ii) The patient lacks compliance and is unable to complete the prescribed course of treatment in accordance with the study plan; (iii) Serious adverse events such as liver, kidney and stomach injury occurred in the course of medication.
2.1.6Grouping method and baseline data. As shown in Table 1, the patients who met the requirements were randomly divided into traditional Chinese medicine group (TCM group,n=30), western medicine group (WM group,n=30) and blank group (n=30). The demographic data and clinical characteristics of the three groups were balanced before treatment (P>0.05).
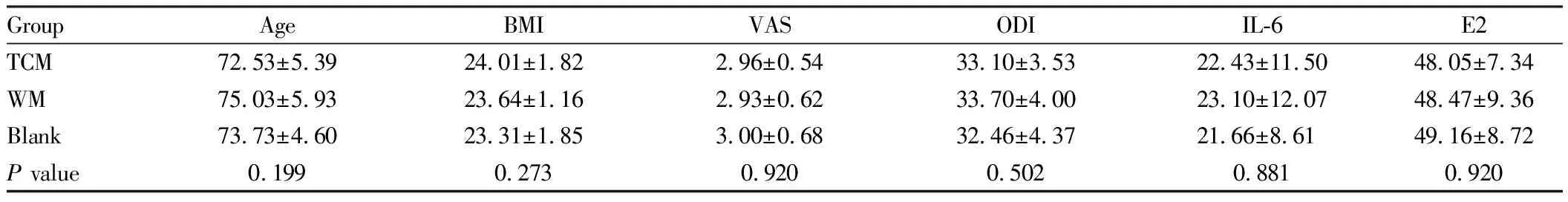
Table 1 Comparison of baseline data of patients in three groups (n=30)
2.2 Methods
2.2.1Treatment method. The patients in all the three groups were treated with PVP, and the operations were performed by the same group of doctors. On this basis, on the first day after operation, the patients in the blank group were given oral common calcium (300 mg) once a day, 2 tablets once a day plus alendronate once a day, 10 mg, while those in the traditional Chinese medicine group were given Erxian decoction on the basis of the blank group. The prescription consisted of Xianmao 15 g, Xianlingpi 15 g, Bajitian 9 g, Huangbo 9 g, Zhimu 9 g, Danggui 9 g. In the western medicine group, celecoxib capsule/200 mg was added on the basis of the blank group, one tablet a day after meals, and the patients in all the three groups were treated continuously for 3 months. The liver and kidney functions were reexamined every month during the treatment period.
2.2.2Observation index. (i)The degree of pain was compared among the three groups after 2 weeks, 1 month and 3 months of treatment. The VAS score was 0:10. The higher the score, the more severe the pain. (ii) Oswestry dysfunction index (ODI) was used to evaluate lumbar function, with a score of 0-100. The higher the score, the worse the lumbar function. (iii) The clinical efficacy of the three groups was compared at each stage of treatment (based on TCM syndrome scores shown in Table 2). (iv)The levels of interleukin IL-6 and estrogen E2 in blood were compared among the three groups during the treatment period.

3 Results and analysis
3.1 Withdrawal and shedding of patientsA total of 3 patients in the traditional Chinese medicine group asked to withdraw after 2 weeks of treatment. Six patients in the western medicine group had a burning sensation of stomach discomfort after 2 weeks of treatment, and 2 patients asked to withdraw. Two patients in the blank group failed to complete follow-up because of incomplete information.
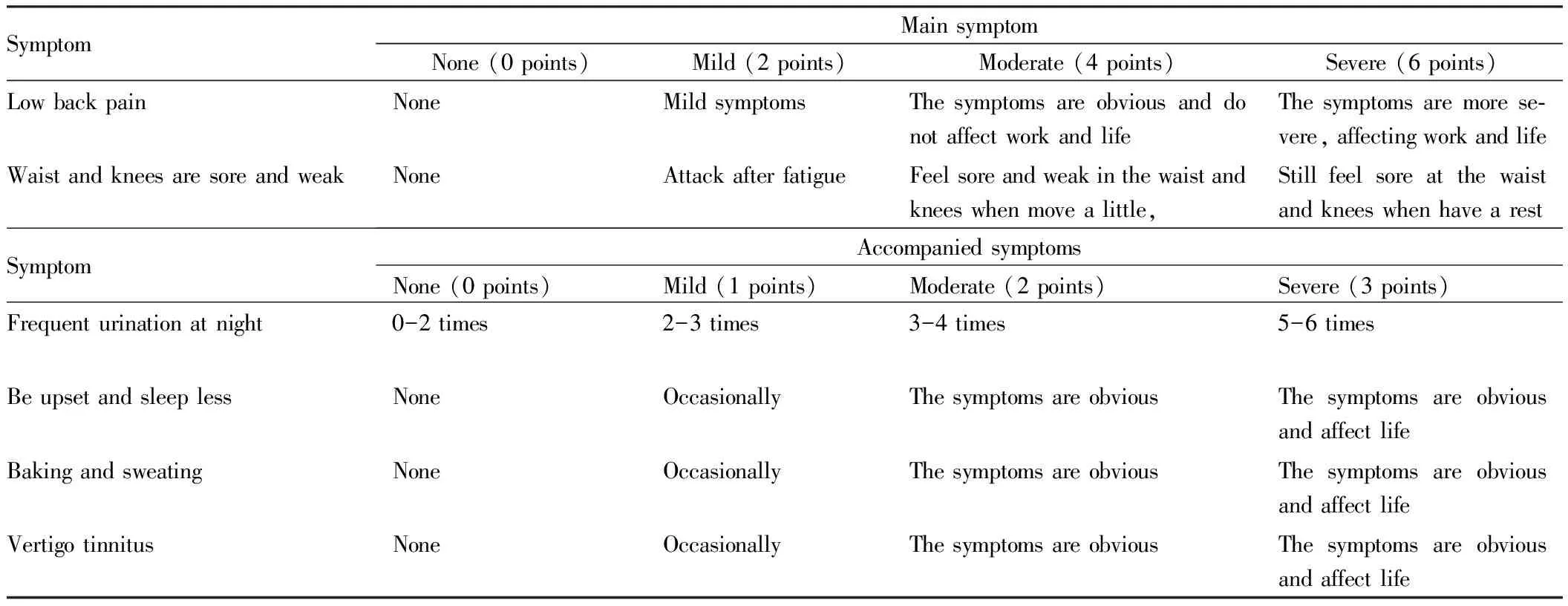
Table 2 TCM syndrome integral
3.2 Comparison of pain degree and lumbar spine function in the three groups before and after treatmentVAS scores and ODI scores between the three groups before treatment were compared (P>0.05). After 2 weeks, 1 month, and 3 months of treatment, the pain relief effect of the two groups of traditional Chinese medicine and western medicine was better than that of the blank group (P<0.05). After 2 weeks of treatment, the VAS score of the western medicine group was lower than that of the traditional Chinese medicine group (P<0.05), and there was no significant difference in curative effect between the groups. After 3 months of treatment, the Chinese medicine group had slightly better pain relief effect than the western medicine group, but the difference was not statistically significant (P>0.05). After 2 weeks and 1 month of treatment, the improvement of lumbar spine function in the medication group was better than that in the blank group (P>0.05). After 3 months of treatment, the ODI score of the Erxian decoction group was lower than that of the celecoxib group (P<0.05, Table 3).
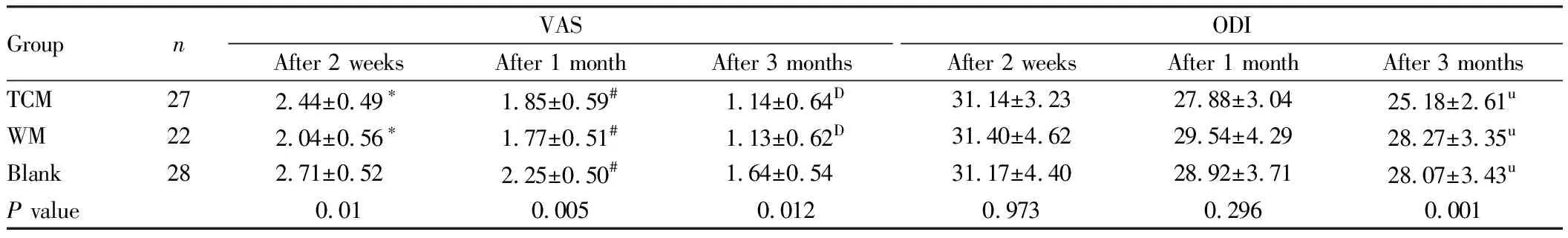
Table 3 Comparison of VAS score and ODI score among three groups at three treatment stages
3.3 Comparison of TCM syndrome scores among the three groupsTCM syndrome scores on the first day after operation were compared among the three groups (P>0.05). After 2 weeks, 1 month and 3 months of treatment, compared with celecoxib group, Erxian decoction group had more advantages in relieving waist and knee pain and other symptoms, and TCM syndrome score was lower than that in western medicine group, with statistically significant differences among groups (P<0.05, Table 4).
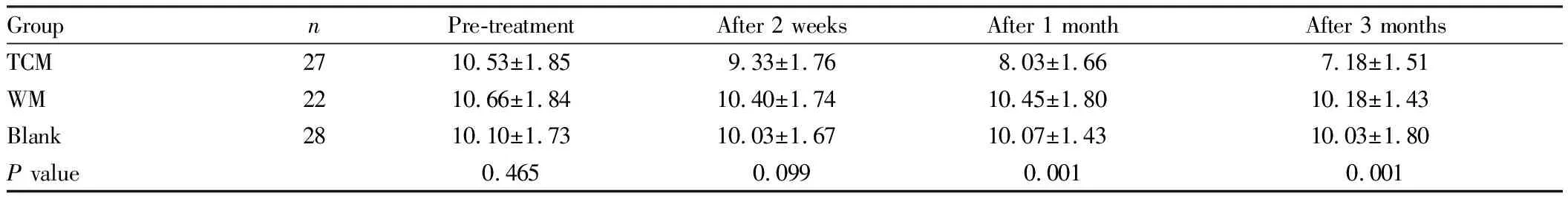
Table 4 Comparison of TCM syndrome scores in three treatment stages
3.4 The levels of IL-6 and E2 indexes were compared among the three groups after 1 month of treatmentBefore treatment, IL-6 and E2 were compared among the three groups (P>0.05). After 2 weeks of treatment, the IL-6 index in the western medicine group was lower than that in the Chinese medicine group (P<0.05). After 3 months of treatment, the level of E2 in the Chinese medicine group was higher than that in the Western medicine group, but there was no statistical significance between the groups (P>0.05, Table 5).
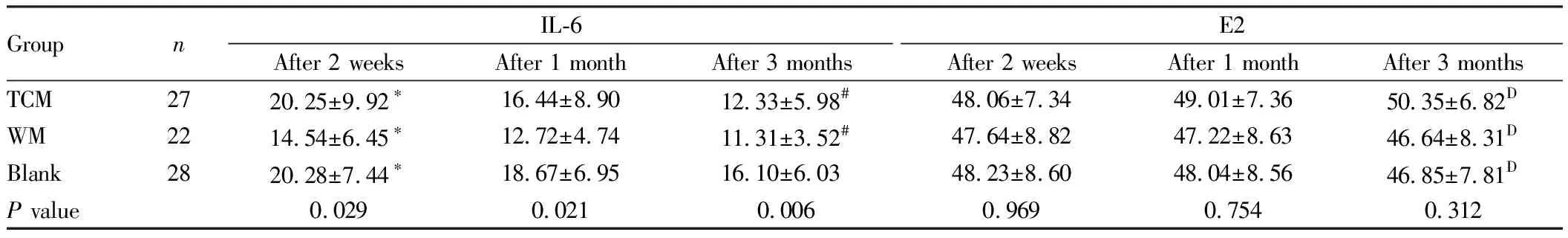
Table 5 Comparison of IL-6 and E2 values in three groups during treatment
4 Discussion
According to statistics, there are 9 million cases of brittle fractures caused by osteoporosis in the world every year, about half of which occur in the vertebral body[4], accounting for about 1/3-1/2 of the incidence of osteoporotic fractures. However, in China, the total prevalence rate of PMOP caused by the decrease of hormone level is 38.8%[5], which is a potential secondary possibility of OVCF. As an important method for the treatment of OVCF patients, PVP is widely used in clinical practice, with the characteristics of minimally invasive and definite curative effect. However, 1.8%-15.6% of patients will experience symptoms of residual low back pain after surgery[6], which will affect postoperative recovery and reconstruction of lumbar spine function. Therefore, effective intervention for postoperative residual low back pain is required.
Erxian decoction is a commonly used prescription in Suzhou TCM Hospital. In the prescription, curculigo and fairy spleen warm kidney yang and nourish kidney essence;Morindaofficinaliswarms kidney yang and strengthens muscles and bones; yin and diarrhea fire. The whole prescription is brief and precise, and its compatibility is rigorous. It plays the role of warming and nourishing the spleen and kidney, replenishing essence and nourishing blood, nourishing yin and supporting yang, and balancing yin and yang. Combined with this study, our prescription is compared with non-steroidal anti-inflammatory drugs, both of which can be applied to the treatment of chronic low back pain after PVP in PMOP patients, and the long-term efficacy is basically similar. However, statistics show that in addition to relieving chronic pain that may be secondary to PVP surgery, Erxian decoction is also effective in improving TCM syndromes such as soreness and weakness of the waist and knees, cold muscles, poor night sleep, spontaneous sweating and night sweating caused by the imbalance of yin and yang. Coincidentally, Xiangetal.[7]combined with Erxian decoction on the basis of western medicine treatment and found that it can further regulate hot flashes, night sweats, insomnia and anxiety in postmenopausal hypertensive female patients, and improve Kupperman score. It has also been reported that Erxian decoction can regulate the level of reproductive hormones, stabilize the internal environment, and relieve a series of symptoms caused by autonomic nervous dysfunction, such as skin paresthesia, head and body pain, and muscle acid[8]. It is worth noting that during the study, 6 patients in the western medicine group were shedding due to gastrointestinal symptoms such as stomach pain and pantothenic acid, while patients in the Chinese medicine group did not see significant damage to liver and kidney function during regular review, so taking Chinese medicine is more in line with the safety considerations of most patients.
Modern studies have found that the persistent pain induced by PVP in PMOP patients is the process of osteoclast-mediated bone remodeling and inflammation[9]. (i) In the short term, the inflammation caused by the initial rejection reaction of bone cement intervention, the aggravation of the inflammatory response during the fracture repair process, and the injury of the paravertebral muscles and soft tissues of the injured vertebra all lead to the further increase of inflammatory factors in the blood of PMOP patients originally at a high level[10], which are the main cause of acute pain, and oral celecoxib drugs can effectively fight against it, thereby relieving symptoms. (ii) Chronic pain beyond 1 month may be caused by the overactivity of osteoclasts in the process of bone remodeling, and acid-sensitive ion channel 1 and capsaicin receptor 1 are activated, resulting in acidification of the local microenvironment, which in turn prolongs the pain[11]. (iii) During the entire pathological process, factors such as TNF-α and IL-6 promote bone resorption, osteoblast apoptosis, and then destroy the microstructure of bone tissue and stimulate local nerve fibers, inducing neuropathic pain. The continuous reduction of estrogen level can also lead to the activation of the inflammatory response of the body tissue[12], and the interaction between the two will make the postoperative residual low back pain stubborn and difficult to subside.
Combined with the results of this study, the prescription mainly achieves the purpose of relieving postoperative chronic low back pain from two aspects: improving osteoporosis and interfering with inflammation around the waist and back. (i) Postmenopausal women often present with high-transition osteoporosis. Preliminary studies have found that Erxian decoction can improve osteoporosis through multiple targets and multiple channels. Wangetal.[13]used network pharmacology integration to discover the active ingredients in the prescription. It can promote the osteogenic differentiation of bone marrow mesenchymal stem cells by regulating bone morphogenetic protein (BMP) and Wnt/β-catenin signaling pathway in osteoblasts, participate in bone formation, and can inhibit the activity of osteoclasts and inhibit bone resorption. (ii) Kaijieetal.[14]found that Erxian decoction may act on targets such as IL-6 and TNF-α by regulating PI3K/Akt, MAPK and neuroactive ligand/receptor signaling pathways, and the formula is effective. Components such as epimedium flavonoids have been shown to have estrogen-like effects[15]and can increase E2 levels, and iridoid glycosides inMorindaofficinaliscan resist inflammatory damage[16]. Therefore, taking Erxian decoction for a long time can improve the decline of hormone levels and possible chronic inflammatory stimulation.
In summary, the prevention and treatment of residual pain after PVP by Erxian decoction is in line with the theory of "prevention after recovery" in traditional Chinese medicine. It effectively controls the progression of postmenopausal osteoporosis, relieves chronic inflammatory stimulation of paravertebral muscle tissue, and reduces the risk of secondary fracture of adjacent vertebral bodies, thus improving the quality of life of PMOP patients after PVP. However, postoperative vertebral infection and/or new vertebral fractures may occur within 3 months of surgery, so the choice of 3 months as a postoperative study period may have been too short to capture other pain-related events. Finally, the objectivity of the analysis is weak, as some of our data are qualitative assessments.
- Medicinal Plant的其它文章
- Experimental Study on Anatomic Reduction of Lateral Pterygoid Muscle (Simulated Manipulation Fracture Reduction) and Condylar Free Reduction for Condylar Fracture
- Protective Effect and Molecular Mechanism of Shui People’s Classic Prescription Jipei Dilong Ointment on Osteoarthritis in Rats
- Effects of Cigu Xiaozhi Formula on miR-378a-3p Expression and Hh Signaling Pathway in TGF-β1 Induced LX2 Cells
- Chlorophyll Fluorescence Response of Persimmon Plants under Salt Stress
- Optimization of Solid-state Fermentation Conditions of Sophora japonica cv. jinhuai by Response Surface Methodology
- Optimization of Compound Coptis Ointment Extraction through the Integration of Pharmacodynamic Indices and Orthogonal Test