脓毒症合并自发性脾破裂出血1例报告
柳舟 夏文芳 詹丽英 方小雨 张亮 詹娜 禹荣 黄丽 朱垒

摘要:脓毒症所致重症感染往往导致多器官功能不全,如心功能不全、肾功能不全、肝功能损伤、脓毒症脑病、凝血功能障碍等。严重感染不仅导致全身炎症反应风暴,同时可诱发脾脓肿形成,甚至自发性脾破裂出血。自发性脾破裂起病隐匿,症状不典型,通常无明显外伤病史,临床容易漏诊。本例脓毒症患者突发左上腹疼痛、血红蛋白进行性下降,紧急完善腹部CT检查,考虑脾破裂出血。剖腹探查术术中发现腹腔大量积血,脾周血肿明显伴脾脏包膜撕裂,遂行全脾切除术。病理提示:脾脏慢性炎症细胞浸润,考虑脾脓肿伴出血。术后患者血色素平稳,腹痛症状明显好转。关键词:脓毒症; 脾破裂; 出血; 金黄色葡萄球菌; 脾切除术基金项目:湖北省重点实验室开放项目(2021KFY018)
Sepsis with spontaneous splenic rupture and hemorrhage: A case report
LIU Zhoua, XIA Wenfanga, ZHAN Liyinga, FANG Xiaoyua, ZHANG Liangb, ZHAN Nac, YU Rongd, HANG Lid, ZHU Leie. (a. Department of Critical Care Medicine, b. Department of Radiology, c. Department of Pathology, d. Department of Gastroenterology, e. Department of Hepatobiliary Surgery, Renmin Hospital of Wuhan University, Wuhan 430060, China)
Corresponding author:ZHAN Liying, 2582062108@qq.com (ORCID:0000-0002-7368-9932)
Abstract:Severe infections due to sepsis often result in multi-organ insufficiency, such as cardiac insufficiency, renal insufficiency, hypohepatia, septic encephalopathy, coagulation dysfunction etc. Severe infections not only cause inflammatory storm, but also induce spleen abscess, and even combined with spontaneous splenic rupture hemorrhage. Spontaneous splenic rupture has an insidious onset, usually without a history of trauma, and is easily missed diagnosis. In this case, the patient with sepsis had sudden onset of abdominal pain and progressive decrease in hematocrit, thus the abdominal CT was immediately performed. The perisplenic mixed high-density shadow indicated splenic hemorrhage. After consultation with the department of hepatobiliary surgery, emergency dissection was performed. Splenic hematoma and laceration were found during the operation, thus total splenectomy was conducted. Pathological indicated chronic inflammatory cell infiltration of spleen, spleen abscess with bleeding. After operation, the patients hematocrit was stable, abdominal pain improved significantly, and he was discharged from hospital after systematic therapy.
Key words:Sepsis; Spleen Rupture; Hemorrhage; Staphylococcus Aureus; Splenectomy
Research funding:Key Laboratory Open Project of Hubei Province (2021KFY018)
脓毒症是宿主对严重感染反应失衡所致危及生命的多器官功能障碍,是ICU的常见疾病。脓毒症往往合并多器官功能不全,如心功能不全、肾功能不全、肝损伤[1]、脓毒症相关性脑病、凝血功能障碍等;一旦感染播散至腹腔,还可诱发脾脓肿,甚至自发性脾破裂出血,危及生命。自发性脾破裂发病率低,起病隐匿,症状不典型,临床容易漏诊。本例脓毒症患者反复高热,突发意识障碍、血压骤降伴血红蛋白進行性下降,急诊腹部CT示:脾周混杂高密度影,考虑脾破裂出血。肝胆外科急诊行剖腹探查术,术中发现脾脏包膜破裂、脾周血肿明显,遂行全脾切除术。现报告1例脓毒症合并自发性脾破裂出血病例,旨在提高对本病的认识,采取积极措施,降低病死率,改善临床结局。
1病例资料
患者男性,45岁。患者1个月前(2022年9月15日)无明显诱因出现畏寒发热,最高体温39.0 ℃,于当地医院就诊,给予美罗培南联合万古霉素抗感染、盐酸溴己新化痰、补液等对症支持治疗。10月18日患者突发氧合下降,血压降低,紧急气管插管、补液升压后,转诊至武汉大学人民医院。既往史:2019年6月于本院行全主动脉弓人工置换+升主动脉部分切除+支架象鼻术,术后声带麻痹、声嘶;精神分裂病史10余年,间断口服奥氮平、丙戊酸钠缓释片;否认吸烟史、饮酒史、高血压、糖尿病、肝炎、结核等特殊病史。入院查体:体温36.3 ℃;心率142次/min;呼吸26次/min;血压76/60 mmHg,去甲肾上腺素泵维持,镇痛镇静状态,气管插管呼吸机辅助呼吸,极度消瘦貌,全身皮肤巩膜无黄染,浅表淋巴结无肿大,胸前正中可见长约20 cm的手术疤痕,颈软,气管居中,心率齐,各瓣膜区未闻及病理性杂音,双肺呼吸音粗,满布痰鸣音及湿啰音,腹软,肝脾肋下未触及,无压痛及反跳痛,骶尾部及髋部皮肤压疮,双下肢无水肿。
入院后完善相关辅助检查,血常规:WBC 8.72 ×109/L, Neu% 82.30%, RBC 2.57×1012/L, Hb 79 g/L, PLT 27×109/L, CRP 240 mg/L, SAA 300 mg/L;凝血功能:PT 13.7 s, APTT 37.2 s, TT 12.60 s, FIB 3.54 g/L, D-dimmer 30.06 mg/L, AT-Ⅲ 38.7%;氨基末端脑钠肽:pro-BNP 13 897 pg/mL;降钙素原:PCT 74.15 ng/mL;心梗三项:MYO 1 000 μg/L, cTnI 0.165 ng/mL;生化:ALT 25 U/L, AST 59 U/L, Alb 21.80 g/L, BUN 19.60 mmol/L, Cr 213 μmol/L, K 3.25 mmol/L, GRF 31.42 mL/min;血气分析:pH 7.41, PaO2152 mmHg, PaCO235 mmHg, Lac 3.0 mmol/L;真菌G试验:77.091 pg/mL。细胞免疫功能:CD3 60.55, CD4 53.46, CD8 7.26, CD4/CD8 7.36;体液免疫:IgG 8.83, C3 0.433, C4 0.04。下呼吸道病原菌(10/20):金黄色葡萄球菌及耐甲氧西林葡萄球菌-DNA阳性。呼吸道病原学高通量测序(10/21):金黄色葡萄球菌(覆盖度99.54%)、肺炎链球菌(覆盖度99.28%)、白色念珠菌(覆盖度95.28%)。外周血病原学高通量测序(10/21):金黄色葡萄球菌(覆盖度99.61%)、热带念珠菌(覆盖度 93.27%)。血培养(10/23):金黄色葡萄球菌。尿培养(10/24):白色念珠菌。心电图(10/18):房性心动过速;V2导联ST段抬高。腹部彩超(10/19):脾脏包膜完整,实质回声分布均匀;腹水彩超(10/19):未见明显异常;心脏彩超(10/19):主动脉夹层术后,置换人工血管未见明显异常。入院诊断:(1)脓毒血症,脓毒性休克,金黄色葡萄球菌性败血症;(2)急性呼吸衰竭;(3)肾功能不全;(4)肝功能不全;(5)血小板减少;(6)心功能不全;(7)低蛋白血症;(8)低钾血症;(9)精神分裂症;(10)凝血功能异常;(11)受压区压疮;(12)心律失常;(13)血管支架植入术后状态。
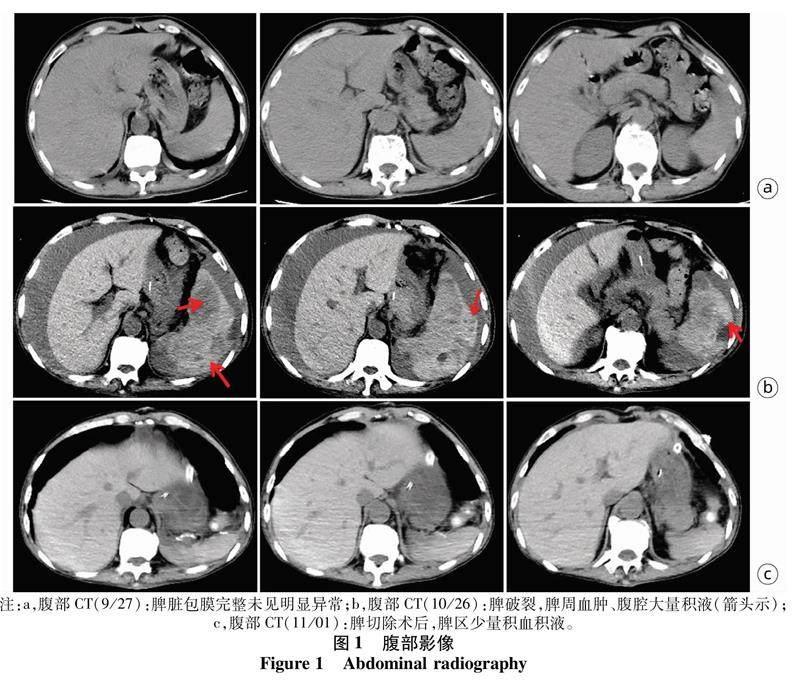
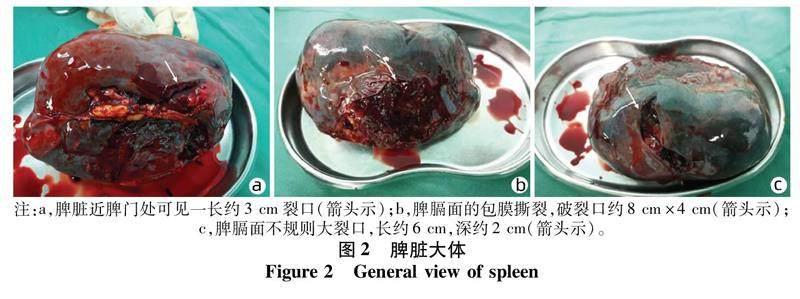
第一天患者反复高热,留取血、尿、痰培养,完善纤支镜检查并加强抗感染治疗。第二天,完善外周血行高通量测序(next generation sequencing, NGS)。第三天,试脱机半小时后血气未见明显异常(pH 7.46, PaO2135 mmHg, PaCO233 mmHg),遂拔除气管插管。第四天,血培养提示金黄色葡萄球菌感染,加用万古霉素抗感染。第五天,患者仍有发热,体温高达39.5 ℃,胸片提示双肺散在斑片影,外周血NGS及血培养均提示金黄色葡萄球菌感染,同时外周血及痰NGS提示真菌感染(热带念珠菌、白色念珠菌),加用米卡芬净抗真菌治疗。第六天,患者突发血压骤降(55/30 mmHg),呼之不应,氧饱和度测不出,遂紧急行气管插管术。第七天,患者血红蛋白从102 g/L骤降至68 g/L,肝酶急剧升高(ALT 569 U/L, AST 1 474 U/L)伴肾功能不全(BUN 32.1 mmol/L, Cr 196 μmol/L)及严重低蛋白血症(Alb 26.5 g/L)。考虑消化道出血可能,输注浓缩红细胞,同时加强抑酸抑酶等对症处理。第八日,患者病情继续恶化,体温峰值39.9 ℃,重度贫血、肝肾功能不全及凝血功能障碍(PT 16.7 s, APTT 42.8 s, D-dimmer 92.97 mg/L)进行加重。患者反复多次输血(4U浓缩红)后血红蛋白未见明显上升,无呕血及黑便,查体全腹膨隆、左上腹压痛可疑阳性,紧急完善腹部检查。腹部B超(10/27):脾周异常包块声影伴腹腔积液。腹部CT(10/27):脾脏低密度影,脾周混杂高密度影,考虑出血;腹腔大量积液(图1)。肝胆外科及介入急会诊,考虑脾破裂出血可能性较大,急诊行剖腹探查术。术中见脾脏肿大,近脾门及脾膈面分别见长约3 cm及6 cm裂口,深约2 cm,部分被膜撕脱(图2),行全脾切除术。术后第一天,患者仍高热39.6 ℃,给予物理降温、强化抗感染、小剂量激素联合双氯芬酸钠栓对症处理后,体温逐渐恢复正常。术后第二天,考虑患者肾功能不全以及药物肾毒性,停万古霉素改为达托霉素联合米卡芬净抗感染治疗。术后第三天,评估后拔除气管插管给予高流量氧疗,继续抗感染、补液等对症支持治疗。术后病理报告(11/3):脾門处血管呈慢性炎症,免疫组化示:CD20(灶状+),CD3(灶状+), CD5(灶状+),CD56(-),Ki-67(+, 低增殖),原位杂交:EBER(-),考虑脾脓肿伴出血(图3)。术后第七天,患者神志清楚,无发热,感染指标较前显著下降,转回当地医院继续治疗。
出院诊断:(1)脾脓肿,非创伤性脾破裂;(2)脓毒性休克,金黄色葡萄球菌性败血症;(3)多脏器功能衰竭;(4)热带念珠菌感染;(5)重症肺炎;(6)腹腔感染;(7)真菌性泌尿道感染;(8)电解质紊乱;(9)血小板减少;(10)低蛋白血症;(11)房性心动过速;(12)凝血功能异常,低纤维蛋白原血症;(13)多浆膜腔积液,胸腔积液,腹腔积液,盆腔积液;(14)高胆红素血症,胆汁淤积;(15)受压区压疮;(16)精神分裂症;(17)血管支架置入术后状态。
2讨论
脓毒症是ICU的常见疾病,病死率较高[2],以脓毒症休克[3]、难治性低血压、微循环障碍、乳酸进行性升高为特点,导致多器官功能不全甚至衰竭[4]。脓毒症合并脾脓肿,诱发自发性脾破裂出血十分罕见[5],发病率仅为0.1%~0.5%[6],临床上容易忽视及漏诊,导致严重不良结局。
自发性脾破裂是指无明确外伤史而发生的脾脏突发性或隐匿性破裂。Rokitansky于1861年首次在2例白血病患者中提出此概念[7]。嗜酸粒细胞增多症[8]、传染性单核细胞增多症[9]、恶性肿瘤[10-11]、血液系统疾病[12]、白血病[13]、结核[14]、疟疾[15]、伤寒[16]、慢性肝炎[17]、立克次体[18]及血吸虫感染[19]等,均可导致脾脏充血肿大且脆性增加,最终诱发脾破裂。脾脏自身病理性改变,如脾囊肿[20]、脾血管瘤[21]及脾血管肉瘤[22]等,往往影响单核巨噬细胞系统导致脾脏脆性增加,易诱发脾破裂。感染性疾病、炎症及免疫系统异常激活,诱发脾肿大或与周围组织粘连,脾脏活动度降低,因此腹压增加或体位改变等动作即可诱发自发性脾破裂[23]。由于无明确外伤史且缺乏典型症状和体征,本病极易漏诊[6]。患者一般无明显诱因,咳嗽、喷嚏、排便、剧烈呕吐、分娩等腹压增加动作,导致膈肌及腹肌强烈收缩,均可诱发脾破裂[20]。自发性脾破裂患者通常表现为突发左上腹持续疼痛,伴恶心呕吐、腹胀等症状,严重时可伴重度贫血或循环衰竭,危及生命。部分患者可出现Kehrs征,阳性率70%~80%[24],即脾周积血刺激左侧膈肌,导致左上腹疼痛及左肩放射痛。因左肩放射痛,Kehrs征易被误诊为急性心血管疾病。诊断性腹腔穿刺、B超、CT及血管造影均为该病常见的辅助检查。腹腔穿刺术简单实用,若抽出不凝血,可协助诊断。B超/CT可间接显示脾破裂的位置、范围及深度,脾周血肿及腹腔积血情况。血管造影则对血管破裂的自发性脾破裂诊断价值较高。若脾破裂严重出血,出血量大且速度快,患者常表现为重度贫血或低血压休克,甚至循环衰竭,危及生命。
脓毒症导致脾脓肿发生相对较少,而脾脓肿合并自发性脾破裂则十分罕见[5],其机制尚不明确。本例自发性脾破裂出血可能与以下多因素相关:(1)脓毒症金黄色葡萄球菌血流感染,侵袭脾脏导致急慢性炎症,大量白细胞及中性粒细胞聚集,IL-1、IL-6等炎症因子释放,免疫损伤导致脾脏局部脓肿、坏死,诱发自发性脾破裂[25];(2)感染导致机体免疫系统异常激活,脾脏作为外周免疫应答的重要场所,启动T、B淋巴细胞活化,炎症信号通路激活,血管通透性增加导致脾肿胀[26];(3)重症感染导致凝血功能异常,抗凝血酶Ⅲ减少,蛋白C及S活性降低,D-二聚体升高,血液高凝,脾脏微血管内纤维蛋白血栓增多,血流灌注不足[27];(4)脓毒症患者内毒素异常升高导致脾交感神经兴奋,神经电活动强度升高,潜伏期缩短,脾脏血流灌注减少;(5)金黄色葡萄球菌分泌致病性溶血素,可诱导脾脏细胞发生依赖于caspase的程序性死亡,同时促使小血管平滑肌收缩、痉挛,导致血流阻滞和组织局部缺血坏死[28];(6)金黄色葡萄球菌释放穿孔素、溶血素等,干扰固有免疫系统,诱导机体IL-1、IL-6分泌;同時,诱导中性粒细胞凋亡,抑制巨噬细胞吞噬活性,介导脾脏免疫损伤[25]。最新研究[29]表明COVID-19感染也是患者自发性脾破裂的高危因素,SARS-CoV-2可损伤脾脏及淋巴结,导致脾萎缩,同时微血栓形成及凝血功能异常,均可导致脾脏血流灌注不足甚至脾破裂。
本例脓毒症合并自发性脾破裂出血经验如下:首先,本例脓毒症患者证实为金黄色葡萄球菌感染,极易导致细胞坏死甚至脾脓肿。金黄色葡萄球菌释放溶血素、穿孔素,侵蚀血管可致局灶性出血逐渐融合,脾脏血肿,严重时可导致包膜破裂出血。其次,严重血流感染的患者,需考虑是否合并其他脏器感染。既往支架异物置入史,反复多次血流感染的患者,治疗过程中发生不明原因血红蛋白下降,需警惕脾破裂的可能。本例患者血压骤降伴不明原因血色素骤降,且无呕血便血症状,排除消化道出血的同时,需积极完善腹部检查。临床诊疗不仅需选择敏感抗生素,同时需考虑药物的代谢及分布,选择对靶器官通透性更优的药物。自发性脾破裂一旦确诊,需立即制订诊疗方案,包括手术治疗及非手术治疗,以手术治疗为主。本例脓毒症患者合并自发性脾破裂,需强调多学科合作诊疗模式。ICU医师需不断强化对脓毒症的认知水平,关注病情变化的同时积极思考,若患者突发左上腹疼痛伴血红蛋白骤降,需考虑本病可能,密切监测生命体征并完善相关辅助检查,一旦确诊尽早治疗,降低病死率,及时挽救生命。
伦理学声明:本例报告已获得患者及患者家属知情同意。利益冲突声明:本文不存在任何利益冲突。作者贡献声明:柳舟、张亮、夏文芳负责课题设计,资料分析,撰写论文;詹丽英负责修改论文;方小雨参与收集数据及修改论文;詹娜负责病理阅片及病理图注;张亮负责影像阅片及影像图注;黄丽、禹荣拟定写作思路,指导撰写文章;朱垒负责外科手术记录及手术图片收集,参与最后定稿。
参考文献:
[1]XING BM, GUO N, NING HH, et al. Sepsis liver damage and autophagy[J/CD]. Chin J Liver Dis (Electronic Version), 2021, 13(3): 37-41. DOI: 10.3969/j.issn.1674-7380.2021.03.006.邢博民, 郭娜, 宁海慧, 等. 脓毒症肝损伤与自噬[J/CD]. 中国肝脏病杂志(电子版), 2021, 13(3): 37-41. DOI: 10.3969/j.issn.1674-7380.2021.03.006.
[2]DEMERLE KM, ANGUS DC, BAILLIE JK, et al. Sepsis subclasses: A framework for development and interpretation[J]. Crit Care Med, 2021, 49(5): 748-759. DOI: 10.1097/CCM.0000000000004842.
[3]WANG Y, CAO ZX, YU JH, et al. Correlation between changes of coagulation - related parameter and prognosis in ICU patients with septic[J]. J Clin Exp Med, 2022, 21(14): 1519-1523. DOI: 10.3969/j.issn.1671-4695.2022.14.017.王艷, 曹志新, 于金辉, 等. ICU脓毒症患者凝血相关参数的变化与预后关系的研究[J]. 临床和实验医学杂志, 2022, 21(14): 1519-1523.DOI: 10.3969/j.issn.1671-4695.2022.14.017.
[4]FONT MD, THYAGARAJAN B, KHANNA AK. Sepsis and septic shock - basics of diagnosis, pathophysiology and clinical decision making[J]. Med Clin North Am, 2020, 104(4): 573-585. DOI: 10.1016/j.mcna.2020.02.011.
[5]ATHEY R, BARTON LL, HORGAN LF, et al. Spontaneous splenic rupture in a patient with pneumonia and sepsis[J]. Acute Med, 2006, 5(1): 21-23.
[6]KOCAEL PC, SIMSEK O, BILGIN IA, et al. Characteristics of patients with spontaneous splenic rupture[J]. Int Surg, 2014, 99(6): 714-718. DOI: 10.9738/INTSURG-D-14-00143.1.
[7]MOURATO NUNES I, PEDROSO AI, CARVALHO R, et al. Chronic lymphocytic leukaemia and spontaneous rupture of spleen[J]. BMJ Case Rep, 2018, 2018: bcr2017221692. DOI: 10.1136/bcr-2017-221692.
[8]SHAJIL C, SATHISHKUMAR D, GEORGE K, et al. Spontaneous splenic rupture: A rare complication in eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)[J]. Indian J Dermatol Venereol Leprol, 2022, 88(3): 392-395. DOI: 10.25259/IJDVL_584_20.
[9]KUZMAN I, KIRAC P, KUZMAN T, et al. Spontaneous rupture of the spleen in infectious mononucleosis: case report and review of the literature[J]. Acta Med Croatica, 2003, 57(2): 141-143.
[10]SWAID F, SHULMAN K, ALFICI R, et al. Spontaneous splenic artery rupture in a patient with an unclassified malignant spindle cell tumor of the spleen: report of a case[J]. Int J Surg Oncol (N Y), 2017, 2(3): e14. DOI: 10.1097/IJ9.0000000000000014.
[11]MIRFAZAELIAN H, ORYAN A, DAVARI A, et al. Spontaneous splenic rupture in melanoma[J]. Case Rep Pathol, 2014, 2014: 865453. DOI: 10.1155/2014/865453.
[12]DUNPHY L, ABBAS SH, PATEL A, et al. Spontaneous splenic rupture: a rare first presentation of diffuse large B cell lymphoma[J]. BMJ Case Rep, 2019, 12(8):e231101. DOI: 10.1136/bcr-2019-231101.
[13]LI XQ, LI YF, YU M, et al. B-cell prolymphocytic leukemia with spontaneous splenic rupture as the first symptom: a clinicopathologic analysis of one case [J]. J Diag Pathol, 2021, 28(1): 9-13. DOI: 10.3969/j.issn.1007-8096.2021.01.003.
李小强, 李英凤, 郁敏, 等. 以自发性脾脏破裂为首发症状的B细胞前淋巴细胞性白血病1例临床病理观察[J]. 诊断病理学杂志, 2021, 28(1): 9-13. DOI: 10.3969/j.issn.1007-8096.2021.01.003.
[14]ZHANG Y, ZHANG J, CHEN T, et al. Spontaneous splenic rupture in an acute leukemia patient with splenic tuberculosis: A case report[J]. Mol Clin Oncol, 2017, 6(2): 209-213. DOI: 10.3892/mco.2016.1120.
[15]LIU J. Spontaneous splenic rupture caused by malaria in South Sudan peacekeeping mission two cases reports [J]. Chin J Disaster Med, 2018, 6(1): 50-51. DOI: 10.13919/j.issn.2095-6274.2018.01.012.刘健. 南苏丹维和任务区疟疾导致自发性脾破裂2例[J]. 中华灾害救援医学, 2018, 6(1): 50-51. DOI: 10.13919/j.issn.2095-6274.2018.01.012.
[16]GEORGE P, AHMED A, MAROLI R, et al. Peritonitis secondary to ruptured splenic abscess: a grave complication of typhoid fever[J]. Asian Pac J Trop Med, 2012, 5(12): 1004-1006. DOI: 10.1016/S1995-7645(12)60191-6.
[17]OKUBO S, KIRIYAMA K, USUI T, et al. Spontaneous splenic vein rupture complicating liver cirrhosis: an autopsy case report[J]. Nihon Shokakibyo Gakkai Zasshi, 2013, 110(3): 426-431.
[18]PENG Y, LI TF, CHEN M, et al. Rickettsial infection with splenic artery malformation and rupture: a case report [J]. Chin J Endemiol, 2022, 41(8): 677-678. DOI: 10.3760/cma.j.cn231583-20210507-00151.彭昱, 李鐵丰, 陈梅, 等. 立克次体感染伴发脾动脉畸形破裂1例[J]. 中华地方病学杂志, 2022, 41(8): 677-678. DOI: 10.3760/cma.j.cn231583-20210507-00151.
[19]OKAMOTO K, BROWN JD. Hepatosplenic schistosomiasis presenting as spontaneous hemoperitoneum in a Filipino immigrant[J]. Am J Med Sci, 2013, 346(4): 334-337. DOI: 10.1097/MAJ.0b013e31828f4bee.
[20]RES LC, KNOOK M, HAZELBAG HM, et al. Spontaneous rupture of a non-parasitic splenic cyst[J]. BMJ Case Rep, 2019, 12(10): e231473 . DOI: 10.1136/bcr-2019-231473.
[21]LIN JL, LIN C, WANG HL, et al. Splenic artery embolization and splenectomy for spontaneous rupture of splenic hemangioma and its imaging features[J]. Front Cardiovasc Med, 2022, 9: 925711. DOI: 10.3389/fcvm.2022.925711.
[22]WHEELWRIGHT M, SPARTZ EJ, SKUBITZ K, et al. Primary angiosarcoma of the spleen, a rare indication for splenectomy: a case report[J]. Int J Surg Case Rep, 2021, 82: 105929. DOI: 10.1016/j.ijscr.2021.105929.
[23]WANG B, ZHU XG, JIANG LH, et al. Diagnosis and treatment of spontaneous splenic rupture in 13 cases [J]. Tian Jing Med J, 2019, 47(9): 962-965. DOI: 10.11958/20191083.王斌, 朱新国, 蒋林华, 等. 自发性脾破裂13例诊治分析[J].天津医药, 2019, 47(9): 962-965. DOI: 10.11958/20191083.
[24]HU MR, XU DZ. Spontaneous splenic rupture [J]. J Clin Surg, 2006, 14(7): 411-412. DOI: 10.3969/j.issn.1005-6483.2006.07.008.胡铭荣, 徐德征. 自发性脾破裂[J]. 临床外科杂志, 2006, 14(7): 411-412. DOI: 10.3969/j.issn.1005-6483.2006.07.008.
[25]ZOU YX, HOU YX. Analysis of diagnosis and treatment of Staphylococcus aureus pneumonia and its extrapulmonary lesions [J]. Chin J Appl Clin Pediatr, 2020, 35(16): 1219-1224. DOI: 10.3760/cma.j.cn101070-20200403-00574.鄒映雪, 侯宇欣. 金黄色葡萄球菌肺炎及其肺外损害的诊治分析[J]. 中华实用儿科临床杂志, 2020, 35(16): 1219-1224. DOI: 10.3760/cma.j.cn101070-20200403-00574.
[26]ZHAO HC, CHEN CZ, SONG HQ, et al. Single-cell RNA sequencing analysis reveals new immune disorder complexities in hypersplenism[J]. Front Immunol, 2022, 13: 921900. DOI: 10.3389/fimmu.2022.921900.
[27]de BACKER D, RICOTTILLI F, OSPINA-TASCN GA. Septic shock: a microcirculation disease[J]. Curr Opin Anaesthesiol, 2021, 34(2): 85-91. DOI: 10.1097/ACO.0000000000000957.
[28]ZHENG F, ZHOU TT, SUN QN, et al. Recent progress in Staphylococcus aureus α-hemolysin [J]. Chin J Microbiol Immunol, 2017, 37(10): 795-801. DOI: 10.3760/cma.j.issn.0254-5101.2017.10.013.郑峰, 周婷婷, 孙倩男, 等. 金黄色葡萄球菌α-溶血素的研究进展[J]. 中华微生物学和免疫学杂志, 2017, 37(10): 795-801. DOI: 10.3760/cma.j.issn.0254-5101.2017.10.013.
[29]SHI HY, QUAN PP, CHU CL, et al. Diagnosis and treatment of spontaneous splenic rupture associated with severe acute respiratory syndrome coronavirus 2 [J]. J Clin Hepatol, 2022, 38(7): 1694-1696. DOI: 10.3969/j.issn.1001-5256.2022.07.046.师鸿运, 权盼盼, 褚成龙, 等. 新型冠状病毒相关自发性脾破裂的诊治[J]. 临床肝胆病杂志, 2022, 38(7): 1694-1696. DOI: 10.3969/j.issn.1001-5256.2022.07.046.
收稿日期:2022-11-12;录用日期:2022-12-22
本文编辑:王亚南
引证本文:LIU Z, XIA WF, ZHAN LY, et al. Sepsis with spontaneous splenic rupture and hemorrhage: A case report [J]. J Clin Hepatol, 2023, 39(8): 1926-1931.

