Spontaneous dislocation of a toric implantable collamer lens resulting in corneal endothelial decompensation: a case report and review of the literature
Li Zhang, Yan-Xi Li, Chun-Yan Lei, Lin Wang, Mei-Xia Zhang
Sichuan University West China Hospital, Chengdu 610041,Sichuan Province, China
Dear Editor
We present a case of spontaneous dislocation of a toric implantable collamer lens (TICL) resulting in corneal endothelial decompensation 8y after implantation. Since 2006,by helping people take off their glasses, the Visian TICL (Staar Surgical Co, Monrovia, CA, USA) have gained popularity in China. Though complications of intraocular pressure(IOP) elevation, cataract formation and endothelial damage exist as relevant problems, implantable collamer lens (ICL)implantation has been generally accepted as a viable option to correct moderate to high ametropia[1‐2].
Dislocation of ICLs and corneal decompensation are both rare complications as described in previous literature. To our best knowledge, this is the first report of spontaneous dislocation of a TICL resulting in corneal endothelial decompensation with the TICL behind the iris. By reviewing the literature,we summarized the clinical characters and potential factors leading to postoperative ICL dislocation in previously reported cases of ICL dislocation.
Ethical ApprovalThe study was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from the patients.
Case ReportA 47‐year‐old gentleman presented to us in May 2021 with complaints of foggy vision with foreign body sensation and photophobia in his right eye of 1y duration.He received bilateral ICL implantations for correction of high ametropia in 2013. No medical history of systemic or ocular diseases was presented by the patient. His preoperative best‐corrected visual acuity (BCVA) was 20/20 in the right eye (refraction, -18.00/-2.00×5°) and 20/30 in the left eye(refraction, -20.5/-3.00×170°). In the right and left eye,respectively, the anterior chamber depths (the distance between the corneal endothelium and the anterior lens capsule) were 2.80 and 2.71 mm, the white‐to‐white (WTW) diameters were 10.9 and 11.1 mm, and the corneal thickness were both 533 μm.Laser iridotomy was performed in both eyes two months before the TICL implantation surgery. Data was calculated basing on the TICL software (STAAR Surgical Company, Monrovia,CA, USA). According to the results, we chose the TICMV4 model, with a power of -23.00/+2.5×95° for the right eye and-23.00 sphere for the left eye. Ametropia of the left eye wasn’t fully corrected because no matched ICL was manufactured at the time. The diameter of ICLs were 11.5 mm for both eyes.Surgery in both eyes was uneventful. Postoperatively, the TICL in the right eye slightly rotated and prolapsed. With consent,another TICL with a diameter of 12.0 mm and a power of-23.00/+2.5×100° was later implanted in the right eye after the former one was explanted. However, the TICL again prolapsed with slight rotation postoperatively. Since the optical zone of the TICL still remained in the central front of the pupil, the patient regained a satisfactory distance uncorrected visual acuity (UCVA) of 20/20. Clinical decision for explantation of the TICL in the right eye was made. However, the man refused to take further surgery and was lost to follow up in the following 8y.
On presentation, UCVA was hand motion for the right eye and 20/200 (refraction, -4.00) for the left eye. IOP was 20 mm Hg for the right eye and 18 mm Hg for the left eye. Slit‐lamp examination after pupillary dilatation showed rotation of approximately 45° and prolapse of the TICL in the right eye with corneal edema (Figures 1 and 2). The corneal endothelial cell density was 2281 cells/mm2for the left eye, while unobtainable for the right eye. Examination of ultrasound biomicroscopy (UBM) showed that the TICL was still behind the iris, but the edges of the TICL arched forward into the anterior chamber (Figure 3). The patient denied history of trauma or strenuous activity. And it had been nearly one year since he started experiencing blurred vision with foreign body sensation and photophobia in his right eye.
With consent, phacoemulsification and intraocular lens implantation after explantation of the TICL was performed on his right eye, and a capsular tension ring was also implanted due to detected unstable zonules. Three months later,descemet’s stripping endothelial keratoplasty was performed for restoring visual acuity.
Dislocation of an ICL has been described several times in previous reports[3‐10](Table 1) and most of the cases were related with ocular trauma[3,6‐7,9‐10]. Occiput injury had been reported once as the reason for ICL dislocation[5]. And the author hypothesized the phakic ICL was pushed forward by the tremendous shock wave from backside in condition of a relatively dilated pupil in dark environment.
Spontaneous dislocation of an ICL was a relatively rarer situation which had also been described twice in the literature[4,8]. The first case was reported in 2005[4], which was relevant with rupture of the zonules. The recent one had reported a case of spontaneous dislocation of the ICL into the anterior chamber due to mydriasis induced by oral antidepressants[8]. Corneal endothelial decompensation was not presented in any of these cases except for one, in which the ICL was dislodged into the anterior chamber with corneal touch because of ocular blunt trauma[3].
Ciliary body morphology is now accessible using UBM, which is helpful for us to observe the intraocular position of ICLs[11].In a recent case report by Chenet al[12], spontaneous rotation of approximately 90° of a TICL reoccurred at one day and a month after implantation. A posteriorly positioned ciliary body,a short and small ciliary process and a shallow ciliary sulcus were found in UBM images from this patient. Part quadrant of the ciliary sulcus lost its normal length and exhibited a nearly obtuse angle. A replacement of the TICL with a larger size non‐toric ICL was performed, and the post‐operative outcome in follow‐up was excellent. The varied structure of ciliary sulcus in this case is quite similar to that of our case (Figure 4). With the change of accommodation states, the footplates may slide down to the ciliary body or even get a chance to cross over the small ciliary body and finally rest on the zonules. Besides,hypermyopia is typically accompanied by weak zonules which may easily be ruptured by the misplaced footplates of a TICL with the assistance of gravity, causing the TICL to subluxate inferiorly.

Figure 1 Anterior segment photograph showing prolapse of the toric implantable collamer lens in the right eye with corneal edema.
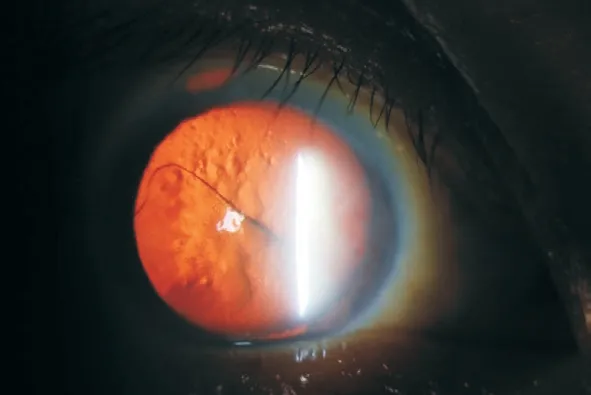
Figure 2 Largely rotated and inferiorly subluxated toric implantable collamer lens.

Figure 3 Ultrasound biomicroscopy showing that the TICL was still behind the iris, but the edges of the TICL arched forward into the anterior chamber TICL: Toric implantable collamer lens.

Figure 4 Ultrasound biomicroscopy showing a posteriorly positioned ciliary body, a short and small ciliary process and a shallow ciliary sulcus.
Endothelial damage was widely concerned for the safety after ICL implantation. Endothelial damage caused by ICL‐endothelium touch is easy to understand, but for the present case, it’s strange and rare because the TICL remained behind the iris without visual endothelium touch. The patient presented with a shallow anterior chamber (2.80 mm for the right eye), and in UBM images, we found the edge of the TICL arched forward into the anterior chamber. Hence, we assume that in dark environment, when the pupil dilated, the TICL may get a chance to touch the corneal endothelium and cause damage, especially when the patient rubbed the eye or sleep with a prone position. The symptoms might be slight and was ignored by the patient, but the damage accumulated, and finally resulted in corneal endothelial decompensation.This unique case demonstrates the potential association of dislocation of ICLs with the ciliary body morphology and zonular weakness. And corneal decompensation may develop under rare conditions even though the ICL still remains behind the iris. Early reposition or explantation of dislocated ICLs is necessary to avoid further complications. UBM images should be carefully examined in the preoperative assessment of ICL implantation to detect morphological abnormalities.Surgeons should pay special attention to hypermyopia patients with zonular weakness and those with unstable ICL position intraoperatively and postoperatively. Patient education and routine follow‐up examination are also of vital importance,because ignorance of the ocular symptoms may result in severe consequences.

Table 1 Review of cases of ICL dislocation
ACKNOWLEDGEMENTS
Authors’ contributions:Zhang L, Wang L conceived the idea for the case study and followed the patient. Zhang L, Li YX,Lei CY wrote the article and Wang L and Zhang MX revised it critically for important intellectual content. All authors read and approved the final manuscript.
Foundation:Supported by 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (No.ZYJC21025).
Conflicts of Interest: Zhang L, None;Li YX,None;Lei CY,None;Wang L, None;Zhang MX,None.
 International Journal of Ophthalmology2023年1期
International Journal of Ophthalmology2023年1期
- International Journal of Ophthalmology的其它文章
- Instructions for Authors
- Morphological and functional changes in the macular area in diabetic macular edema after a single intravitreal injection of aflibercept
- Macular vascularisation changes analysed using OCT angiography after successful rhegmatogenous retinal detachment repair
- Comparison of success rate and intraocular pressure spikes between selective laser trabeculoplasty and micropulse laser trabeculoplasty in African American and Hispanic patients
- Efficacy of custom-made soft keratoconus lenses on corneal aberrations and photic phenomena in patients with keratoconus: a corneal topography imaging based study
- Clinical observation of recombinant human nerve growth factor in the treatment of neurotrophic keratitis
