A case of persistent refractory hypoglycemia from polysubstance recreational drug use
Jie Er Janice Soo, Mingwei Ng, Terence Kee Liem Chong, Boon Kiat Kenneth Tan, R Ponampalam
Department of Emergency Medicine, Singapore General Hospital, 169608, Singapore
Dear editor,
Studies have revealed a significant prevalence of mixed substance abuse,[1-3]and a focused approach towards polysubstance use has been emphasized.[4]Among recreational drugs, cases of hypoglycemia from ecstasy,[5]amphetamine,[6]eutylone,[7]and cannabinoid[8]use have been reported, but none of these cases have had persistent refractory hypoglycemia. We present a case of persistent refractory hypoglycemia in a patient with polysubstance recreational drug use that included synthetic cannabinoids, amphetamine, and eutylone.
CASE
A middle-aged gentleman presented to the emergency department (ED) with altered mental status and hypoglycemia. He was found lying on his bedroom fl oor with sildenafil oral jelly, tadalafil tablet bottles and an unlabelled white powder with an intravenous drug infusion set surrounding him. He had no significant chronic medication use or past medical history; in particular, he did not have diabetes mellitus, nor was he on any insulin or oral hypoglycemic agents.
On arrival at the ED, he was febrile, tachycardic (pulse rate 140-145 beats/min), and hypertensive (blood pressure 155/76 mmHg [1 mmHg=0.133 kPa]). He was initially drowsy and obtunded with chest abrasions and swelling over his lips and mouth.
Laboratory investigations revealed neutrophilic leukocytosis (total white blood cell count 34.2×109/L) with normal hemoglobin and platelet levels. His arterial blood gas showed respiratory acidemia (pH 7.10, partial pressure of carbon dioxide [PCO2] 63 mmHg, bicarbonate 21.5 mmol/L). He also had acute kidney injury (creatinine 236 mmol/L), rhabdomyolysis (creatine kinase >20,000 U/L), myocardial injury (troponin 1,272 ng/L) and transaminitis (alanine aminotransferase 146 U/L, aspartate aminotransferase 625 U/L, normal bilirubin and alkaline phosphatase levels). His serum lactate, ketone, and thyroid levels otherwise returned to normal.
His chest X-ray showed right upper lobe collapse with consolidation, while a non-contrast computed tomography of his brain showed a small acute left parietal subdural hematoma. His 12-lead electrocardiogram showed sinus tachycardia with a heart rate of 140 beats/min and prolonged QTc of 601 ms.
Refractory hypoglycemia
The patient’s capillary blood glucose as checked by the paramedics when they found him obtunded at the scene was 2 mmol/L but was unable to establish intravenous access to administer glucose. On arrival to the ED, he was started on a dextrose infusion, and his mentation improved markedly. He became combative and required sedation.
However, he developed recurrent episodes of hypoglycemia. His capillary blood glucose was 2.6 mmol/L 3 h later, requiring repeated administrations of dextrose boluses in the ED. Even after he was admitted to the inpatient unit, his glucose levels remained borderline for the next 72 h, and he was subsequently started on 50 μg octreotide every 12 h on the second day of his admission while the dextrose drips were continued.
Multiorgan involvement
The patient’s blood pressure in the ED was labile, with the lowest reading of 57/30 mmHg. He was started on noradrenaline after he remained hypotensive despite taking two liters of crystalloids. He was intubated because of severe respiratory acidosis and admitted to the intensive care unit (ICU). In the ICU, he required single inotropic support (noradrenaline up to 0.2 μg/[kg·min]), which was weaned and discontinued on day five. His mental status improved two days later. His ventilator requirements were also minimal (max fraction of inspired oxygen [FiO2] 40%), and he was extubated after five days.
The patient was also initiated on renal replacement therapy on the third day of admission after he developed worsening oliguric acute kidney injury from rhabdomyolysis. Dialysis was terminated fifteen days after his renal function fully recovered. His transaminitis peaked on the third day of his admission (aspartate aminotransferase >7,000 U/L, alanine aminotransferase 4,526 U/L) but normalized on discharge as well.
He was moved to the high dependency unit (intermediate level of care between the ICU and general ward) after seven days in the ICU and had a total inpatient stay of 26 d. Apart from the drug overdose, he was also diagnosed with sepsis from communityacquired pneumonia as well as a traumatic subdural hematoma, which was conservatively managed and resolved on interval imaging a month later.
Further history obtained from the patient by the psychiatrist later revealed that he had intentionally overdosed on illicit drugs. He had injected several drugs, including amphetamine, methamphetamine, and N-methyl-D-aspartate (NMDA), intravenously. His blood and urine toxicology samples detected the presence of amphetamine, methamphetamine, eutylone, sildenafil, and synthetic cannabinoid (ADB-BUTINACA hydroxybutyl metabolite), as shown in the report in Table 1.
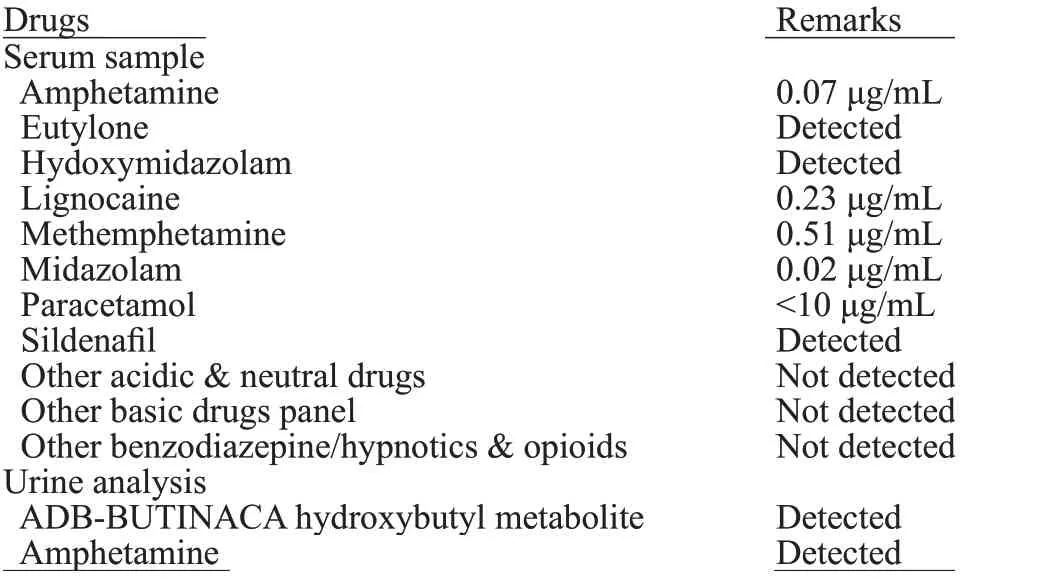
Table 1. Toxicological report
DISCUSSION
We present a case of a patient with polysubstance recreational drug use (synthetic cannabinoid, methamphetamine, amphetamine, eutylone, andsildenafil) who presented with refractory hypoglycemia and multiorgan dysfunction. Although no universal definition for refractory hypoglycemia exists, most researchers describe “refractory” as either a prolonged duration of hypoglycemia over hours to days or as a requirement for high doses of dextrose to normalize glucose levels and maintain euglycemia,[9]as in this case report.
The most likely explanation for the refractory hypoglycemia would be amphetamine and synthetic cannabinoid use compounded by reduced elimination due to renal dysfunction. Experiments studying the physiological effects of amphetamine use on animal models demonstrated an increased prevalence of reactive hypoglycemia.[10]Suggested mechanisms include the direct effect of the pancreas on insulin secretion, changes in glucose metabolism, and changes in receptors of glucose uptake. Despite having significant transaminitis, this patient did not have features suggesting acute liver failure causing hypoglycemia. Nevertheless, there were no insulin or C-peptide levels, which would aid in a better understanding of the mechanisms of hypoglycemia if it may be insulin driven and whether it is endogenous or exogenous.
While sulphonylureas, which would typically be identified on toxicology screening, were absent from this patient’s toxicological report, the possibility that the patient overdosed on sulphonylurea-laced medications must still be carefully considered because the drug screen may not be sufficiently sensitive.[10]The hypoglycemic effects of sulfonylureas or short-acting insulin may persist even after the drug has been eliminated from the circulation.
While dextrose is usually adequate to correct limited episodes of hypoglycemia, refractory hypoglycemia usually demands additional pharmacological interventions, such as octreotide, as dextrose boluses have the potential to stimulate endogenous insulin release leading to rebound hypoglycemia. Octreotide is a longeracting somatostatin analog that inhibits insulin secretion and the insulin response to glucagon. This is useful for the treatment of drug-induced endogenous secretion of insulin. It is hence an antidote for sulfonylurea toxicity.
In comparison, glucagon, another common drug used for hypoglycemia, would have additional improvement of inotropy and chronotropy (due to its effect on adenylate cyclase) and can be given intramuscularly. However, glucagon also increases pancreatic insulin secretion and may have a limited role in patients with low glycogen reserves. Of note, repeated use of glucagon may result in tachyphylaxis. Both octreotide and glucagon are short-acting and will require repeated doses or continuous infusion.
This patient’s polysubstance use also led to significant effects on his cardiac, respiratory, metabolic, and renal systems. Fluctuations and lability in blood pressures were likely a result of an interplay between the sympathomimetic drug overdoses and disease processes: while eutylone and synthetic cannabinoid use may increase his blood pressure, sildenafil, sepsis, and dehydration would otherwise counteract this in particular. Management would therefore require frequent monitoring and reassessment of hemodynamic and fl uid status to guide fluid resuscitation and consideration of early vasoactive agents for titration, especially for patients with intracranial pathology where aggressive blood pressure control is crucial.
Funding:None.
Ethical approval:Not needed.
Confl icts of interest:The authors declare that there is no confl ict of interest.
Contributors:JS proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
 World journal of emergency medicine2023年1期
World journal of emergency medicine2023年1期
- World journal of emergency medicine的其它文章
- Modified qSOFA score based on parameters quickly available at bedside for better clinical practice
- Hyoscine N-butylbromide inhalation: they know, how about you?
- Occurrence of Boerhaave’s syndrome after diagnostic colonoscopy: what else can emergency physicians do?
- A case of chemical eye injuries and aspiration pneumonia caused by occupational acute chemical poisoning
- A case of unusual acquired factor V deficiency
- Cardiogenic shock and asphyxial cardiac arrest due to glutaric aciduria type II
