latrogenic aortic dissection during right transradial intervention in a patient with aberrant right subclavian artery: A case report
Kyungeun Ha, Albert Youngwoo Jang, Yong Hoon Shin, Joonpyo Lee, Jeongduk Seo, Seok In Lee, Woong Chol Kang, Soon Yong Suh
Kyungeun Ha, Division of Cardiology, Department of Internal Medicine, Yonsei University College of Medicine, 50 Yonsei-ro, Seodaemun-gu, Seoul, South Korea
Albert Youngwoo Jang, Yong Hoon Shin, Joonpyo Lee, Jeongduk Seo, Woong Chol Kang, Soon Yong Suh, Division of Cardiology, Department of Internal Medicine, Gil Medical Center,Gachon University College of Medicine, Incheon, South Korea
Seok ln Lee, Department of Thoracic and Cardiovascular Surgery, Gil Medical Center, Gachon University College of Medicine, Incheon, Incheon, South Korea
Abstract BACKGROUND Aberrant right subclavian artery (ARSA) is the most common congenital anomaly of the aortic arch. When patients having such anomalies receive transradial intervention (TRI), aortic dissection (AD) may occur. Herein, we discuss a case of iatrogenic type B AD occurring during right TRI in an ARSA patient, that was later salvaged by percutaneous angioplasty.CASE SUMMARY A 73-year-old man presented to our hospital with intermittent chest pain.Coronary computed tomography (CT) angiography revealed significant stenosis in the left anterior descending artery. Diagnostic coronary angiography was performed via the right radial artery without difficulty. However, we were unable to advance the guiding catheter past the ostium of the right subclavian artery to the aortic arch for percutaneous coronary intervention, while the guidewire tended to go down the descending aorta. The patient suddenly complained of chest and back pain. Emergent CT aortography revealed type B AD propagating to the left renal artery (RA) with preserved renal perfusion. However, after 2 d,the patient suddenly complained of right lower limb pain where the femoral pulse was suddenly undetectable. Follow-up CT indicated further progression of dissection to the right external iliac artery (EIA) and left RA with limited flow. We performed percutaneous angioplasty of the right EIA and left RA without complications. Follow-up CT aortography at 8 mo showed optimal results.CONCLUSION A caution is required during right TRI in ARSA to avoid AD. Percutaneous angioplasty can be a treatment option.
Key Words: Aberrant subclavian artery; Coronary angiography; Aortic dissection; Aortography;Percutaneous transluminal angioplasty; Case report
lNTRODUCTlON
Aberrant right subclavian artery (ARSA) is a congenital anomaly of the aortic arch. In ARSA, the right subclavian artery arises from the descending aorta and passes between the trachea and the esophagus[1]. It is observed in 2% of the general population and is more frequent in patients having Down syndrome with a prevalence of 35%[2,3]. Diverse clinical manifestation associated with ARSA have been reported, including dysphagia, dyspnea and retrosternal pain, although most patients are generally asymptomatic[4,5]. Several cases of ARSA associated with procedure-related aortic dissection (AD)treated surgically or conservatively have been reported[6]. Herein, we report a case of a patient with an incidentally found ARSA during right transradial intervention (TRI), which further resulted in iatrogenic type B AD that was further salvaged by percutaneous angioplasty.
CASE PRESENTATlON
Chief complaints
A 73-year-old man presented to the emergency room with intermittent chest pain and shortness of breath (New York Heart Association class II).
History of present illness
The patient had developed chest pain and dyspnea on exertion in the past 1 mo, which had worsened for 3 d.
History of past illness
The patient also had a history of hypertension as well as smoking (30 pack years).
Physical examination
His initial blood pressure was 130/80 mmHg with a heart rate of 80 beats per minute. Room air oxygen saturation was 97%. He had a regular heartbeat without a murmur. His lung sounds were also clear.There was no abdominal tenderness or pitting edema.
Electrocardiogram showed sinus rhythm with T wave abnormality in leads V1 to V3 without definite ST segment elevation or depression.
Laboratory examinations
Initial cardiac enzyme levels, including creatine kinase-myocardial band and troponin I were within the normal range. The serum creatinine level was normal (0.96 mg/dL).
Imaging examinations
Coronary computed tomography (CT) angiography as an initial screening test revealed significant proximal left anterior descending (LAD) artery stenosis. Percutaneous coronary intervention was decided. Diagnostic angiography was performedviathe right radial artery, which showed 90% stenosis of the mid LAD. We re-inserted the extra backup 3.5 guiding catheter for percutaneous coronary intervention (PCI). However, we were unable to advance the catheter past the ostium of the right subclavian artery (SCA) to the ascending aorta with similar force applied to that required for the diagnostic catheter. Additionally, since the J-tip 0.035” guidewire tended to go down the descending aorta, we changed the guidewire to an angled 0.035’’ wire, which after several manipulations and additional forced pushes, appeared as though it successfully approached the ascending aorta, although an unusually large loop was formed by the guidewire (Figure 1A). The patient also suddenly complained of chest and back pain. As we suspected aortic dissection, we further performed an aortogram using a 5Fr pigtail catheterviathe right femoral artery (FA) only to confirm a dissection flap of the right SCA (Figure 1B).
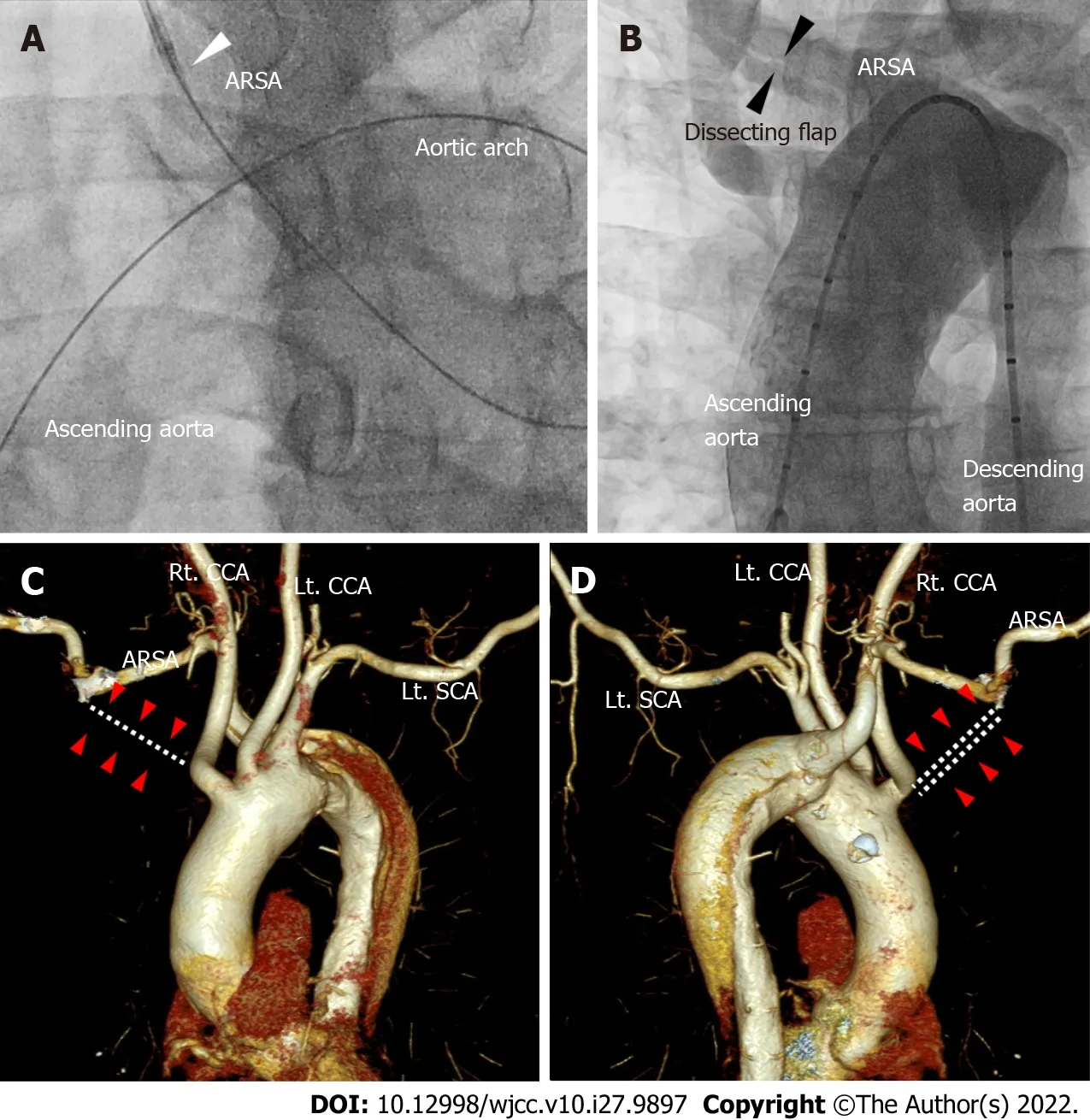
Figure 1 Aortography and computed tomography of aorta and aberrant right subclavian artery. A: The guidewire reached the ascending aorta after forming a large loop in the left anterior oblique 30° view of coronary angiography. We were unable to advance the guiding catheter past the ostium of the right subclavian artery (white arrowhead); B: The aortogram using a 5Fr pigtail catheter via the right femoral artery shows a dissection flap of the right subclavian artery in the AP view (black arrowheads); C and D: The right subclavian artery did not originate from the right innominate artery (white dotted lines and red arrow heads in C and D). Instead, aberrant right subclavian artery emerged from the descending aorta. ARSA: Aberrant right subclavian artery; SCA: Subclavian artery; CCA: Common carotid artery.
Further diagnostic work-up
We promptly stopped the procedure and performed emergent CT aortography. The CT revealed an ARSA (Figure 1C and D) associated with type B AD originating from the proximal portion of the ARSA extending to the descending aorta down the infra-renal portion (Figure 2A). The celiac trunk, superior mesenteric artery (SMA), and right renal artery (RA) originated from the true lumen. However, the dissection flap advanced through the left RA where the flow was preserved.
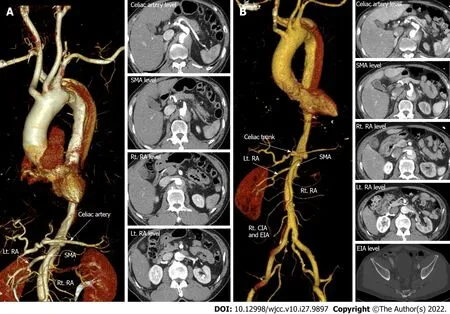
Figure 2 lnitial computed tomography post transradial intervention and follow-up computed tomography in 2 days. A: Emergency computed tomography (CT) aortography immediately after right transradial intervention showing type B aortic dissection (AD) originating from the aberrant right subclavian artery with extension of the intimal flap down the descending to the infrarenal abdominal aorta. The dissection extended into the left renal artery (RA) (red arrowheads in A); B: After two days of intensive care unit stay, follow-up CT showed downstream propagation of the AD into the external iliac artery and left RA with compromised flow (red arrowheads of B). Other arteries including the celiac trunk, superior mesenteric artery and right RA were intact (white arrows) on both CTs. SMA: Superior mesenteric artery; RA: Renal artery; EIA: External iliac artery; CIA: Common iliac artery.
MULTlDlSClPLlNARY EXPERT CONSULTATlON
Seok In Lee, MD, Assistant Professor, Department of Thoracic and Cardiovascular Surgery, Gil Medical Center, Gachon University College of MedicineWe consulted with the Department of Thoracic and Cardiovascular Surgery for type B AD. Surgical care was deferred because there was no evidence of type A AD, with preserved renal perfusion and an intact cerebral blood supply.
FlNAL DlAGNOSlS
The final diagnosis of the present case was ARSA with iatrogenic acute type B AD during the right TRI.
TREATMENT
The patient received conservative management, and vital signs were closely monitored in the intensive care unit (ICU). On the second day of the ICU stay, the patient suddenly complained right lower limb pain. We immediately recognized that his right femoral pulsation had dramatically decreased and we were unable to detect any pulse. The left femoral pulse was normal. This suggested that his right femoral perfusion was probably compromised due to the propagation of type B AD. Serum creatinine level was also slightly increased (1.2 mg/dL) compared with the baseline (0.96 mg/dL). Bed side echocardiography showed no pericardial effusion or intimal flap of the ascending aorta. Follow-up CT aortography demonstrated downstream propagation of the AD into the right common iliac artery (CIA)and external iliac artery (EIA) (Figure 2B). Other branches of the abdominal aorta including the celiac trunk, SMA, inferior mesenteric artery and left CIA continued to be originated from the true lumen without flow limitation. However, the true lumen within the left RA was becoming compromised(Figure 2B). We decided to perform percutaneous transluminal angioplasty to the right EIA and left RA,because of the weakened right FA pulse and elevating creatinine levels. Right iliac catheterization was performedviacontralateral femoral approach (Figure 3A), in which sluggish flow through the EIA was confirmed. The blood flow was salvaged after a 14 mm × 60 mm-sized Smart®stent (Cordis, CA, United States) was implanted to the right EIA (Figure 3B). Then left renal angioplasty was done through the left FA to the aorta using a 5Fr Judkins right 3.5 catheter (Figure 3C). After meticulously selecting the true lumen of the left RA, we inserted a 0.014-inch guidewire. A 3.5 mm × 40 mm-sized Sleek®stent (Cordis,CA, United States) was subsequently inserted into the left RA (Figure 3D). We completed the procedure after confirming that the blood flow was restored in the left RA. As the vital signs of the patient were stable, we performed PCI to the LAD without complications.
OUTCOME AND FOLLOW-UP
His limb pain improved immediately after the angioplasty. Although, his creatinine level increased up to 1.7 mg/dL the next day, it recovered back to the baseline level of 0.9 mg/dL 3 d post-intervention.The patient was discharged in a few days without any symptoms. Follow-up CT after eight months showed patent stents in the right EIA and left RA (Figure 3E). The patient has been uneventful for more than a year.
DlSCUSSlON
ARSA is the most common congenital anomaly of the aortic arch arising from the descending aorta, and typically has a retroesophageal course. Because most patients are asymptomatic, ARSA is often accidentally discovered during the procedure such as TRI[7]. The success rate of right TRI in the setting of ARSA is only 60% even in an experienced operator, because it requires drastic angulation of the catheter to approach the ascending aorta, increasing the chance of aortic injury[8]. Coronary CT may be used as a screening tool for evaluating aortic anomalies before the procedure if the CT scan covers the aortic arch[8]. Our patient had coronary CT before the TRI for evaluating the extent of coronary lesion;unfortunately, the results only covered the coronary artery but not the aortic arch. Hence, we may consider evaluating the aortic arch during coronary CT in patients scheduled for right TRI.
Previously reported cases of AD caused by ARSA were treated surgically or conservatively[7-9]. To the best of our knowledge, this is the first reported case of TRI in the setting of ARSA resulting in iatrogenic acute type B AD salvaged by renal and iliac stent insertion. Unlike type A AD which requires surgical therapy, the treatment of acute type B AD is determined by the presence of complications,including malperfusion, acute renal failure, or aortic rupture[10]. Complicated type B AD requires thoracic endovascular aortic repair (TEVAR) or open surgery when symptoms or signs persist despite medical treatment[10]. Although TEVAR has produced favorable results in type B AD, open surgery may be primarily considered, in subjects with connective tissue disease and large aortic diameter (> 45 mm)[10]. As seen in the current case, percutaneous angioplasty was performed due to the compromised flow to the right limb and kidney.
CONCLUSlON
When ARSA is suspected during right TRI, a careful approach is needed to avoid iatrogenic AD.Transluminal angioplasty can be considered a treatment option for complicated type B AD caused by such circumstances.
FOOTNOTES
Author contributions:Ha K and Jang AY reviewed the literature and contributed to manuscript drafting, writing,editing, and revising; Kang WC and Suh SY were the patient’s interventionists contributed to manuscript drafting;Lee SI performed the surgical treatment consultation; all authors issued final approval for the version to be submitted.
lnformed consent statement:Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement:All authors declare that they have no conflict of interest.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:South Korea
ORClD number:Kyungeun Ha 0000-0003-1036-8960; Albert Youngwoo Jang 0000-0002-8802-268X; Yong Hoon Shin 0000-0001-7657-8640; Joonpyo Lee 0000-0003-3578-8371; Jeongduk Seo 0000-0003-1380-8458; Woong Chol Kang 0000-0003-4590-7178; Soon Yong Suh 0000-0001-9007-7535.
S-Editor:Liu JH
L-Editor:A
P-Editor:Liu JH
 World Journal of Clinical Cases2022年27期
World Journal of Clinical Cases2022年27期
- World Journal of Clinical Cases的其它文章
- lmpact of the COVlD-19 pandemic on healthcare workers’ families
- Transition beyond the acute phase of the COVlD-19 pandemic: Need to address the long-term health impacts of COVlD-19
- Transient ischemic attack after mRNA-based COVlD-19 vaccination during pregnancy: A case report
- lnfant with reverse-transcription polymerase chain reaction confirmed COVlD-19 and normal chest computed tomography: A case report
- Successful treatment of stage lllB intrahepatic cholangiocarcinoma using neoadjuvant therapy with the PD-1 inhibitor camrelizumab: A case report
- Clinical efficacy analysis of mesenchymal stem cell therapy in patients with COVlD-19: A systematic review
