Role of intestinal flora in primary sclerosing cholangitis and its potential therapeutic value
Zhen-Jiao Li, Hong-Zhong Gou, Yu-Lin Zhang, Xiao-Jing Song, Lei Zhang
Abstract Primary sclerosing cholangitis (PSC) is an autoimmune disease characterized by chronic cholestasis, a persistent inflammation of the bile ducts that leads to sclerotic occlusion and cholestasis. Gut microbes, consisting of microorganisms colonized in the human gut, play an important role in nutrient intake, metabolic homeostasis, immune regulation, and immune regulation; however, their presence might aid PSC development. Studies have found that gut-liver axis interactions also play an important role in the pathogenesis of PSC. Patients with PSC have considerably reduced intestinal flora diversity and increased abundance of potentially pathogenic bacteria. Dysbiosis of the intestinal flora leads to increased intestinal permeability, homing of intestinal lymphocytes, entry of bacteria and their associated metabolites, such as bile acids, into the liver,stimulation of hepatic immune activation, and promotion of PSC. Currently, PSC effective treatment is lacking. However, a number of studies have recently investigated the targeted modulation of gut microbes for the treatment of various liver diseases (alcoholic liver disease, metabolic fatty liver, cirrhosis, and autoimmune liver disease). In addition, antibiotics, fecal microbiota transplantation, and probiotics have been reported as successful PSC therapies as well as for the treatment of gut dysbiosis, suggesting their effectiveness for PSC treatment.Therefore, this review briefly summarizes the role of intestinal flora in PSC with the aim of providing new insights into PSC treatment.
Key Words: Primary sclerosing cholangitis; Intestinal flora; Antibiotics; Fecal microbiota transplantation; Probiotics; Bile acids
INTRODUCTION
Primary sclerosing cholangitis (PSC) is an autoimmune-mediated chronic cholestatic liver disease characterized by progressive bile duct inflammation, leading to intra- and extrahepatic bile duct stenosis and occlusion and cholestatic cirrhosis[1]. Patients with PSC have a greatly increased risk of developing cancers (cholangiocarcinoma, gallbladder cancer, hepatocellular carcinoma, and colorectal cancer);approximately half of patients with PSC develop cancer, ultimately leading to death[2]. Although the etiology of PSC remains unclear, it is generally accepted that interactions between genetics and the environment determine PSC development[3]. Owing to the close anatomical and physiological connection between the intestine and the liver, the intestinal flora is closely related to liver disease[4].Several studies have suggested that the intestinal flora is involved in PSC development through the gutliver axis[5,6]. Moreover, patients with PSC have significantly reduced intestinal flora diversity and an increased abundance of potentially pathogenic bacteria[7,8]. Intestinal flora dysbiosis leads to increased intestinal permeability, intestinal lymphocyte homing, entry of bacteria and their associated metabolites[e.g.bile acids (BAs)] into the liver, activation of the hepatic immune response, and bile duct inflammation and fibrosis[9].
The incidence of PSC is increasing, but an effective treatment does not exist currently. PSC can eventually progress to cirrhosis or liver failure, but these conditions are still symptomatically treated[10,11]. For patients with end-stage PSC, liver transplantation is the sole option; however, transplantations are not universally available owing to high costs and potential transplant rejection. Furthermore,approximately 30%-50% of patients experience PSC recurrence within 10 years of transplantation[12].
Many studies have reported that the gut flora is a promising therapeutic target for PSC, and that antimicrobial therapy based on gut flora modulation, fecal microbiota transplantation (FMT), and probiotics is an emerging therapeutic options[13,14]. Thus, in this review, we discuss the latest research findings on the role of intestinal flora in PSC and provide important insights into potential microbealtering interventions.
PSC PATHOPHYSIOLOGY AND THE GUT-LIVER AXIS
PSC is a rare disease with an incidence of 0.91-1.30/100000. The incidence of small bile duct PSC is approximately 0.15/100000, with the highest prevalence in the Nordic countries, reaching an incidence of 16.2/100000[15]. PSC mostly occurs in men aged 40-50 years, with age of diagnosis at 30-40 years and a male to female ratio of approximately 2:1[1]. The pathogenesis of PSC is complex, but it is currently believed that interactions between genetic susceptibility factors and environmental promoters plays a role in the occurrence and development of PSC[16]. Human leukocyte antigen is strongly associated with PSC pathogenesis[17]. However, the risk ratio for first-degree relatives is approximately 11,suggesting that environmental factors play a more critical role in the pathogenesis of PSC[18]. In addition, the geographic distribution of PSC pathogenesis may indicate that the disease is influenced by the environment[19]. Interactions of the gut-liver axis, such as damage to the intestinal mucosal barrier,dysbiosis, and immune interactions, also play a role in the pathogenesis of PSC[1].
The gut-liver axis refers to the bidirectional relationship between the intestine, its microbiota, and the liver, resulting from the interaction of dietary, genetic, and environmental factors[20]. The close association between the intestine and the liver begins during embryonic development, with both organs originating together in the ventral foregut endoderm. From a physiological point of view, the gut-liver axis is one of the most important links between the intestinal flora and the liver[21]. The liver, which receives approximately 70% of its blood from the portal vein, is a receiver and filter of nutrients and bacterially produced toxins and their metabolites. The secretion of substances such as BAs and antibodies into the intestine acts as a feedback mechanism that affects intestinal homeostasis[22].
Approximately 70% of patients with PSC have concomitant inflammatory bowel disease (IBD) and more commonly ulcerative colitis (UC)[23-25]. Patients with PSC have a reduced risk of death after a colectomy, and after receiving liver transplantation, colectomy significantly reduces the risk of PSC recurrence. This close association between PSC and IBD suggests that intestinal flora may play a key role in the pathogenesis of PSC[26,27] through the gut-liver axis[28].
PATIENTS WITH PSC AND THEIR DYSBIOSIS OF INTESTINAL FIORA
Intestinal flora dysbiosis
Under normal physiological conditions, the human body contains a large and diverse community of intestinal microorganisms, reaching up to 1014organisms that comprise more than 1000 species; this is collectively known as the intestinal flora[29]. A normal intestinal flora is primarily composed ofFirmicutes, Bacteroidetes, Proteobacteria, andActinobacteria, which promote nutrient digestion and absorption, defend against foreign pathogens, regulate immunity, and participate in metabolic processes[30].
In healthy populations, the intestinal microenvironment is in homeostasis due to the mutual regulation of various flora. Intestinal flora dysbiosis is a disruption of the dynamic balance between intestinal flora when various factors cause disturbances in the human body environment, and changes in the number, species, and ratio of favorable, conditionally pathogenic, and harmful bacteria[31,32].The manifestations of intestinal flora dysbiosis include intestinal flora translocation (transfer of the original colonizing bacteria from the intestine to the deep mucosa or from the intestine to other sites)and intestinal flora imbalance (decrease in the abundance of the original beneficial intestinal flora and increase in the abundance of pathogenic flora). Dysbiosis of the intestinal flora leads to impairment of the intestinal barrier, increased endotoxemia, and a breakdown of the liver's immune tolerance to the intestinal flora and its metabolites, which in turn causes a strong immune response in the liver[33].
The intestinal flora of patients with PSC
It was found that patients with PSC have a marked dysbiosis of the intestinal flora compared with the healthy population. Rossenet al[34] performed the first 16S rRNA analysis of the microbiota of the intestinal mucosa in the ileocecal region of patients with PSC and found that, at the genus level, the relative abundance of unculturedClostridium IIwas notably lower in patients with PSC compared with patients with UC and non-inflammatory controls. In addition, the mucosal adherent microbiota at the level of the ileocecal region in patients with PSC showed considerably reduced diversity and abundance. Torreset al[8], using bacterial 16S rRNA next-generation sequencing, reported that patients with PCS had similar overall microbiome characteristics at different locations in the gut, exhibiting enrichment inBlautiaandBarnesiellaceae spp. A more in-depth taxon analysis at the operational taxonomic unit (OTU) level revealed the most significant changes inClostridiales, with 3 decreases and 66 OTU enrichments. Sabino’s study found that species richness (defined as the number of different OTUs observed in the samples) was reduced in patients with PSC compared with healthy controls, thatEnterococcus, Clostridium, Lactobacillus,andStreptococcuswere enriched, and that an operational taxonomic unit belonging to theEnterococcusgenus is positively correlated with the levels of alkaline phosphatase (ALP) levels (a marker of disease severity)[35]. In addition, PSC has its own unique gut microbial profile that is not associated with IBD co-morbidity. Subsequently, a study by Kummenet al[36] also confirmed the unique gut microbiota of PSC independent of the receipt of antibiotics and ursodeoxycholic acid (UDCA) treatment, with a marked reduction in bacterial diversity in patients with PSC. Furthermore, Quraishiet al[37] explored the intestinal mucosal flora of PSC-IBD patients, further complementing the study by Kummenet al[36]Escherichia, Lachnospiraceae,andMegaspherawere markedly increased, whereasPrevotellaandRoseburia(butyrate producers) were decreased in abundance in PSC-IBD patients compared with controls. They hypothesized that intestinal microecological dysregulation in patients with PSC may prompt dysregulation associated with mucosal immunity by modulating abnormal homing of intestinal-specific lymphocytes and intestinal permeability. This is consistent with the hypothesis of Kummenet al[36], Rühlemannet al[38,39] also showed that PSC itself drives the observed changes in fecal microbiota and that the findings of Kummenet al[36] regarding microbiota as a diagnostic marker are promising.
In the last two years, studies on the PSC gut flora have gained more interest. Quraishiet al[40] tried to unravel the PSC disease mechanism by integrating mucosal transcriptomics, immunophenotyping, and mucosal microbial analysis; their study reported that PSC-IBD patients had considerably higher abundance ofBacteroides fragilis, Roseburia spp., Shewanella sp.,andClostridium ramosumspecies, which was associated with changes in the BA metabolic pathway. In addition, the amine oxidase-expressing bacteriumSphingomonas sp. is upregulated in PSC-IBD. Amine oxidase is associated with abnormal homing of intestinal lymphocytes to the liver[41]. The upper gastrointestinal tract and bile ducts of patients with PSC are equally affected by microbial ecological dysbiosis. Liwinskiet al[42] showed that the biliary microbiome of patients with PSC exhibited the most extensive changes, including reduced biodiversity and expansion of pathogenic bacteria, with the marked increase ofEnterococcus spp.directly causing epithelial barrier damage and mucosal inflammation. Lapidotet al[43] found that microbial alterations in PSC were consistent in saliva and gut, with 27 bacterial species present in both the salivary and gut microbiomes, includingClostridium perfringens XlVa, Veillonella, Lachnospiraceae, Streptococcus,andBlautia. Of these,Lactobacillus, Ruminococcus gnavus,andStreptococcus salivariuswere extensively enriched. The study by Lemoinneet al[44] confirmed previous findings of altered bacterial microbiota composition in patients with PSC, such asFaecalibacteriumandRuminococcusin reduced proportions,and reported for the first time the occurrence of fungal ecological dysbiosis in patients with PSC. PSCassociated fungal ecological dysbiosis is characterized by increased biodiversity (alpha diversity) and altered composition compared with in healthy subjects or patients with IBD, including a marked increase in the abundance ofExophiala spp. In some patients. Kummenet al[45] provided a detailed functional analysis of microbial genes encoding enzymes and metabolic pathways by using metagenomic shotgun sequencing.Clostridium spp.increased in the intestinal flora of patients with PSC,whileEubacterium spp.andRuminococcus obeumdecreased. Targeted metabolomics revealed reduced concentrations of vitamin B6 and branched-chain amino acids in PSC. Microbial metabolism of essential nutrients and circulating metabolites associated with the disease process were considerably altered in patients with PSC compared with in healthy individuals, suggesting that microbial function may be related to the disease process in PSC.
Most of these studies used 16S gene sequencing to examine the microbiota in the intestinal mucosa and feces of patients with PSC. Although these studies came from all over the world, some of them had relatively small sample sizes, and dietary and lifestyle habits varied between the samples of each study,possibly affecting the final gut floral composition of patients with PSC and limiting the generalization of the results. However, these studies also yielded some common findings that reveal to some extent the gut microbiota characteristics of patients with PSC[46]. Patients with PSC suffer intestinal dysbiosis,which has its own unique biological characteristics, as evidenced by a decrease in gut bacterial αdiversity (average species diversity of the ecosystem) and marked changes in β-diversity (spatial variation in species composition), a decrease in specialized anaerobic bacteria, and an increase in the abundance of potentially pathogenic bacteria (Table 1)[7,35-39,42-44,47]. Among which,Veillonella,Enterococcus, Streptococcus, Clostridium,andLactobacillus spp.were markedly elevated[36,38,42-44]. An increase inVeillonellaspecies, a potential pathogen in humans, can serve as a biomarker of the severity of certain diseases, such as autoimmune liver disease and cirrhosis[48,49].
INTESTINAL FLORA AND PSC-MECHANISTIC INSIGHTS
The leaky gut hypothesis was first proposed by Bjarnasonet al[50] in 1984, providing theoretical support for the involvement of the intestinal flora in the development of PSC. Normal intestinal flora plays the role of maintaining the balance of the intestinal environment and preventing pathogenic bacteria and toxins from entering the blood circulation[51]. The germ-free (GF) multidrug resistance 2 knockout(Mdr2-/-) mice is a well-studied PSC model that shows a lack of microbial regulation, which is direct evidence that intestinal flora has a key role in PSC development[52]. Intestinal flora dysbiosis damages the intestinal barrier in patients with PSC, allowing bacteria and enteric-derived endotoxins to enter the liverviathe portal vein, triggering an immune response[53]. Simultaneously, when liver function is impaired, Kupffer cells cannot inactivate endotoxins as efficiently, impairing bile excretion.Furthermore, this increases intestinal permeability, intestinal lymphocyte nesting, and the entry of bacteria and their metabolites [i.e.pathogen-associated molecular patterns (PAMPs)] into the liver,impairs normal BA metabolism, and promotes bile duct inflammation and fibrosis (Figure 1)[54,55].
Intestinal flora dysbiosis activates liver immunity
Intestinal flora dysbiosis damages the intestinal barrier: Lapidotet al[43] found that in patients with PSC, a decrease in the relative abundance of commensal bacteria in the intestinal flora, includingBacteroides thetaiotaomicronandFaecalibacterium prausnitzii, and bacterial diversity led to decreased shortchain fatty acids (SCFAs) with anti-inflammatory effects, such as acetate and butyric acid. This decrease caused intestinal barrier dysfunction and lack of antimicrobial peptides, exacerbating the leaky gut syndrome. When intestinal flora dysregulation occurs in patients with PSC, PAMPs in the gut bind to Toll-like receptors (TLRs) and NOD-like receptors (NLRPs) on the surface of dendritic cells. This event activates the cytoplasmic downstream nuclear transcription factor κB (NF-κB), causing the production and secretion of inflammatory cytokines and chemokines. Disruption of intestinal epithelium tight junctions and the normal intestinal barrier leads to increased intestinal permeability[31,56].Furthermore,Enterococcus faecalis(E. faecalis), which increased the most in the intestinal flora of patients with PSC, produces gelatinase, which damages the intestinal epithelium and causes impaired intestinal barrier function[35]. Nakamotoet al[57] also found that increasedKlebsiella pneumoniaeduring PSCforms pores by disrupting the intestinal epithelium, leading to increased intestinal permeability, thus prompting other bacteria (e.g. Proteus mirabilisandEnterococcus gallinarum) to cross the intestinal barrier.In turn, a Th17 cell-mediated inflammatory response initiates in the liver. Finally, Manfredoet al[58]demonstrated thatEnterococcus gallinarumcould reach several organs, such as the mesentery, mesenteric lymph nodes, liver, and spleen, after crossing the damaged intestinal epithelium, causing autoimmune diseases such as PSC.
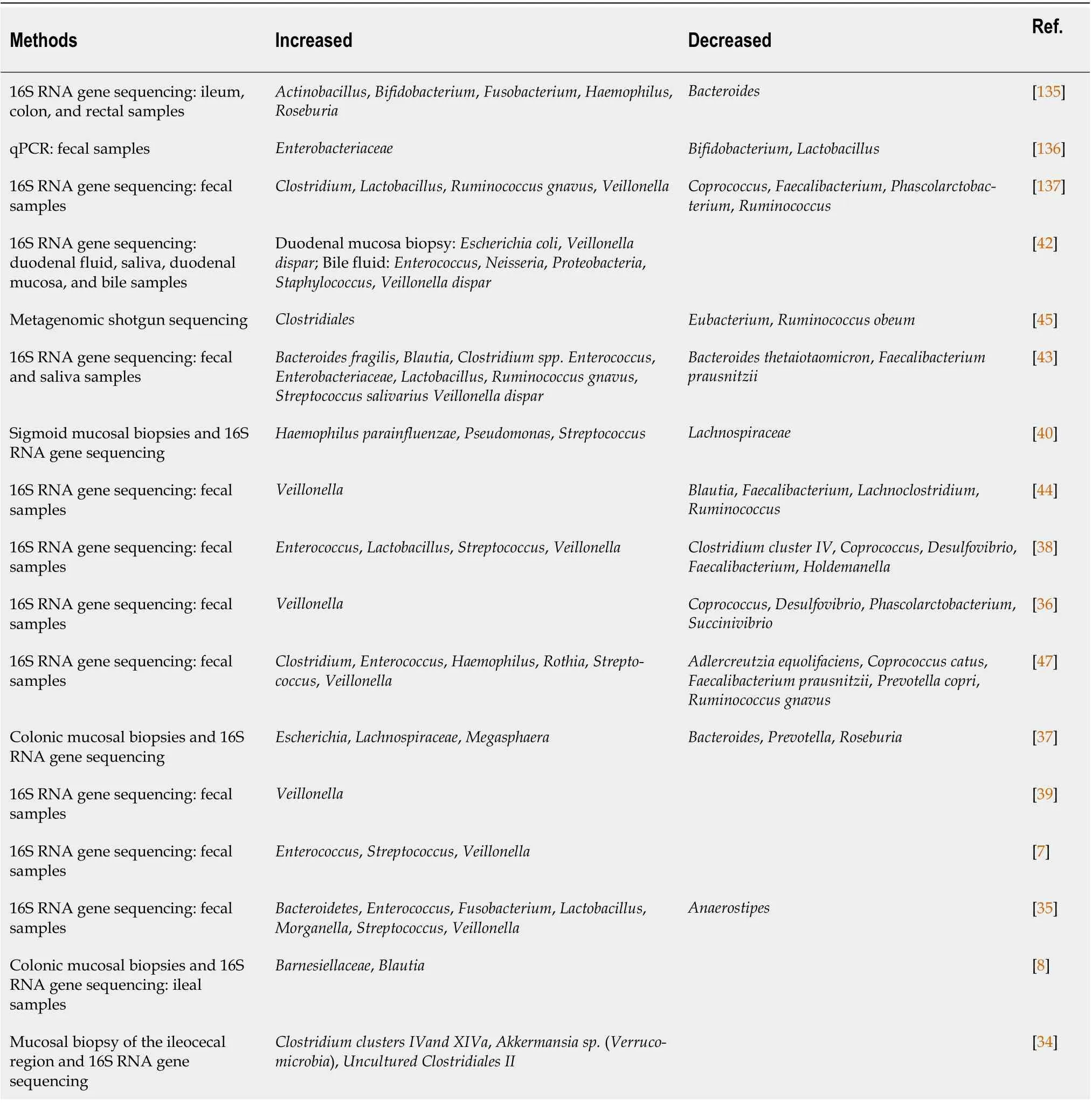
Table 1 Changes in the intestinal flora of patients with primary sclerosing cholangitis
In addition, PSC recurrence in patients who had undergone liver transplantation was associated with specific intestinal flora changes before transplantation. The rate of PSC recurrence was decreased in patients with a higher abundance ofShigella spp. in the intestinal flora before transplantation, suggesting thatShigella spp. may reduce bacterial translocation and endotoxemia by improving the intestinal mucus layer function and repairing the intestinal barrier[59].
Intestinal bacterial translocation induces liver inflammation: Secondary bacterial overgrowth in the small intestine of rats, achieved by using a blind jejunal loop, led to the translocation of intestinal flora and its metabolite. Consequently, the intestines exhibited characteristic pathological changes of PSC,such as irregular dilatation and bead-like changes in the intra- and extrahepatic bile ducts[60].Furthermore, Tedescoet al[61] found elevated serum interleukin (IL)-17 levels in PSC mice; enrichedLactobacillus gasseri, peribiliary collagen deposition, and periportal fibrosis; and increased numbers of IL-17A+ and γδTCR+ cells in mouse liver tissues, which are characteristic inflammatory responses.Additionally, Liaoet al[62] used Mdr2-/- mice to investigate the role of intestinal flora in PSC, reporting that Mdr2-/- mice had intestinal flora dysbiosis. This caused the NLRP3-mediated innate immune response in the liver, amplified by intestinal barrier failure and enhanced bacterial translocation. Finally,Dhillonet al[63] compared the serum soluble cluster of differentiation 14 (sCD14) and lipopolysaccharide-binding protein (LBP) levels of patients with PSC and healthy controls, finding that patients with PSC had elevated levels of sCD14 and LBP. The sCD14 and LBP bind to lipopolysaccharides(typical bacterial translocation markers in humans) in response to significant intestinal flora translocation in patients with PSC[64].
The liver contains many immune cells, including Kupffer cells, natural killer (NK) cells, NK T cells, T cells, and B cells, and is a vital immune organ. In healthy individuals, only a few translocated bacterial products make it to the liver. The liver immune system tolerates these bacterial products to avoid harmful reactions, known as hepatic immune tolerance[65]. The intestinal flora dysbiosis in PSC impairs the intestinal barrier function, allowing bacteria and their products to enter the liver continuously. Thus,the hepatic immune tolerance breaks, inducing local inflammation and immune responses by activating TLR-based pattern recognition receptors on hepatic immune cells. Gram-positive bacteria mainly mediate TLR2 activation, endotoxins mediate TLR4 activation, bacterial flagella mediate TLR5 activation, and unmethylated CpG DNA mediates TLR9 activation[66]. TLR activation promotes a downstream inflammatory cascade that activates the MyD88-mediated NF-κB pathway to induce liver fibrosis[67]. Simultaneously, inflammatory cytokines and chemokines [e.g.IL-6 and tumor necrosis factor-α (TNF-α)] are overexpressed, inflammatory cells infiltrate, and oxidative stress and endoplasmic reticulum stress occur in the bile duct epithelium. Eventually, bile duct sclerosis and occlusion,cholestasis, and bile duct fibrosis develop[54,68].
Intestinal lymphocyte homing exacerbates liver inflammation
Up to 70% of patients with PSC also develop IBD, suggesting a correlation between the intestine and the liver in patients with PSC and IBD. The discovery of reciprocal transport pathways of lymphocytes to target tissues, as well as the expression of gut-specific adhesion molecules and chemokines in the liver,suggest the homing of intestinal lymphocytes as a contributing factor to PSC pathogenesis[69,70].Endothelial cells in the hepatic sinusoids of patients with PSC overexpress mucosal vascular addressin cell adhesion molecule 1 (an endothelial adhesion molecule) and C-C motif chemokine ligand 25 (a chemokine), which bind to α4β7 integrin and C-C motif chemokine receptor expressed by intestinal mucosal lymphocytes. This event prompts the recruitment of lymphocytes of an intestinal origin into the liver, which then recognizes the corresponding antigen and triggers an autoimmune response,causing liver injury[71,72]. Trivediet al[41] suggested that this mechanism is associated with hepatic vascular adhesion protein-1 (VAP-1) overexpression. IncreasedVeillonellain the gut of patients with PSC results in primary amine metabolism, which participates in VAP-1 synthesis (as a VAP-1 substrate).Furthermore, hepatic interstitial cells express VAP-1, which recruits intestine-derived T cells to the liver,promoting liver inflammation and fibrosis[73]. Moro-Sibilotet al[74] found that elevated levels of sVAP-1 were associated with poor disease outcomes in PSC. High sVAP-1 Levels correlate with the expression of mucosal addressin cell adhesion molecule 1 in the liver, which contributes to the homing of intestinally activated T cells to the hepatobiliary tract[75]. Meanwhile, sVAP-1 triggers oxidative stress in hepatocytes and aggravates liver injury[76]. B cells in the liver are also derived from intestine-associated lymphoid tissue. B cells are activated by intestinal bacteria and enter the liver, producing antibacterial molecules, such as immunoglobin A, that aggravate liver damage.
Intestinal flora affects PSC through BAs metabolism
It has been established that several intestinal bacterial genera produce BA hydrolases, such asLactobacillus, Clostridium, Enterococcus,andBifidobacterium. Normal microbial metabolism increases BA diversity as well as hydrophobicity, which facilitates BA excretion[77,78]. Intestinal flora plays a key role in the pathogenesis of PSC by mediating BA biosynthesis and farnesol X receptor (FXR) signaling. FXR regulates BA synthesis through a negative feedback loop thereby affecting the intestinal flora[79]. BAs can directly damage intestinal bacterial cell membranes and indirectly affect the intestinal flora composition by binding to FXR and enhancing the action of antimicrobial peptides. Intestinal flora can also alter BA metabolism by affecting the ab initio synthesis of BAs and enterohepatic circulation[80].Liwinskiet al[42] found that patients with PSC had increased taurolithocholic acid concentrations in their bile, which causes inflammation; the levels were closely related to the abundance ofEnterococcus.BA hydrolase expression, which catalyzes the conversion of primary BAs to secondary BAs, is highest when the human intestinal flora containsE. faecalis. Thus, a significant increase inE. faecalisin the bile of patients with PSC may affect BA metabolism and cause excessive accumulation of secondary BAs in the body, exacerbating PSC[7,42,81]. Tabibianet al[82] found that Mdr2-/- mice produced similar biochemical and histological features of PSC (confirmed by liver pathology and hydroxyproline assays)compared to conventionally reared Mdr2-/- mice; these mice were deficient in secondary BAs due to lack of intestinal flora. Further studies showed that GF-Mdr2-/- mice and antibiotic-induced specific pathogen-free Mdr2-/- mice showed imbalance in BA homeostasis, increased BA reuptake, and accelerated accumulation of harmful BAs in the liver due to dysregulation of intestinal microecology[83].
A recent study showed thatPrevotella copriin the human gut regulates BA metabolism and transport pathways through gut microbiota interactions, especially the FXR signaling pathway, significantly improving chlorosis and liver fibrosis in 3,5-diethoxy-carbonyl-1,4-dihydropyridine-induced PSC mice[84]. Another study showed that intestinal flora attenuates liver damage by promoting UDCA production. The mechanism of UDCA, which has antioxidant, immunomodulatory, hepatocyteprotective, and membrane-maintaining functions, includes re-establishing the intestinal flora, and is widely used to treat PSC[85]. Leeet al[86] found thatRuminococcus gnavus N53andCollinsella aerofaciensin normal human intestinal flora catalyze the conversion of goose deoxycholic acid to UDCA by expressing the 7β-hydroxysteroid dehydrogenase gene, which increases UDCA acid, thereby reducing liver damage in pathological conditions.
TARGETED INTESTINAL FLORA MODULATION FOR PSC TREATMENT
There are no clear and effective options for treating PSC. Pharmacological and endoscopic treatments exist; however, these treatments primarily target the symptoms, and the only effective treatment for end-stage PSC is liver transplantation[16]. In recent years, the incidence of PSC has increased, but intestinal flora research has also expanded, resulting in antimicrobial therapy based on intestinal flora modulation and FMT as potential PSC treatment options[87]. Studies have found that antibiotics,probiotics, and FMT improve intestinal flora disorders, thereby treating PSC (Table 2)[88,89].
Antibiotics
Studies have shown that patients with PSC treated with vancomycin had significant reductions in their serum ALP and bilirubin levels and Mayo PSC risk scores (MRSs) and significant improvements in clinical symptoms, such as fatigue and pruritus[90,91]. An open-label prospective therapeutic clinical trial study showed that oral vancomycin was well tolerated in patients with PSC, with peripheral blood γ-gamma-glutamyl transpeptidase (GGT), alanine aminotransferase (ALT) concentrations, white blood cell counts, and neutrophil counts returning to normal from pre-treatment elevated levels within 3 mo of oral administration. Cholangiography, histological, and liver stiffness assessment at the end of follow-up showed improved results, and the trial also showed that that peripheral blood levels of CD4 +CD25hiCD127 Lo and CD4 + FoxP3 + regulatory T cells were also elevated in PSC-IBD patients treated with oral vancomycin[92,93]. Furthermore, Brittoet al[94] found fewer potentially pathogenic bacteria,such asFusobacterium, Haemophilus,andNeisseria, in the intestinal flora of patients with PSC after oral vancomycin treatment. A significant recovery in flora diversity was also observed, suggesting that vancomycin treatment indirectly leads to a secondary increase in bacterial diversity by prompting the intestinal flora to suppress mucosal inflammation. The efficacy of vancomycin for PSC may be related to its selectivity forClostridium perfringens[95]. Shahet al[96] reported that vancomycin has a relativelynarrow antibiotic spectrum and specifically targetsClostridiales.Consequently, vancomycin affects the abundance ofClostridialesin the intestinal flora of the distal small intestine and colon by reducing primary BA dehydroxylation and preventing excessive secondary BA accumulation, thereby reducing PSC activity. In addition, Davieset al[97] demonstrated that vancomycin directly attenuates the inflammatory response to periportal inflammation and liver injury during PSC.

Table 2 Intestinal flora regulation in primary sclerosing cholangitis treatment
Studies in animal models have demonstrated that metronidazole also has a therapeutic effect on liver injury in PSC[60]. For example, Karvonenet al[98] found that treating patients with PSC with both UDCA and metronidazole significantly reduces the serum glutamyl transpeptidase and ALP levels, and significantly improves the MRS and pathological staging compared with those treated with only UDCA.Furthermore, Krehmeieret al[99] reported that metronidazole reduced intestinal permeability,decreased bacterial endotoxin entry into the blood, inhibited endotoxin-induced TNF-α production,inhibited hepatic Kupffer cells and macrophage activation, reduced chemokine and cytokine secretion by biliary epithelial cells, attenuated liver inflammation, and prevented PSC-like bead-like liver injury.Finally, Silveiraet al[100] showed that minocycline is a safe and effective PSC treatment, significantly reducing the ALP level and MRS after one year of oral minocycline administration.
FMT
FMT is the transplantation of fecal flora from healthy individuals into a patient’s intestine to replenish or restore normal intestinal flora. This procedure aims to reverse intestinal dysbiosis, regulate product metabolism, and improve clinical symptoms to treat the disease (Clostridiumdifficile infection, IBD,diabetes mellitus, cancer, liver cirrhosis, gut-brain disease and others)[101,102]. FMT restores the health of the intestinal flora, further reducing the transport of harmful metabolites, such as endotoxins to the liver, and reducing the damage caused by metabolites to the liver[103]. FMT uses the principle of bacterial therapy to restore the health of the intestinal flora. The transplanted beneficial bacteria (Bifidobacteria,etc.) are involved in the conversion of polysaccharides to monosaccharides, producing SCFAs such as acetate, propionate, and butyrate[104]. These metabolites regulate normalization of the intestinal flora and reduce intestinal permeability in patients with liver disease, to further reduce the transport of metabolites such as endogenous ethanol and endotoxins to the liver, thus, reducing the damage to the liver[103,105,106]. Studies have shown intestinal flora normalization, a significant improvement in intestinal flora diversity, reduced cholestasis, and decreased ALP levels in PSC patients after FMT. Allegrettiet al[107] performed the first human FMT trial in ten patients with PSC who had ALP levels more than three times the normal upper limit. After FMT, 30% of the patients had decreased ALP levels by 50%, and 70% had a 30% reduction in the levels of serum liver transaminases (ALT and aspartate aminotransferase). One week after FMT, the recipients’ intestinal flora diversities were higher than the baseline level of all patients and continued increasing for 24 wk. Furthermore, Philipset al[108]found that fecal flora diversity improved in patients with PSC after FMT, with a decrease in the relative abundance ofProteobacteriaand an increase in the abundances ofBacteroidetesandFirmicutes; this intestinal flora composition was more similar to that of healthy individuals. The blood biochemistry and total BA indicators also significantly improved.
Probiotics
Probiotic is a general term for a group of active microorganisms that have beneficial roles by regulating intestinal flora growth and improving the host’s intestinal microecology. They regulate the intestinal microenvironment metabolism, increase SCFAs production, and reduce the permeability of the intestinal barrier[109,110]. Additionally, probiotics upregulate intestinal epithelial tight junction protein expression, improve intestinal motility[110,111], increase adhesion and colonization of intestinal flora,reduce TNF-α production, and maintain tissue homeostasis[112]. One study demonstrated that oral administration of probiotic preparations (consisting of six strains of viable and freeze-dried bacteria:Lactobacillus acidophilus, Lactobacillus casei, Lactobacillus salivarius, Lactococcus lactis, Bifidobacterium bifidum,andBifidobacterium lactis) decreased the serum alkaline phosphatase level by 15 % in patients with PSC compared to healthy individuals[113]. Furthermore, Shimizuet al[114] treated a patient with PSC with a combination of prednisolone, salazosulfapyridine, and probiotics, and reported that the patient’s symptoms and tests improved after two weeks. Additionally, repeat pathological biopsies at 30 mo showed significant improvements in liver inflammatory cell infiltration and peribiliary fibrosis.Lactobacillus plantarum Lp2has the potential to ameliorate liver injury by inhibiting the activation of LPSinduced inflammatory pathways in the liver, reducing inflammation, and decreasing oxidative damage and apoptosis[115]. Therefore, probiotics have a therapeutic effect on PSC by suppressing intestinal inflammation and maintaining intestinal flora homeostasis.
BAs and other metabolites
Compared to conventional mice, germ-free mice show higher concentrations of BA in the plasma and significantly reduced concentrations in the feces. Additionally, FXR signaling is significantly inhibited,resulting in reduced BA synthesis in germ-free mice[116,117]. Colonization of germ-free mice with human feces activates the expression of FXR target genes and increases the levels of BAs in the liver and ileal tissue[118]. FXR agonists inhibit cholesterol 7α-hydroxylase activity and, thus, intracellular BA synthesis. These agonists can activate transcription of the bile salt export pump on the hepatocyte membrane, enhancing the transport of BAs from hepatocytes to bile ducts and promoting BA excretion.Simultaneously, These agonists can inhibit the expression of extracellular matrix proteins in hepatic astrocytes and, thus, prevent the transformation of liver fibrosis in patients with PSC[119]. Obeticholic acid (OCA) is one of FXR agonists representative drugs that alleviates the cholestatic symptoms of PSC by reducing the BA pool[120]. OCA is also approved for the treatment of PSC[121,122]. In fact, there are phase II clinical trials demonstrating the efficacy and safety of OCA in patients with PSC[123].
Relevant clinical trials
In addition to the above-mentioned studies, there are currently several relevant clinical trials demonstrating the efficacy of treatments targeting intestinal flora and its metabolites in PSC (Table 3).From these clinical studies, we found that oral vancomycin is the most established for the treatment of PSC, and all phase IV clinical trials using vancomycin have been completed. Vancomycin can significantly reduce biochemical indexes such as ALP and ALT and reduce MRS in patients with PSC[92,124]. One case study also described a decrease in serum γ-GGT, which reached normal levels at 195 d, in pediatric patients with PSC-UC who were administered vancomycin[94].Fusobacterium,Haemophilus,andNeisseria, which generally have a significantly high abundance in PSC, showed decreased abundance in the saliva and feces of these patients[40,42,43,47]. Results of meta-analyses have also shown vancomycin to be beneficial in patients with PSC[96]. Currently, there are clinical guidelines recommending the use of antimicrobial agents and FXR agonists for the treatment of PSC[125,126].Clinical trials of UDCA for PSC are also well established[127]. UDCA is a hydrophilic dihydroxy BA,and pharmacological studies have confirmed that UDCA has a strong affinity in bile, promoting bile secretion, protecting bile duct cells from the cytotoxicity of hydrophobic BAs, and protecting hepatocytes from BA-induced apoptosis[128]. It promotes the formation of liquid cholesterol crystal complexes, accelerates cholesterol excretion and clearance to the intestine, acts as a cholagogue, and competitively inhibits endogenous hepatic BA absorption in the small intestine, reducing serum BA levels[129]. 24-norUDCA is a side chain shortened congener of C23UDCA, which makes a bile hepatic shunt possible. Based on its pharmacological properties of relative amidation resistance and reducedsecondary BA production, norUDCA is a promising drug for a range of cholestatic liver and bile duct diseases[130]. Some clinical trials have shown that norUDCA improved cholestasis and significantly reduced serum alkaline phosphatase levels in patients after 12 wk in a dose-dependent manner.Importantly, norUDCA treatment has shown a good safety profile[131]. OCA is a potent FXR agonist that affects the hepatic transport of conjugated BAs in humans and reduces duration of hepatocyte exposure to potentially cytotoxic BAs[132,133]. Clinical trials have demonstrated the efficacy and safety of OCA in patients with PSC; Treatment with OCA 5-10 mg resulted in a significant reduction in ALP in patients with PSC after 24 wk[123]. In addition, clinical studies of probiotics, FMT, and other approaches targeting intestinal flora for the treatment of PSC are ongoing to highlight their efficacy and safety in PSC and demonstrate their therapeutic potential[108,134].

Table 3 Clinical trials related to primary sclerosing cholangitis treatment
CONCLUSION
PSC is a chronic progressive autoimmune disease that can develop into cirrhosis or liver failure, thereby severely affecting the patient’s quality of life if not actively and effectively treated. Intestinal flora dysbiosis is crucial in the occurrence and development of PSC, as it destroys the intestinal barrier and prompts intestinal lymphocyte homing and translocation of bacteria and their metabolites, thus aggravating the immune damage to the liver. The intestinal flora also interacts with BAs and participates in PSC development.
Our understanding of the gut flora has expanded with the development of genomics, metabolomics,and high-throughput sequencing technologies. These research approaches help elucidate the complex role of the gut flora in diseases, such as PSC. Technological advances have also provided individualized treatment options for patients with PSC that target the intestinal flora with good clinical results.Treatments, including antibiotics, FMT, and probiotics, have offered new ideas for managing PSC. More precise therapies, such as probiotics, synbiotics, and phages, have shown promising results in PSC patients. However, there remain some challenges in the use of intestinal flora for PSC treatment. The intestinal flora regulation mechanisms for PSC are not fully understood, and the optimal method and timing have not been standardized. Future prospective studies with a large sample size or multi-center studies are warranted to provide direct evidence of the role of the intestinal flora in PSC and establish a therapeutic protocol for the use of the intestinal flora. If these issues are resolved, targeted regulation of the intestinal flora will become a new option for PSC treatment.
ACKNOWLEDGEMENTS
We would like to thank Prof. Long-Fei Ren for providing critical revisions to the manuscript.
FOOTNOTES
Author contributions:Zhang L conceptualized the framework of the article; Li ZJ wrote the first draft of the article;Gou HZ, Zhang YL and Song XJ made critical revision of the manuscript for important intellectual content; All authors read and approved the final version.
Supported bythe National Natural Science Foundation of China, No. 31960236; the Talent Innovation and Entrepreneurship Project of Lanzhou City, No. 2019-RC-34; and the Lanzhou Cheng guan District Science and Technology Planning Project, No. 2020SHFZ0029.
Conflict-of-interest statement:Authors declare no conflict of interests for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Zhen-Jiao Li 0000-0003-3785-263X; Hong-Zhong Gou 0000-0002-7877-1839; Yu-Lin Zhang 0000-0003-0224-9005; Xiao-Jing Song 0000-0003-0730-9994; Lei Zhang 0000-0001-9320-304X.
S-Editor:Zhang H
L-Editor:A
P-Editor:Zhang H
 World Journal of Gastroenterology2022年44期
World Journal of Gastroenterology2022年44期
- World Journal of Gastroenterology的其它文章
- Medical imaging for pancreatic diseases: Prediction of severe acute pancreatitis complicated with acute respiratory distress syndrome
- Machine learning insights concerning inflammatory and liver-related risk comorbidities in noncommunicable and viral diseases
- Development of Epstein-Barr virus-associated gastric cancer: Infection, inflammation, and oncogenesis
- Glucagon-like peptide-2 analogues for Crohn’s disease patients with short bowel syndrome and intestinal failure
- Postoperative outcomes and recurrence patterns of intermediate-stage hepatocellular carcinoma dictated by the sum of tumor size and number
- Virological and histological evaluation of intestinal samples in COVID-19 patients
