Comparison between hospital-and community-acquired septic shock in children: a single-center retrospective cohort study
Guo-Yun Su ·Chao-Nan Fan ·Bo-Liang Fang ·Zheng-De Xie·Su-Yun Qian
Abstract Background We explored the differences in baseline characteristics,pathogens,complications,outcomes,and risk factors between children with hospital-acquired septic shock (HASS) and community-acquired septic shock (CASS) in the pediatric intensive care unit (PICU).Methods This retrospective study enrolled children with septic shock at the PICU of Beijing Children’s Hospital from January 1,2016,to December 31,2019.The patients were followed up until 28 days after shock or death and were divided into the HASS and CASS group.Logistic regression analysis was used to identify risk factors for mortality.Results A total of 298 children were enrolled.Among them,65.9% (n =91) of HASS patients had hematologic/oncologic diseases,mainly with Gram-negative bacterial bloodstream infections (47.3%).Additionally,67.7% (n =207) of CASS patients had no obvious underlying disease,and most experienced Gram-positive bacterial infections (30.9%) of the respiratory or central nervous system.The 28-day mortality was 62.6% and 32.7% in the HASS and CASS groups,respectively(P < 0.001).Platelet [odds ratio (OR)=0.996,95% confidence interval (CI)=0.992–1.000,P =0.028],positive pathogen detection (OR=3.557,95% CI=1.307–9.684,P =0.013),and multiple organ dysfunction syndrome (OR=10.953,95%CI=1.974–60.775,P =0.006) were risk factors for 28-day mortality in HASS patients.Lactate (OR=1.104,95% CI=1.022–1.192,P =0.012) and mechanical ventilation (OR=8.114,95% CI=1.806–36.465,P =0.006) were risk factors for 28-day mortality in patients with CASS.Conclusions The underlying diseases,pathogens,complications,prognosis,and mortality rates varied widely between the HASS and CASS groups.The predictors of 28-day mortality were different between HASS and CASS pediatric patients with septic shock.
Keywords 28-day mortality·Children·Community-acquired septic shock·Hospital-acquired septic shock·Septic shock
Introduction
Pediatric sepsis triggered by severe inflammatory responses to infections is the leading cause of mortality and morbidity worldwide,especially in children younger than 5 years old [1–3].It occurs in up to 8% of pediatric intensive care unit (PICU) patients,causing 1 in 4 deaths with a mortality rate ranging from 7.8% to 40% [4,5].Children in developing countries have a significantly higher sepsis-related death rate compared to developed countries (31.7% vs.19.3%) [6].In China the mortality of Chinese children with severe sepsis and septic shock is as high as 34.6% [2].Septic shock is a subset of sepsis,usually resulting in tissue necrosis,multiorgan failure,and death [7].The precipitating factor of sepsis is an infection,which can be categorized as nosocomial or community-acquired infection according to the site of infection.The morbidity and mortality rates of sepsis caused by nosocomial infections are significantly different from those caused by community-acquired infections [8,9].Identifying the causes of these differences is essential to avoid the risk factors of death and to prevent and treat septic shock.
Published data on pediatric sepsis regarding the source of infection are very limited.Murni et al.[10] recently reported that among 2646 patients admitted to the PICU,170 (6.4%) developed nosocomial sepsis,and 70 of these children died (fatality rate of 41%).In another multicenter prospective study of 136 children with sepsis in Spain,22.8% (31/136) had nosocomial infections,of which 29.0%(9/31) died,and 7.6% (8/105) died of community sepsis[11].In a prospective population-based cohort study with 444 episodes of blood culture-proven sepsis in 429 neonates,Giannoni et al.[12] reported that 20% of cases were early-onset sepsis,62% cases were nosocomial late-onset sepsis,and 18% were community-acquired late-onset sepsis.They also showed that hospital-acquired sepsis occurred in infants of lower gestational age and was more frequently associated with comorbidities,wheras community-acquired sepsis was more common in term infants and male infants.Obtaining national or regional data is not an easy process,and data for such studies in Chinese patients is even scarcer.An analysis of a population-based database in China showed that among 21,191 hospitalized adult patients,935 met the diagnosis of Sepsis-3 [7],among which 498 had severe sepsis or septic shock,and 62.1% of Sepsis-3 patients had community-acquired infections.The mortality rate of patients with severe sepsis or septic shock was 53.4% and that of patients with Sepsis-3 was 32.0% [13].Studies on children and infants in developed countries,as well as on adults in developing countries,showed that there were differences in mortality and disease characteristics between nosocomial sepsis and community sepsis.Nevertheless,adequate data on nosocomial and community-acquired infections in children with septic shock in developing countries,especially China,have not yet been available.
This single-center retrospective study was designed to examine the differences in baseline characteristics,treatment,prognosis,outcomes,and risk factors of pediatric patients with hospital-acquired septic shock (HASS) and community-acquired septic shock (CASS),providing further guidance for the prevention and treatment of pediatric sepsis in clinical practice.
Methods
Study design and subjects
We conducted a 4-year,single-center,retrospective cohort study from January 1,2016 to December 31,2019.The study included eligible children from the PICU of Beijing Children’s Hospital.Patients who were 29 days to 18 years old were included,and all patients were diagnosed with pediatric septic shock according to the 2015 Chinese expert consensus diagnostic standard for children (septic shock was diagnosed if children who had sepsis had insufficient tissue perfusion and cardiovascular dysfunction) [14]: (1)hypotension (blood pressure below the 5th percentile for age or systolic blood pressure below the normal value of this age group by less than two standard deviations);(2)vasoactive drugs were needed to maintain blood pressure in normal range (dopamine > 5 μg/kg/min) or any dose of dobutamine,norepinephrine,or epinephrine;and (3) three manifestations of hypoperfusion among 1) peripheral artery pulsation was weak,heart rate and pulse increased rapidly,2) pale or pale gray skin,wet and cold,marbled pattern,3)the capillary refilling time (CRT) was prolonged (> 3 seconds) (except for the influence of ambient temperature),and the CRT could be normal during warm shock,4) early irritability or malaise,apathy,late stage of confusion,even coma,convulsion,5) after fluid resuscitation,the urine volume was still < 0.5 mL/kg/h for at least 2 hours,6) arterial blood lactic acid > 2 mmol/L.Children with incomplete medical records and those who were lost to follow-up were excluded.The study protocol was reviewed and approved by the Ethics Committee of Beijing Children’s Hospital.Patient informed consent was waived.
Groups
In this study the patients were divided into the HASS and CASS group according to whether the sepsis was due to nosocomial or community-acquired infections.The HASS group included patients who had infections 48 hours after admission and developed septic shock.The CASS group included patients who had infections on admission or within 48 hours after admission and had developed septic shock.Children who underwent hemodialysis or intravenous chemotherapy within 30 days or were hospitalized for more than 2 days in the past 90 days were classified as pediatric patients with healthcare-related infections and were also considered as HASS patients [15].
Data collection
Clinical,demographic,diagnostic,antimicrobial,and etiological testing results;empirical antimicrobial therapy;and other treatment history,complications,and prognosis data of pediatric patients were collected from the clinical electronic medical record system (Jiahe System,Beijing).The 28-day survival after septic shock could not be identified from the medical record,and this information was obtained through telephone call follow-ups.Data were collected in the form of variable tables on a secured electronic database.The pediatric index of mortality 2 (PIM2) score was applied as a mortality prediction tool used in the PICU.The primary outcome of the present study was 28-day mortality.Secondary outcomes included in-hospital mortality,length of PICU stay,and length of hospital stay.
Definitions
HASS and CASS were determined based on the definitions by the European Centers for Disease Prevention and Control[16].According to expert recommendations of the 2012 European Committee for Antimicrobial Susceptibility Testing [16],multidrug-resistant (MDR) bacteria were defined as bacteria that obtained non-susceptibility to at least one agent in three or more antimicrobial categories.Extensively drug-resistant bacteria were defined as bacteria that were non-susceptible to at least one agent in all except two or fewer antimicrobial categories (i.e.,bacterial isolates remain susceptible to only one or two categories).The definition of organ dysfunction in children was based on the recommendations of the 2005 International Pediatric Sepsis Conference [17,18].
Statistical analysis
All statistical analyses were performed using SPSS 23.0(IBM Corp,Armonk,NY,USA).Kolmogorov–Smirnov test was used to verify the normality of the continuous data.Quantitative data with normal distribution were denoted by mean ± standard deviation,and quantitative data with a nonnormal distribution were denoted by median and quartiles.Quantitative data with a normal distribution (or non-normal distribution) of the two groups were analyzed using the Student’sttest (or the Mann–WhitneyUtest as a nonparametric test).Categorical variables were presented as a count (percentage) and were analyzed using Pearson’s Chi-square test or continuous correction Chi-square test.To determine the risk factors for 28-day mortality of children with septic shock in the two groups,multivariable logistic regression analyses were conducted.The variables included in these analyses were the statistically significant variables in the univariable analyses and were tested for multicollinearity.The results of the multivariable logistic regression analyses were reported as adjusted odds ratio (OR) and 95% confidence interval (CI).Statistical significance was established atP< 0.05.
Results
General information
In this study 325 children with septic shock were initially identified.Among them,21 patients were excluded because their data were incomplete,and six patients were excluded because they were lost to follow-up.Finally,298 patients were included in this study (Fig. 1).Among them,91(30.5%) patients were in the HASS group,and 207 (69.5%)were in the CASS group.In the HASS group,37 (40.7%)patients were from the hematology department,10 (11.0%)patients were from the PICU,five (5.5%) patients were from the surgery department,11 (12.1%) patients were from other internal medicine departments,and 28 (30.8%) patients were from other hospitals.The median age of the HASS children was 5.2 (1.2–10.8) years,and 64.8% (59/91) were male.The PIM2 score at PICU admission was 9.6 (4.1–14.8) in the HASS group.In the CASS group,the median age of the children was 2.3 (0.6–8.2) years,60.9% (126/207) of them were male,and the PIM2 score at the time of PICU admission was 8.5 (5.1–16.1) (Table 1).The characteristics of the pediatric patients are shown in Table 1.
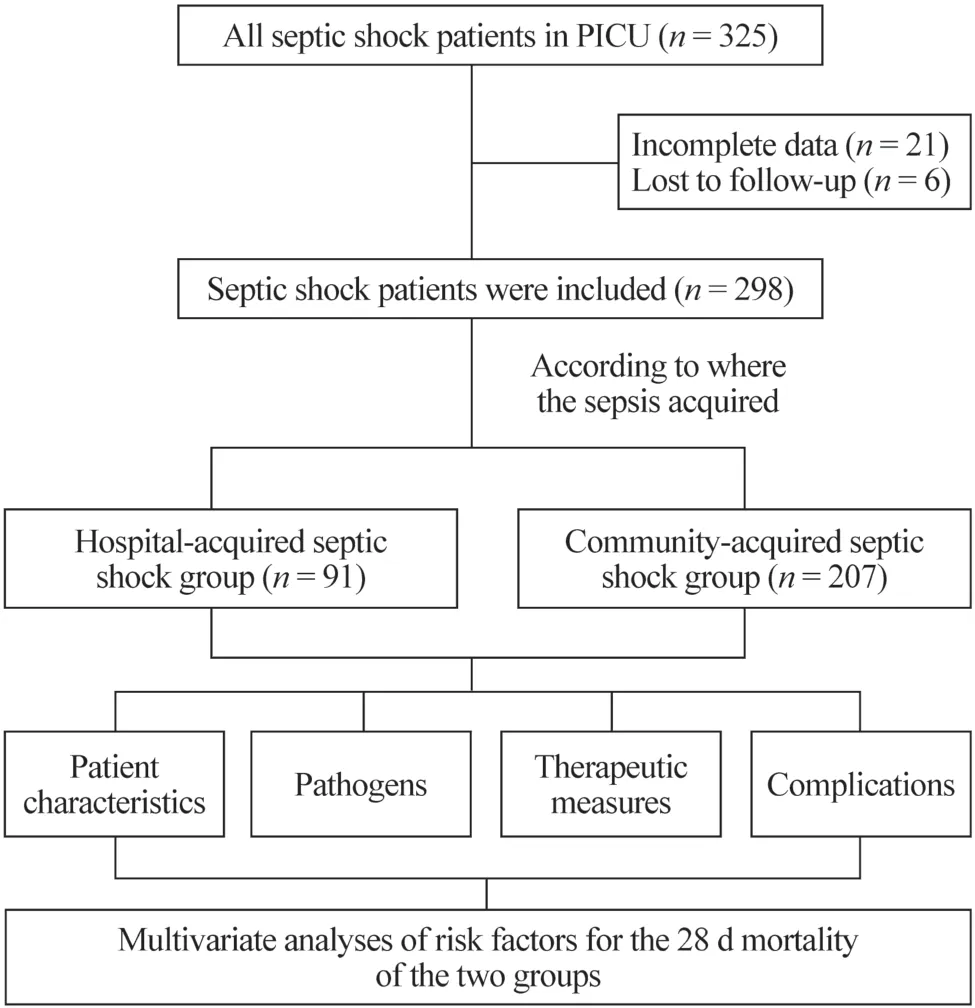
Fig.1 Flowchart of the study
Infection sites and distribution of causative microorganisms
In this study the most common infection sites were the digestive tract,respiratory tract,bloodstream,and central nervous system.Bloodstream infection was dominant in the HASS group (36.3%) compared with the CASS group (11.1%).The CASS group had a higher number of patients with respiratory tract infections (25.1%) and central nervous system infections (22.2%) (Table 1).
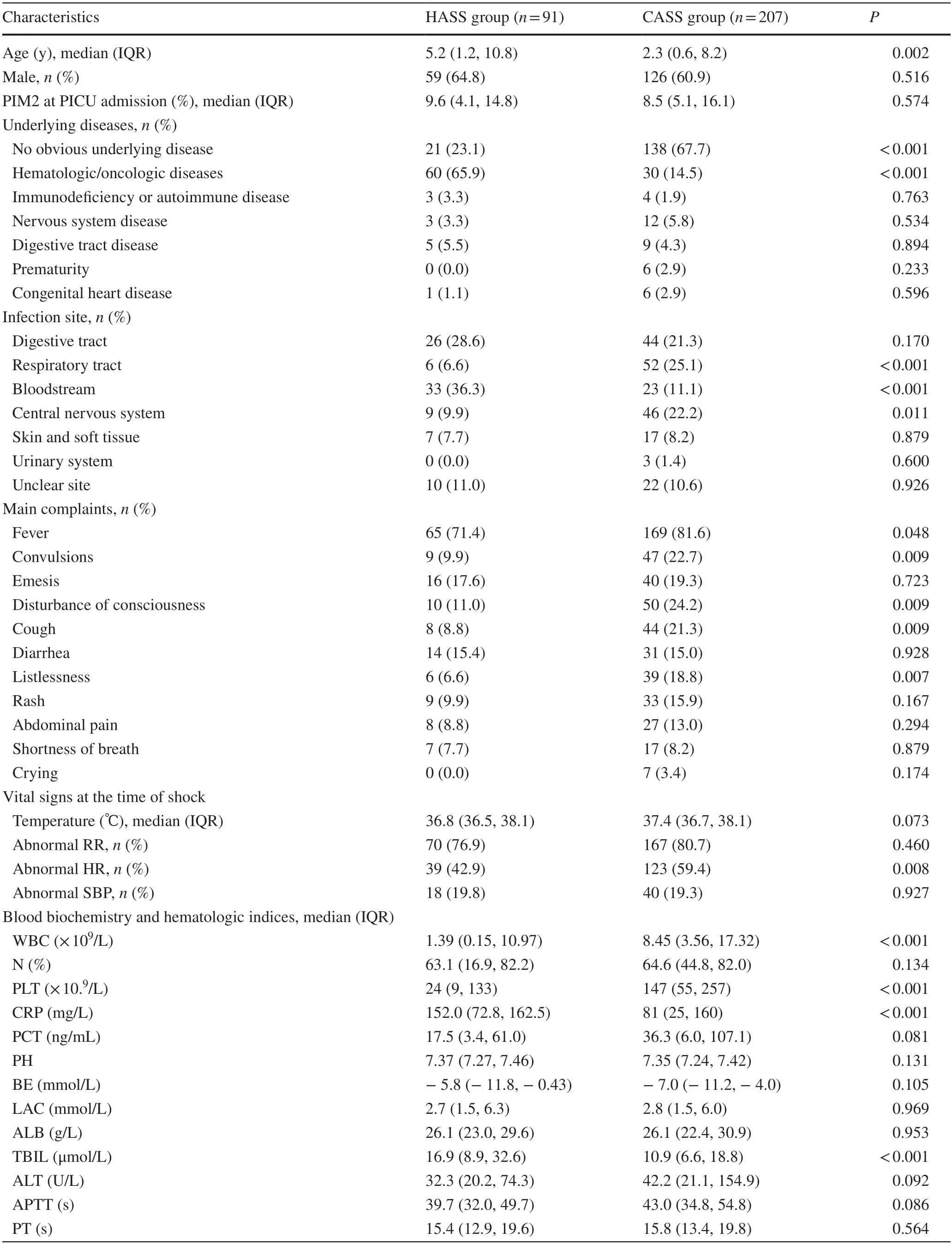
Table 1 Demographics and clinical data of children with septic shock
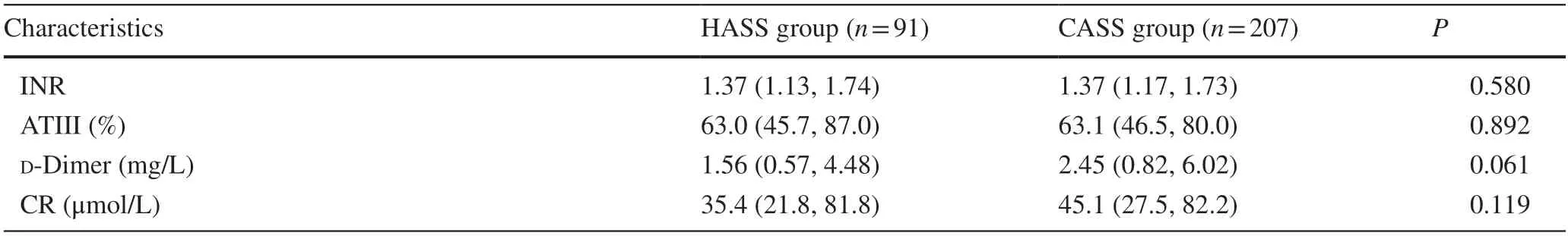
Table 1 (continued)
The microbiological test results of patients are shown in Table 2.A statistical difference in pathogen distribution was observed.The patients in the CASS group had more Grampositive bacterial infections than those in the HASS group(P< 0.001).Among Gram-positive pathogens,a higher rate of infection fromStaphylococcus aureuswas observed in the CASS group (10.1%) compared with the HASS group(1.1%) (P< 0.001).
A higher number of patients in the HASS group had Gram-negative bacterial infection (47.3%) compared to the CASS group (16.9%) (P< 0.001).The detection rate ofKlebsiella pneumoniaeandPseudomonas aeruginosain the HASS patients was 18.7% and 12.1%,respectively,higher than those in the CASS group (3.4% and 5.3%;P< 0.001 andP=0.039,respectively).A significant difference was observed in MDR bacterial infection between the HASS(39.6%) and CASS groups (28.0%) (P=0.048).
Supportive and antimicrobial therapies
A significant difference in the use of empirical antimicrobial therapy on the first day between the two groups was observed.The patients in the CASS group were mainly given two antimicrobial drugs (55.1%).In contrast,more than two antimicrobial drugs were used for patients in the HASS group (54.9%) (Table 3).
Complications and outcome
The CASS group had more patients with cerebral dysfunction compared to the HASS group.No significant differences were observed in the proportion of multiple organ dysfunction syndrome (MODS) and other complications between the two groups.The total 28-day mortality rate of the two groups was 45.0% (134/298).Statistically significant differences were observed between the HASS (62.6%) and CASS groups (37.2%;P< 0.001).The in-hospital mortality rate in the HASS group (33.3%) was higher than that of the CASS group (12.1%;P< 0.001;Table 4).
Predictive risk factors for 28-day mortality in children with septic shock
In this study the variables mentioned previously (Table 5)were included in the univariable logistic regression analysis of the 28-day mortality rate.For all patients,HASS,combined hematologic/oncologic diseases,PIM2,lactate (LAC),platelet (PLT),activated partial thromboplastin time,international normalized ratio,total bilirubin,mechanical ventilation,vasoactive drug therapy,renal replacement therapy,positive pathogen detection,respiratory failure,renal injury,cerebral dysfunction,and MODS were associated with the 28-day mortality rate.Combined hematologic/oncologic diseases,PLT,invasive mechanical ventilation therapy,MODS,vasoactive drug therapy,and positive pathogen detection were related to the 28-day mortality in the HASS group.In the CASS group,PIM2,activated partial thromboplastin time,international normalized ratio,creatinine,pH value,LAC,invasive mechanical ventilation therapy,respiratory failure,renal injury,disseminated intravascular coagulation,cerebral dysfunction,and renal replacement therapy were associated with the 28-day mortality (Table 5).
The results of multivariable logistic regression analysis after excluding the collinear predictors showed that HASS,combined hematologic/oncologic disease,LAC,PLT,mechanical ventilation,positive pathogen detection,renal injury,and MODS were risk factors in all children with septic shock.PLT,positive pathogen detection and MODS were risk factors for 28-day mortality in the HASS group.LAC and mechanical ventilation were risk factors for 28-day mortality in the CASS group (Table 6).
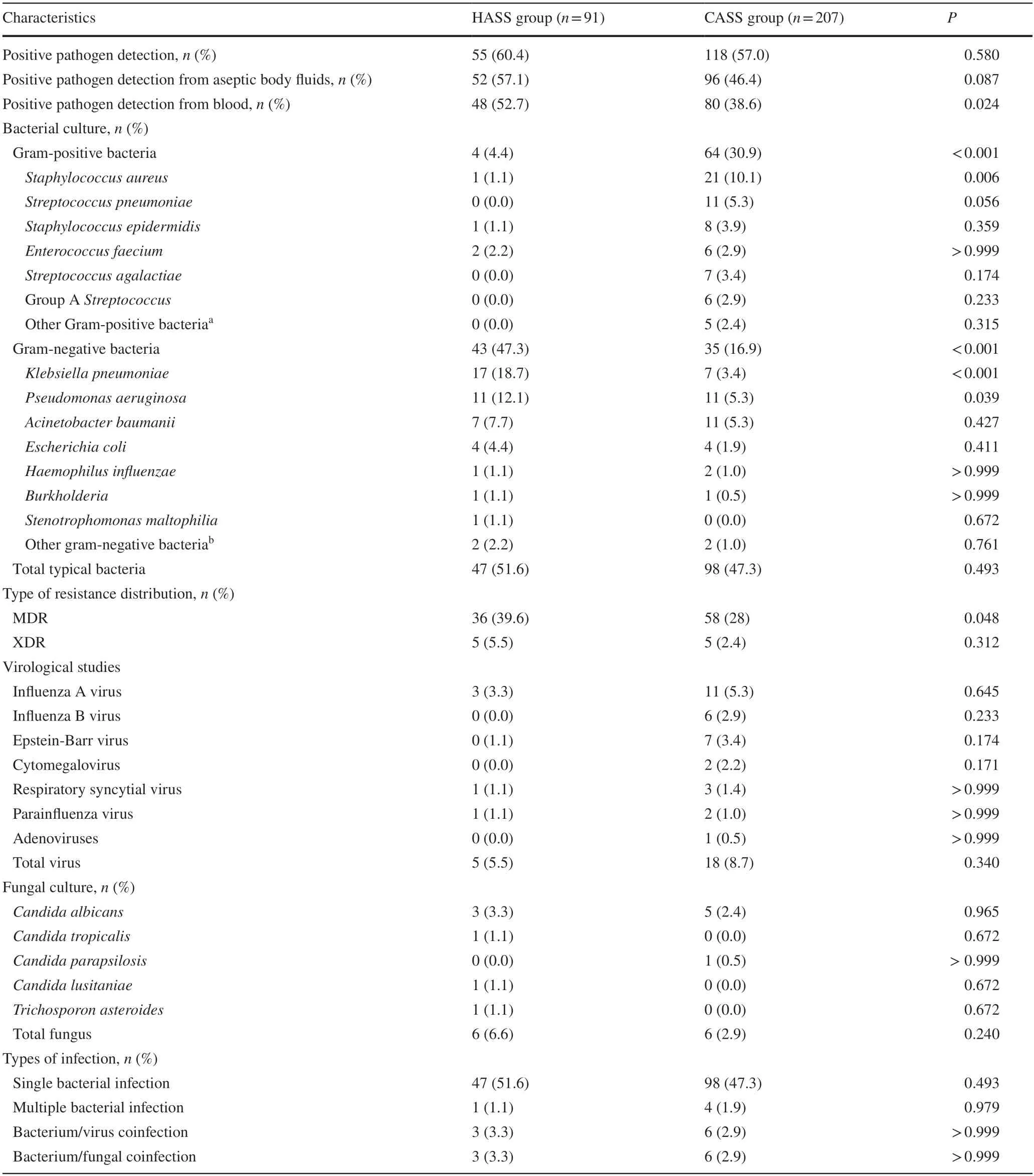
Table 2 Distribution of the causative microorganisms in pediatric patients with septic shock
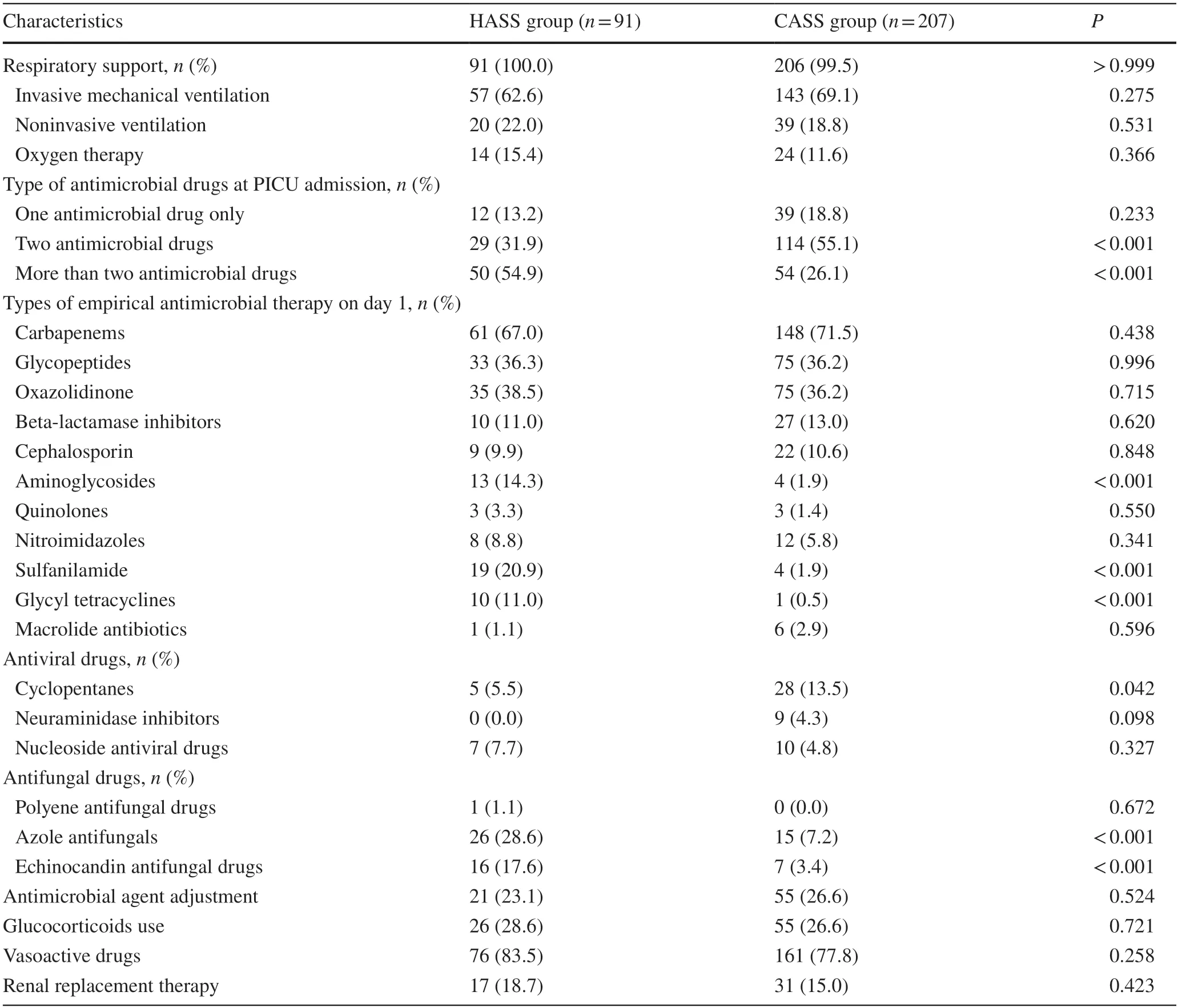
Table 3 Supportive and antimicrobial therapies in pediatric patients with septic shock
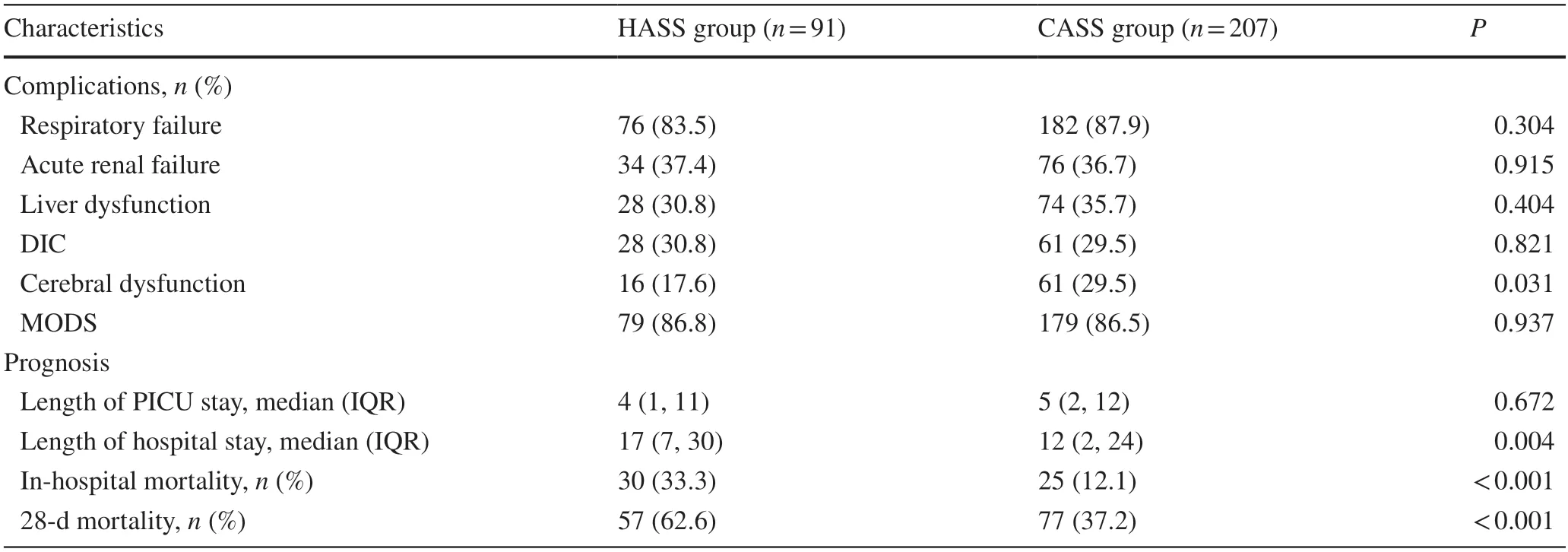
Table 4 Complications and outcomes in pediatric patients with septic shock
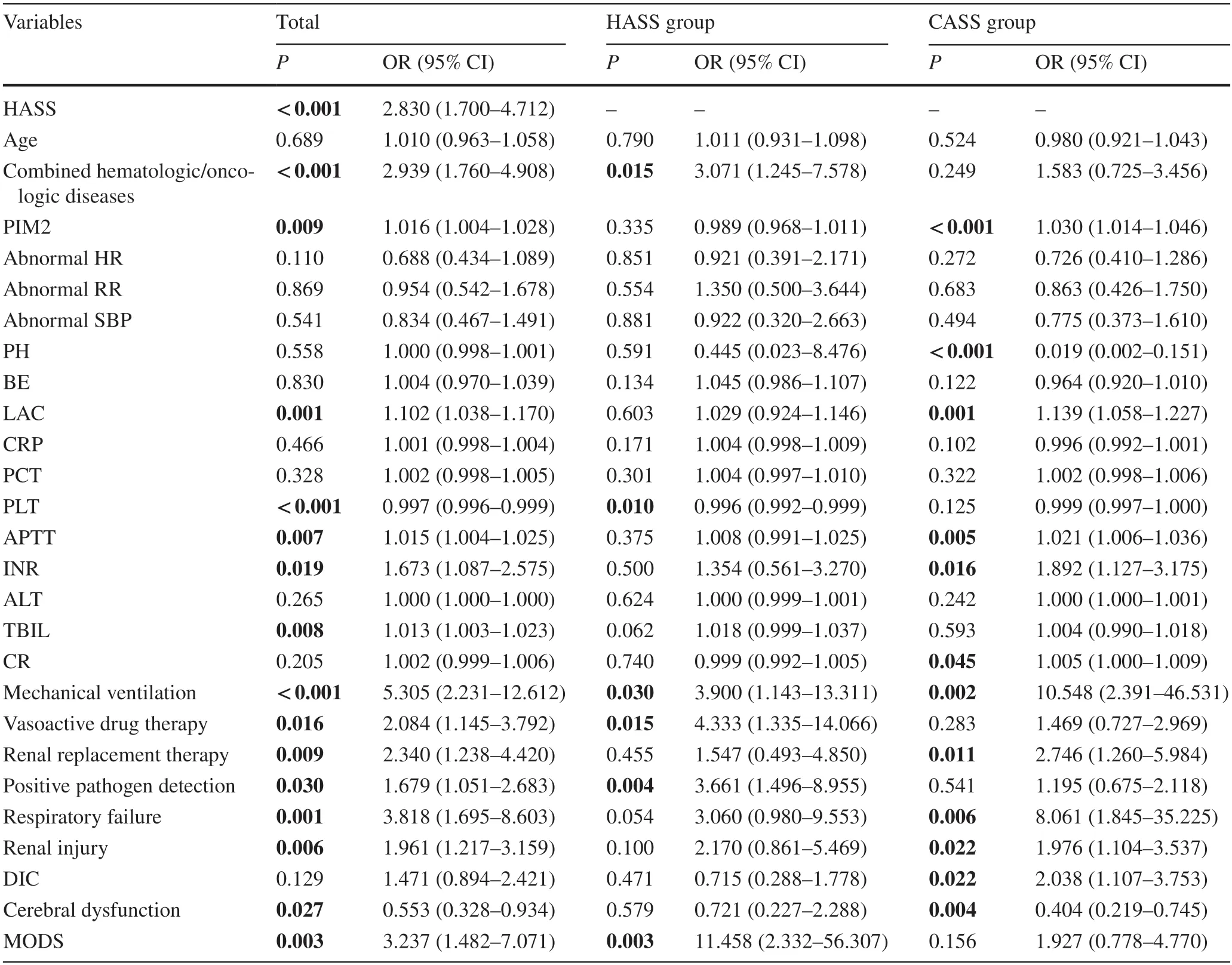
Table 5 Univariable logistic regression analysis of 28-day mortality in children with septic shock
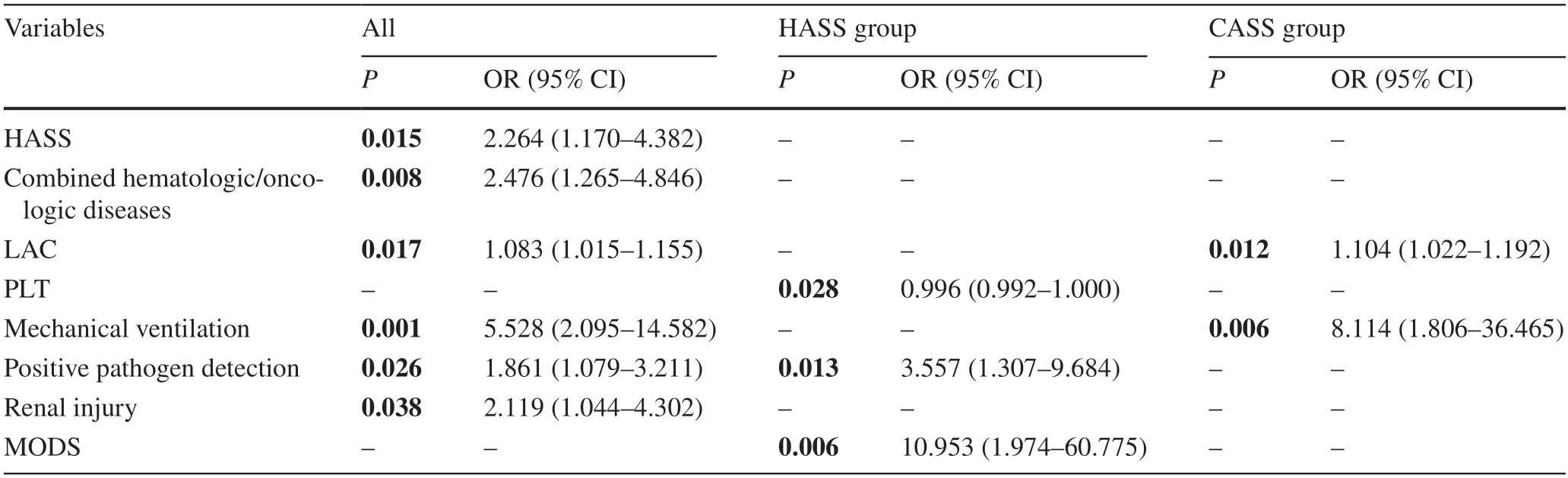
Table 6 Predictors of 28-day mortality in children with septic shock from multivariable logistic regression analysis
Discussion
In the present study several differences were observed between pediatric patients with HASS and CASS.The underlying diseases,pathogens,infection sites,and mortalityvaried widely between HASS and CASS;in addtion,the predictors of 28-day mortality were different.
Several studies have been conducted to assess the differences between HASS and CASS,but the study on Chinese children is limited.Regarding the difference in basic diseases,published data have suggested that most blood malignancies in HASS patients can lead to immune deficiency,which is a risk factor for infection and death [19–21].In addition,neutropenia was shown to be one of the factors that could increase the risk of infection [22].HASS patients presented bloodstream and digestive tract infections,which was similar to the findings by Westphal et al.and Baker et al.[23,24].Baker et al.demonstrated that chemotherapy damages the gastrointestinal mucosa and that enterogenic sepsis and bacteremia occur in hospitals [24].The main site of CASS was the respiratory tract,which was in line with the results of the current study [23].Significant differences have previously been observed in microbiological infection profiles between HASS and CASS patients [25,26].Under the influence of gastrointestinal mucositis caused by chemotherapy and long-term neutropenia,children with nosocomial infections,especially hematologic neoplasms,were at high risk of Gram-negative bacteremia [24].Nonetheless,the predominant type of pathogen in CASS is Gram-positive bacteria [27].
The 28-day mortality of patients varied in the HASS and CASS groups.Similar conclusions were reached for a multicenter cohort study,in which the mortality rates fromnosocomial and community-acquired infections were 64.6%and 37.5%,respectively [28].A previous study showed that immune deficiency and granulocytopenia increased the risk of death from sepsis,and the majority of children in our study were hospitalized for chemotherapy due to hematologic neoplasms diseases [29].
The predictors of 28-day mortality in the two groups varied remarkably.The multivariable logistic regression analysis showed that the risk of 28-day mortality in HASS increased with positive pathogen detection or MODS.PLT was shown to be a protective factor for mortality in children with HASS.In patients with CASS,the increase of LAC and the need for mechanical ventilation were risk factors for 28-day mortality.Another study found that bloodstream infections acquired in the intensive care unit were related to increased mortality [30],which was consistent with the present study.Furthermore,MODS might be a predictor of sepsis mortality,which has been verified in previous studies [31–33].On the other hand,some studies have analyzed MODS as a dependent variable for outcome or prognosis [34].In this study organ function was restored in 60.9% of patients with CASS post-treatment.In the HASS group,30.4% of children with MODS survived;therefore,irreversible MODS is deemed a direct risk factor for death from septic shock because MODS is a severe manifestation[35].Several studies revealed that PLT should be included in the prognosis model of sepsis in children [36,37].The prognostic power of PLT has been studied extensively in adults [38–40],and PLT might play a key role in coordinating the host inflammatory response [38].Hematological/oncological diseases were predominant in the HASS group.Due to tumor and chemotherapy,white blood cell and PLT levels were lower than normal,and the effect on prognosis was more prominent than in patients with normal PLT count and function.Therefore,the predictive value of PLT should be explored according to the characteristics of different populations.Accumulating evidence from adults and children showed that LAC was related to the prognosis of septic shock [41–44],and most of the cases had communityacquired infections,which was consistent with the present study.Similar to previous studies,the mortality in the CASS group could be predicted by mechanical ventilation [37,45].Due to severe conditions of patients treated with invasive ventilators and to adverse effects of invasive ventilation on hemodynamics,the need for invasive mechanical ventilation is a risk factor for mortality [46].
The highlights of the current findings were as follows:first,the children in the HASS group had significantly fewer complaints than those in the CASS group.Similar findings were noted in the study by Heinz et al.[47],wherein the patients with neoplasm of neutropenia presented atypical or indistinct signs and symptoms of infection,and fever might be the sole clinical symptom.Therefore,early attention should be paid to fever in HASS pediatric patients.Second,many Gram-negative bacterial infections in CASS were involved in nosocomial infections.It is not uncommon for these drug-resistant Gram-negative bacteria to cause infection in the community and have drug resistance[48–51] because the patients often have underlying diseases[52].In a study in Milan conducted on adults,the resistance rate of the community infection was about 17% [53].In a pediatric study in China,the overall resistance rate of Gram-negative bloodstream infections was 60.1% [54].The high drug resistance rate of community infection requires the attention of medical staffand society.The emergence of drug-resistant bacteria poses significant challenges tothe selection of antibiotics and the risk of death.Third,in this study the first antibiotic selection for CASS patients was excessive.Although the antibiotics were adjusted after obtaining the microbial results,the selection should be based on guidelines,patient status,local microorganisms,and drug resistance.Fourth,PIM2 is a predictor of death but not HASS in the present study.Interestingly,PIM2 estimates were significantly lower than the actual 28-day mortality rate.Several studies confirmed that PIM2 has a good prediction ability for critical illness but differed significantly from that in the HASS group.Edwards et al.and Fonseca et al.revealed a higher mortality rate for complex chronic conditions than predicted by PIM2 [55,56].In a report in 2014,PIM2 was shown to have a significant effect on treatment prior to admission to the PICU,and both age-uncorrected physical sign data and the inapplicability of high-risk diagnoses of PIM2-specific regions may be biased [57].In addition to the above factors,unscheduled hospitalization also increased the bias between PIM2 predictions and actual deaths in our data.
Nevertheless,the current study had some limitations.First,this was a single-center retrospective cohort study that relied on routine clinical data,with lost cases and a small amount of missing data on the variables.Second,although the total number of cases was approximately 300,data of multifactor regression analysis after grouping were less.Because some patients were transferred to our hospital after they developed septic shock,information on neutrophils,anemia,PLT,central venous catheterization,immunosuppressive state,mucosal barrier destruction,andother potential organ dysfunctions could not be obtained.Third,we found that the mortality of children with septic shock was extremely high,that the high-grade antibiotics were the preferred antimicrobial drugs,and that high rates of drug-resistant bacteria were detected in the CASS group.However,because the study was based on a special population and treatment measures,the conclusions cannot be applied to other PICUs indiscriminately.For the logistic regression model,we required more patients to ensure the stability of the model;therefore,more outcome events are imperative to substantiate these findings.
In conclusion,the underlying diseases,pathogens,complications,prognosis,and mortality rates varied widely between HASS and CASS.The predictors of 28-day mortality differed between HASS and CASS pediatric patients with septic shock.
AcknowledgementsThe authors of this paper greatly appreciate Su-Yun Qian’s invaluable mentorship and guidance and would like to thank all the nurses and doctors in pediatric intensive care unit in Beijing Children’s Hospital.Finally,the authors also appreciate all the Medical Record Office stafffor their convenience and assistance in retrieving this medical record.
Author contributionsQSY participated in the study concept and design,critical revision of this article for important intellectual content,and final approval of the version to be published.SGY carried out study design and data acquisition,analysis,and interpretation;and drafted the manuscript.FCN and FBL participated in the study concept and design.All authors read and approved the final manuscript.
FundingThis work was supported by the CAMS Innovation Fund for Medical Sciences (No.2019-I2M-5-026).The funder had no role in study design;in the collection,analysis and interpretation of data;in the writing of the report;and in the decision to submit the article for publication.
Data availabilityThe data from this study are available from the corresponding author upon reasonable request.
Declarations
Ethical approvalThe study protocol was reviewed and approved by the Ethics Committee of Beijing Children’s Hospital (approval number:2020-Z-040).The patient's informed consent has been waived.
Conflict of interestNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.The authors have no conflict of interest to declare.
Open AccessThis article is licensed under a Creative Commons Attribution 4.0 International License,which permits use,sharing,adaptation,distribution and reproduction in any medium or format,as long as you give appropriate credit to the original author(s) and the source,provide a link to the Creative Commons licence,and indicate if changes were made.The images or other third party material in this article are included in the article's Creative Commons licence,unless indicated otherwise in a credit line to the material.If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use,you will need to obtain permission directly from the copyright holder.To view a copy of this licence,visit http:// creat iveco mmons.org/ licen ses/ by/4.0/.
 World Journal of Pediatrics2022年11期
World Journal of Pediatrics2022年11期
- World Journal of Pediatrics的其它文章
- Pediatric dysphagia overview: best practice recommendation study by multidisciplinary experts
- Determinants of neonatal jaundice in Ethiopia: a systematic review and meta-analysis
- Pathogenic changes of community-acquired pneumonia in a children’s hospital in Beijing,China before and after COVID-19 onset:a retrospective study
- Effect of early atopic sensitization in children aged 0–2 years on the development of asthma symptoms at 9–11 years of age
- Integration of multiscale entropy and BASED scale of electroencephalography after adrenocorticotropic hormone therapy predict relapse of infantile spasms
- Neutropenia: diagnosis and management
