Nursing undergraduates’ experiences of a simulation-centred educational program in hospice care in Macao: A qualitative research
Yan Wang,Haobin Yuan
Macao Polytechnic University,Macao SAR,China
Keywords:Curriculum Hospice care Nursing students Qualitative research Teaching
ABSTRACT Objectives: The study aimed to explore the experiences of nursing undergraduates participating in a simulation-centred educational program in hospice care in Macao,China.Methods:This descriptive qualitative study was based on the data collected through semi-structured individual interviews.Seventeen nursing undergraduates in Macao,China who attended the simulation-centred program in hospice care participated in this qualitative from November to December 2020.This program included three parts: introduction to hospice care (2 h),management of terminal symptoms (10 h),and hospice situation simulations (6 h).The interview data were analyzed using qualitative content analysis.Results:This study revealed two themes and six sub-themes.Theme 1 was developing competencies in caring for dying patients and their families,which included four subcategories of sensitivity to patients’needs,knowledge of hospice care,skills of symptom control and comfort supply,and communication skills.Theme 2 was improving the ability to self-care and support colleagues,which included two subcategories of reflection on life and death and sharing and supporting among colleagues.Conclusion:This program improved the competency of nursing undergraduates in hospice care and participants’ learning experience was good.
What is known?
· Undergraduate nursing students’ competency in hospice care was insufficient.
· The hospice simulation effectively improved students’ knowledge,attitude,communication skills,self-efficacy,satisfaction,and performance.
What is new?
· Undergraduate nursing students’ experiences of a simulationcentred educational program in hospice care were described.
· The simulation-centred educational program improved students’ competency in hospice care.
1.Introduction
Nurses are always put into the centre of hospice care,relieving the dying physically,psychologically,socially,and spiritually.With the aging population and the uprising morbidity of chronic diseases,there is a universal and urgent summon for well-trained nurses to provide compassionate care and ensure dignity for terminal patients.Despite the international advocate of incorporating hospice education into the nursing bachelor’s curriculum,most nursing programs fail to provide enough education [1].Many factors contributed to inadequate education [1-3],including limited curriculum time,inadequate practising units,overly prudent clinical tutors,high tension in real hospice situations,and students’difficulty applying theory to the clinic.Hospice theoretic learning was merged into other subjects,while hospice clinical practice could not always be guaranteed.Insufficient education made students ill-prepared for hospice care.Chover-Sierra et al.found that 619 nursing students’knowledge of hospice care was medium-low through an online survey[4].The another descriptive study showed that 187 junior nursing students had insufficient knowledge and self-efficacy in hospice care[5].Insufficient knowledge resulted in students’ poor attitudes toward hospice care and potentially hindered the provision of high-quality hospice care [6].Among the survey by Thampi,only 39% of nursing students showed positive attitudes toward caring for the dying[7].Inadequate education lead to nurses’ incompetence,thereby reducing the quality of nursing.Marchˊan’s investigation revealed that more than 60% of nursing professionals felt insufficient education to care for the dying [8].
Educators’ endeavours were presented in educational interventions in hospice care.For example,Cha et al.’s study confirmed the positive effects of hospice education,composed of 16 h of lectures,by promoting medical students’ knowledge and attitude toward hospice medicine [9].Choi et al.used a hospice program consisting of 10 3-h sessions to improve participants’perception of hospice,attitude towards death,and meaning of life,and teaching methods included lecture,video-watching,presentation,and discussion [10].Tamaki et al.improved students’knowledge,skill performance,and self-confidence through a hospice simulation with standardized patients[3].A wide range of teaching strategies was used in previous research,such as didactic instructions,clinical practice,and simulation-based activity [11].The didactic instructions were good at knowledge teaching,while clinical practice provided students with authentic participation.The limited opportunities of hospice clinical practice put light on the simulation-based method.As an experiential learning method,the simulation was increasingly accepted as a preparation,substitute,or supplement for hospice clinical practice.One systematic review,which included the end-of-life education programs from 2008 to 2018,concluded that simulation-based activities were the primary educational method and were considered valuable and beneficial for learning in end-of-life education programs [12].
Most simulation-based activities in previous studies carried out one or two simulation scenarios based on complex hospice cases.Hjelmfors et al.[13] conducted three simulation scenarios in one day to train students’communication skills in challenging hospice situations.Montgomery et al.[14]incorporated hospice simulation into the community health nursing curriculum.The 30-min simulation was about a cancer patient in his last stage.Sarabia-Cobo et al.’s [2] study used two simulation scenarios of cancer patients,and each was composed of a scenario (15 min) plus a debriefing (25 min).Lippe et al.[15] designed a 2-h simulation consisting of four parts: continuation of care,change in status,withdrawal of care,and debriefing.In Mahan’s research [16],two simulated scenarios were compared with a 6-to-8-hour actual hospice.Saylor et al.paired nursing and medical students to form the hospice care team to conduct a 1.5-h inter-professional hospice simulation [17].In Kopka et al.’s research [18],a three-credit gerontology course used integrated teaching strategies,and the simulation scenario was used as an ending to this course.The patient’s death was simulated in 10 min,followed by 20 min of debriefing.Tamaki et al.adopted a 30-min simulation as the educational intervention in a random controlled trial [3].
Our literature review revealed that most previous studies did not equip students with enough hospice knowledge before simulation scenarios.Additionally,the time of simulation scenarios allowed students to apply knowledge,and practice skills were limited.Both theoretical learning and simulation practice had their benefits,making them unable to replace each other.While theoretical understanding was vital as the foundation of the learning process,experiential learning was good at bridging the gap between theory and practice[19].Hospice care was characterized by profound and complex knowledge and practical nursing skills.Inadequate knowledge preparations and limited scenarios practice might not lead to profound and persistent changes in nursing students’ competency in hospice care.
1.1.Background
After preliminary confirmation of the effectiveness of simulation-based activities in hospice education,it was time to refine and deepen this approach.The undergraduate nursing curriculum did not have the subject of hospice care in Macao,China.An 18-h simulation-centred hospice care program was developed,and quantitative and qualitative methods were used to assess the effectiveness of this program.
The program was named simulation-centred because the simulation was strengthened by theoretical lectures and diversified by mini-simulations and situation simulations.It was composed of three parts:introduction to hospice care,management of terminal symptoms,and hospice situation simulations.In Part 1 (2 h): by theoretical lecture,the evolution and fundamental theories were introduced,integrating hospice care into social networks,emphasizing nurses’ role in bridging relative professionals to help the dying and their families.Part 2(10 h)was concentrated on training participants’ patient-centred hospice competency.The teaching methods used in this part included lectures and mini-simulations.Terminal symptoms were classified into small groups.We lectured on one group of symptoms,and then a mini-simulation closely followed.In Part 3 (6 h): besides allowing participants to demonstrate their hospice competency,this part focused on constructing nurse-inwards competency.The teaching methods used in this part included pre-briefings,simulation scenarios,and debriefings.Participants were divided into the patient,nurse,and family groups to be involved in the simulation scenarios [20].
1.2.Aim of the study
In line with previous studies,the first component of our research got positive quantitative results which showed this program could elevate students’ scores in hospice knowledge and attitude.This article,as the second component of this study,aimed to provide a descriptive and in-depth understanding of nursing students’ experiences in this program by the qualitative method.
2.Methods
This was a descriptive,qualitative study conducted in Macao,China.Data were obtained from semi-structured individual interviews and analyzed using qualitative content analysis.
2.1.Participants
This study recruited voluntary participants from Year 2 and Year 3.Year 1 students were not invited because their nursing knowledge was not ready for this training.Year 4 students spent most of their time in clinical practicum and could not coordinate with the schedule of this program.Total 52 students finished the whole program.Purposive sampling was performed to gain rich and diverse data.The students who were good at asking questions during lectures,actively involved in simulation practices,proactively participated in discussions,mentioned their memorable lifeand-death experiences,and initiatively sharing feelings during the debriefing were invited to attend the interview.Data collection and analysis were carried out simultaneously.Data collection was stopped by the sign of no new data appearance.Data saturation was achieved when the number of interviewees reached 17 (Table 1).
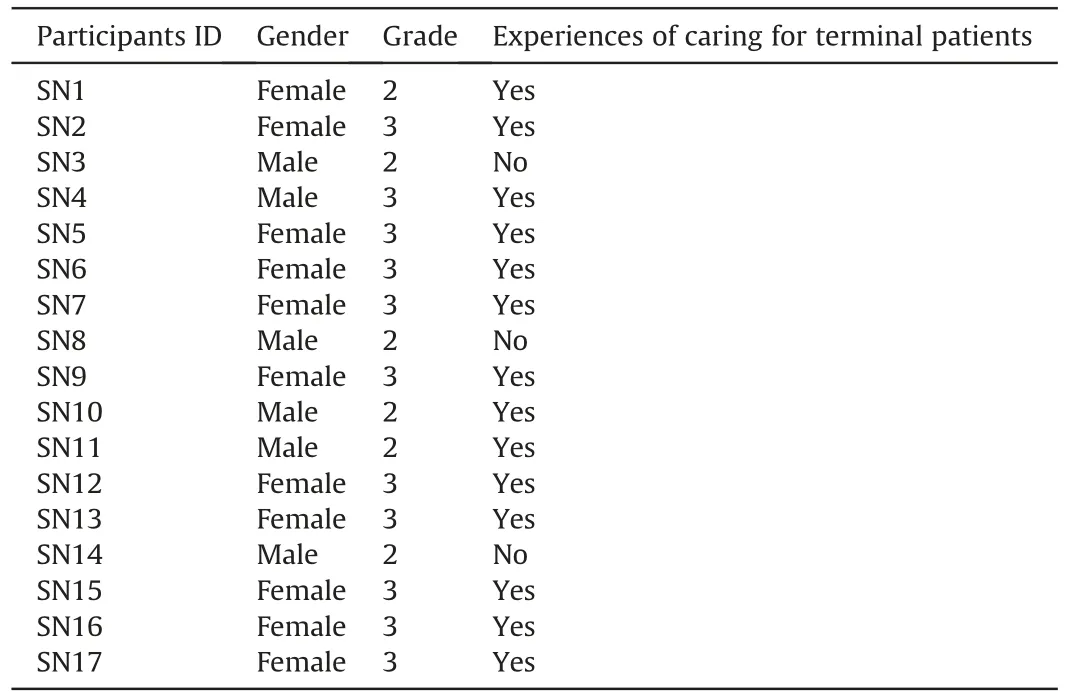
Table 1Demographic data of the participants.
2.2.Data collection
Data were collected using semi-structured interviews by the primary researcher (Y.Wang).The interviews were conducted inNovember and December 2020.Participants were invited to a quiet university room and interviewed individually to ensure that personal experiences were freely and fully expressed.Before the interview,the objectives of this research were explained,and a consent form was gained.The demographic data were collected,including the gender,grade,and experiences of caring for terminal patients.The time of each interview ranged from 17 to 44 min (around 30 min).Two researcher(Y.Wang and H.Yuan)developed the interview question scheme,which was composed of two questions.Question 1,“How did you feel when you learned about hospice care?”was used to detect students’experiences of hospice care learning.Question 2,“What do you think about the teaching methods used in this hospice educational program?” was used to detect students’ experiences of the teaching methods used in this program.The interviews were voicerecorded and transcribed verbatim by Y.Wang.The transcripts were sorted and sent back to interviewees for confirmation.
2.3.Data analysis
It was performed by the qualitative content analysis method based on the process mentioned by Graneheim and Lundman [21].The content analysis helped to understand the manifest and latent experiences of participants.The process was performed by condensing,aggregation,and abstraction for identifying meaning units,coding,classifying categories,and constructing themes.Two researchers (Y.Wang,H.Yuan) performed the data analysis independently using Nvivo 12.0: 1) read all data repeatedly and immersedly while highlighting meaning units in the text which appeared to capture critical concepts;2) approached the texts by making notes,condensing text and labelling for codes;3) initial coding scheme was decided after open coding of three transcripts by discussion between two researchers;4) coded the remaining transcripts and revised the initial coding scheme;5) codes were sorted into subcategories;6) combined subcategories into categories;7)constructed themes.An example of data analysis showed in Table 2.

Table 2Example of data analysis.
2.4.Ethical consideration
The university ethical committee approved the study (RP/ESS-02/2018).Inform consent was gained from every participant after explaining the study.The right of withdrawal and personal data confidentiality was ensured.
2.5.Trustworthiness
The research team consisted of two associated professors from Macao Polytechnic University.The two researchers,with Doctor’s degrees,had experience in caring for dying patients and families in clinical ICU work.W.Yan was responsible for the university elective course named Life and Death Education.H.Yuan was an expert in pedagogical research and published articles on the research of teaching methods.H.Yuan and W.Yan were the university’s simulation teaching organizers and published articles related to simulation education.
Two researchers developed the interview questions scheme.To gain dependability,W.Yan interviewed all participants.The teacherand-student relationship may cause interviewees to hold negative experiences,so the interviewer tried to create a tranquil,open,and relaxed atmosphere.The interviewer kept dynamic interaction by asking follow-up questions and requesting interviewees to verify and explain their words.There was no time limitation in the interview to ensure rich data collection.Field notes were taken to mark the interviewee’s particular facial expressions,posture,and voice tone.The coding scheme was refined gradually on the two researchers’consensus.Two researchers do the data analysis dependently.The intersubjective understanding of each’s results was achieved by regular discussion.We supplied interviewees with the transcripts and final analysis results to gain their confirmation.We described the educational interventions clearly and provided an example of the data analysis process to reach transparency.This study was reported according to the COREQ checklist[22].
3.Results
This study revealed two themes and six sub-themes: 1) Developing competencies in caring for dying patients and their families(sensitivity to patients’ needs,knowledge of hospice care,skills of symptom control and comfort supply,communication skills);2)improving the ability to self-care and support colleagues(reflecting on life and death,sharing and supporting among colleagues).
3.1.Theme 1: Developing competencies in caring for dying patients and their families
Through theoretical learning,practising and reflection,students showed their improvements and feelings in caring the dying patients and families.
3.1.1.Sensitivity for patients’ needs
Being sensible to patients’needs was the first step to supplying suitable nursing.Students learned to detect patients’ physical and psychological needs.
Students mentioned that they initially did not know what to do and what to say facing a dying patient.
“Maybe it was because I did not know his needs.” (SN6)
One student reported,
“Most dying patients seldom expressed their needs and kept worried and complaining.” (SN8)
Students learned special assessing techniques to detect patients’physiological needs.
“I knew he was in pain because I learned the pain gave information through vital signs,breathing sounds,posture,and even the facial expressions.”(SN6)
Students began to look through miserable symptoms to detectpatients’ psychological needs.Instead of asking “What do you need?” they used chatting.
“After practicing talking many times in simulations,I found that patients might not directly voice their needs.For example,the patient’s praise of my beautiful hair might show her worry about her sick appearance before visiting friends.Next time,I would use her scarf to make a beautiful cap.” (SN15)
A student said,
“When I knew what did he want,I transferred my heart from anxiety to his needs.” (SN5)
3.1.2.Knowledge of hospice care
Students’ knowledge enrichment was presented in the fundamental principles of hospice care,symptom management,and pharmacy.
We lectured students on the significance of hospice care.One student said,
“I recognized the hospice care could help every single patient and benefit the whole society.” (SN3)
One student emphasized that the most significant gain from this program was
“The core of hospice care is not to cure,but to comfort and accompany,which gave me a great relief from the pressure of saving lives.” (SN14)
We lectured on terminal symptoms that dying patients shared regardless of original diseases before mini-simulations.Most students said,
“Understanding the mechanism was vital for symptom control.The knowledge was brand new for us,and lectures showed me a clear and detailed knowledge system.It should be taught before simulations.” (SN8)
One student recalled her experience of the patient’s terrifying death rattles.
She said,
“Now I am not afraid anymore because I understood the sound was coming from the patient’s disability to swallow thicksecretions because of the relaxation of oropharyngeal muscles.”(SN15)
A student mentioned his once guilty experience of a wound dressing,for he believed it was him that caused the patient’s continuous bleeding.“This course gave me relief! Considering the hyperplasia and weakness of the capillary in malignant wounds,I will be more careful next time.” (SN4)
Their pharmacy knowledge was deepened,
“I could never imagine such a wide range of analgesics could be used.We should not let Morphine handle every pain.Now I knew the non-steroidal anti-inflammatorydrugs (NSAIDs) combined with steroids might help the pain of bone metastasis,while tricyclic antidepressants may be needed for nerve pain.I felt confident that I could give suggestions to doctors.” (SN8)
Another student showed her cheer,
“Different pharmacokinetics and routes of administration could keep our patients free of pains during 24 hours.” (SN13)
3.1.3.Skills of symptom control and comfort supply
Students shared their experiences of practising and demonstrating skills of caring for the dying in simulations.
A student praised the mini-simulation as a bridge,
“It was a good idea to make the theoretical learning close to practice.It was the first time I learned through simulations.Several times of mini-simulations gave me opportunities to try.It cut terminal symptoms into groups and eased my burden.I thought my brain would go blank if I met an overcomplicated case in the first simulation.” (SN11)
“After assessing his breath sound,I practised the routine that a nurse could do to relieve his dyspnea,from the posture adjustment,bronchodilators administration,oxygen supply,to breath practising.I felt less stressed because I would not hurt authentic dying patients.I knew nurse preceptors should give priority to patients than to students.I felt safe here because the tutor focused on me.”(SN12)
We taught students to transfer the nursing focus from curing to soothing.One student expressed better feelings when facing a terminal hepatic cancer patient,
“I accepted that the ascites could never be eliminated.However,I could measure his abdominal circumference,drainage ascites while closely monitoring his consciousness,care for the drainage catheter,encourage him to adjust his posture in bed,and make a careful diet plan with his family.” (SN3)
A student said,
“The course encouraged me because something else was worth a try besides the analgesics.Musical therapy,aromatherapy,and transcutaneous electrical nerve stimulation gave us optional choices.We are not alone.I am glad we can seek help from other specialists.” (SN9)
Ensuring cleanliness and comfort was important for terminal patients.One student said,
“Everyone likes clean and tidy,and I would not keep thinking about his death.I treated him as someone who needed clean and tidy,and this idea made me feel easier.” (SN1)
When we encouraged students to find methods to eliminate odour from the malignant wound,they suggested,
“We could suture a little bag,packaging some black tea,maybe coffee powder was also good.” (SN16)
Students regarded debriefing as valuable,
“Correcting was the core of moving forward.By tutor-guided debriefing,I recognized what I did correctly and incorrectly.”(SN10)
The student who role-played the nurse in the simulation scenario expressed her surprise,
“Showing complicated symptoms,surrounded by role-played families,the simulated scenario was realistic.Although extremely challenging,although not perfect,I used all I have learned to care for the dying!There still was a long way to go,but at least I took the first step.” (SN17)
3.1.4.Communication skills
Nurses worked under high pressure when caring for dying patients and their families.Appropriate communication was the key to high-quality hospice care.Communication practice went through mini-simulations and simulation scenarios.
“The worry about saying something wrong was why I kept silent before dying patients.I found it easier when facing a manikin because mistakes were allowed.” (SN11)
We trained research assistants to simulate dying patients with different personalities and guided students to understand patients’messages precisely.Students reported,
“Patients asked you expected questions about his disease,such as‘how long could I live?’Others sounded irrelevant,such as‘when will the typhoon come?I miss my childhood playing in the wild wind and downpouring rain during the No.8 Gale Signal!’ Now I knew both were talking about their reluctance to leave the world.”(SN7).
Students were trained to answer questions according to patients’ backgrounds.When facing a brave and highly educated patient,students were encouraged to take a franker attitude.
“I tried to discuss death affairs with the patient gradually.He gave me a good response,saying,‘finally,there was someone who could talk about the death with me.’” (SN12)
To comfort a Christian,a student said,
“I could strengthen her with the idea that she might be reunited with her dead husband.” (SN8)When in front of a patient with severe anxiety and depression,
“I think silent accompany was better than words,”one student said,“I would suggest to the doctor an anti-depression recipe.”(SN16)Many students concluded,“I would not be awkward or too worried because I could communicate with them.” (SN11)
We encouraged empathy by inviting students to play different roles:nurses,patients,and family members.The role-played nurse said,
“I merged into the situation,touching their sorrow from the deepest heart.” (SN3)
The student role-played the family member,saying,
“I have heard that families might be more painful than the dying one.Now I could not agree more.” (SN7)
The other student role-played the patient,saying,
“I will never say a sentence like‘do not cry,’or‘do not be sad,’to the patient.I knew such sentences were so pale and unhelpful to the dying one.” (SN6)
The observers who were not involved in the simulation scenarios said,
“The spectators see better than the players.In the eyes of a bystander,everything is clear and clean.” (SN1)
A student concluded confidently,
“The role-playing let me understand everyone in the dying situation.Suitable communication came from better understanding.”(SN9)
Students assumed the debriefing improved communications skills.
“In the debriefing,we discussed the dialogue in the scenario and found a better way for the nurse to answer the patient’s question.Thanks to the rerun simulation for allowing me to correct my wrong words.” (SN8)
One student added reran simulation as
“an opportunity to gain confidence,believing my competency to behave better.” (SN2)
3.2.Theme 2: Improving the ability to self-care and support colleagues
In addition to the ability to care for patients,participants recognized the importance of self-care and found ways to train themselves to become strong nurses.
3.2.1.Reflecting on life and death
We guided students to reflect on life and death,not just the patient’s death but also every person’s death.
“The most fundamental nature of death was un-avoidance,so we should not overburden ourselves by the unreal dream of saving all lives.Dying was the last stage when living was approaching death.Yes,it was always suffering.Hospice care was to relieve the suffering instead of stopping death.” (SN4)
“Acceptance of death cured me,caring for the dying with scientific methods and passional heart left me no regret.” (SN10)
Students reported,
“Witnessing patients’death made me sad.Their death reminded me of my death.How sad when I think I am going to die.” (SN8)
A student encouragingly said,
“I used to feel shame about my sadness of death.Now I knew no need to feel shame.I was a common human being needing to be consoled for death sadness.Caring for myself was of the same importance as caring for patients.I needed to handle this issue seriously,finding practical methods to care for myself.Although getting shared methods with the tutor,I thought doing exercise was more suitable for me because it could strengthen my body and mind.Strong nurses,although the same mortal as patients,could become the support for patients.” (SN13)
One student impressed the interviewer by saying,
“My future death and the patient’s impending death united us.The connection relieved my pain and encouraged me to serve the dying.” (SN17)
3.2.2.Sharing and supporting among colleagues
Students expressed appreciation for this program,allowing them to connect with colleagues.
“Arranging one’s death in advance was wise but weird when discussing with friends.I was glad I could talk about death in the debriefing with colleagues.” (SN2)
One student said,
“I like to hear about the tutor’s experience as an ICU nurse.It was touching and made me believe I would become a good nurse to comfort the dying in the future.Her sharing gave me hope to stand out from my clumsy.” (SN13)
One student said,
“Hearing classmates’ upsidedown,sadness,hesitation,and depression,I recognized I was not alone!As nursing students,we all struggled with the negative moods caused by hospice care.I felt better when sharing my feelings with colleagues under the same pressure.Sharing was a good method to alleviate anxiety.” (SN5)
Students emphasized the importance of sharing,
“Only if you would like to share,colleagues could recognize your difficulties.Colleagues were the most suitable ones to support you because they knew what you confronted in hospice care.” (SN14)
4.Discussion
This study provided a deep insight into the experiences of nursing undergraduates in the simulation-centred educational hospice program.The discussion was organized into two aspects:learning methods and learning outcomes.
4.1.Learning methods
The learning method is one of the decisive factors for learning outcomes.Participants described help from suitable learning methods in this program.They characterized the didactic lecture as an appropriate method to learn theoretical knowledge,especially mentioning that knowledge was the prerequisite for simulation.Participants praised mini-simulations which allowed them immediate application of learned knowledge.Although the minisimulation was not as complicated as the simulation scenario,students thought it gave them chances to try and get used to the simulation learning.Participants felt more challenges because of combined terminal symptoms and the existence of role-played families in simulation scenarios.They valued tutors’ feedback in debriefing on students’ performance in scenarios,including confirmations for rightness and corrections for wrongness.They claimed they gained confidence by trying again in the reran simulation.Participants presented that the debriefing was helpful in nurse-inward construction by sharing and supporting each other.
An integrative review [23] stated that a wide range of teaching strategies had been used in end-of-life care,resulting in students’positive changes.The authors found it unable to compare the effectiveness of each method because most included articles adopted multiple teaching methods and lacked intervention details.Few studies used the lecture as the only teaching method.Most included studies used minutes of lectures to prepare for other learning methods.We could not find clear descriptions of how and what students learned from didactic lectures.The published articles’focus was predominantly on simulations.The most important reform of our study was to use abundant theoretical lectures before simulation.The basic theory of hospice care was not the same as in medical-surgical nursing.By being equipped with the necessary theories,students could be ready for caring dying patients.Our participants’ experience confirmed this view.
Bodine [24] thought nurses’ hospice knowledge was weak because of insufficient education in their bachelor program,so she gave 8-h lectures,resulting in improved knowledge.She also compared two teaching strategies: 8-h lectures with 8-h lectures plus one simulation scenario.The study did not find statistical significance in knowledge between the two teaching strategies.This research shared the same view as our study that the simulation made students apply their newly acquired knowledge and skills in a safe environment.The simulations gave students the courage to practise.The author advocated that the simulation could help participants understand nurses’ role in the interdisciplinary hospice care team and promote professional communication.Our study found the same results participants found their improvements in knowledge and also knew when and from whom nurses should search for help to relieve patients’ terminal sufferings.
Tamaki et al.[3]used a random controlled trial to highlight the advantages of simulations by comparing conventional interventions,which included a lecture and four lessons of case study discussion.This study designed the simulation scenario as a terminal cancer patient,advocating that this method supplied students with safe and low-stress circumstances.Ruiz-Pellˊon's et al.[12]review concluded that simulation activities conveyed a feeling of safety and ease.These results were in line with our participants’experience.Because of the high vulnerability of dying patients,students feared their immaturity would cause irreversible harm.The simulation gave students chances to grow by trial and error safely.
Mini-simulations our participants greatly appreciated were the second reform in our study.One simulation may not be enough to improve students’ competency or attitude.Students need more practice to learn gradually.Changes took time,and students needed more practice opportunities.
Dreifuerst regarded debriefing as a crucial part of the simulation[25],and the same results were shared with our study.The researcher conducted the debriefing from a systematic process to release emotions and moved into a critical analysis of the simulation events.The debriefing in the present study was performed in a reverse direction.We debriefed students’ performance first,followed by reran simulation clips,and ended in sharing,supporting,and reflecting.Our participants commended the debriefing,which was grounded on the pragmatic level and sublimed to the metaphysical level,helping them practice nursing for dying patients and nurses’ self-psychological construction.We agreed that debriefing was an effective learning method for consolidating knowledge and skills.Similar results were found in Nunes’ study,recommending that researchers pay special consideration to help students process feelings and emotions [26].
4.2.Learning outcomes
The American Association of Colleges of Nursing (AACN) elaborates competencies of hospice care for undergraduate nursing students as 17 items[27].We sorted the 17 competencies into three aspects: society-connecting,patient-centred,and nurses-inward.Participants in the present study expressed their feelings of positive learning outcomes in the 17 competencies.Firstly,students said they mastered some special knowledge in hospice care,including the principles of this subject,the mechanism and management of terminal symptoms,and pharmacy.Our participants could clearly describe the social function of hospice care and understood the role of nurses as a bridge in the hospice care interdisciplinary professional team.They also expressed their perceived upgrade of skills in evaluating and controlling terminal symptoms,comfort supply,and communications.Secondly,participants mentioned increased confidence because of their improved competencies.Their anxiety was relieved when they understood that the core was to alleviate suffering,not save lives.Moreover,they expressed their pride in caring for the dyings,showing a positive attitude towards hospice care.Finally,they showed the ability to self-care during the pressure-provoking work and the willingness to share and support among colleagues.
Previous hospice educational studies found many positive learning outcomes assessed differently.Carmack et al.stated in her review that there was a wide range of quantitative assessing methods and qualitative descriptions for students’ learning outcomes [11].Most published articles showed positive learning outcomes.The most commonly used quantitative method was to assess changes in knowledge or attitude by scales.Nevertheless,the comparison was difficult because of the inconsistency of the different scales.Also,some studies used the rating by participants to show positive changes in perceived competencies and satisfaction with learning methods.For example,Lippe[15]used students’ratings to show elevated competence and attitude.Tamaki et al.[3]got participants’ positive learning outcomes considering their knowledge,skill performance,and self-confidence by knowledge scale,objective structured clinical evaluation exams,and self-rating questionnaire,respectively.
The qualitative outcomes,like learning experiences,expectations for future study,and beliefs about hospice care,were collected by open-ended questionnaires or interviews.For example,Fabro et al.[28] analyzed students’ reflection papers to describe their experiences during simulation learning.The qualitative description was good for educators to detect students’experiences and feelings during the learning process,which was why the present study took interviews to hear from participants.
Ruiz-Pellon et al.[12]included twelve qualitative and five mixed methods studies to conduct a systematic review and qualitative meta-synthesis.The 17 articles were about students’experiences in end-of-life education programs.Three themes emerged: feelings and emotions,end-of-life education,and competencies acquired.The reviewers grouped all participants’ emotions and feelings.When facing dying/death in the pedagogical activities,students expressed helplessness,anger,disbelief,and special difficulties when facing families.Our participants rarely expressed such unfavorable feelings.Instead,they voiced cheer when they could do something for the dying and were less awkward when they could properly communicate.This result may indicate gained competencies could decrease students'’ negative feelings about hospice care.Ruiz-Pellon et al.[12] emphasized the importance of communication skills,sharing the same results with us in students’improved communication when facing patients,families,and other medical staff.
4.3.Limitation
We only collected data one time and did not ensure the dependability by showing the data’s stability over time,which presented another limitation.The research was conducted under the unique inter-culture background of Macao,China which may limit the generalization of the results from this study.
5.Conclusion
The study aimed to explore how nursing undergraduates experienced a simulation-centred educational program in hospice care.Students reported good learning experiences with the learning methods.Didactic lectures equipped them with the necessary knowledge,mini-simulations allowed them immediate application of knowledge,simulation scenarios gave them a whole picture about a dying/death situation,and debriefing helped them in self-care and colleague support.
Students reported improved hospice competency.They could care for the dying and families with more knowledge,better symptom control and comfort supply,and more appropriate communication.Their understanding of the principle of hospice care and acceptance of the mortal fate of human beings helped them become more robust nurses.
6.Recommendation
Besides the quantitative results from the educators’perspective,more students’ voices should be heard in hospice care learning.Although the effectiveness has been confirmed,more consideration should be taken to make the simulation method more rational and refined.
CRediT authorship contribution statement
Wang Yan:Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Writing -original draft,Funding acquisition.Yuan Haobin: Methodology,Formal analysis,Investigation,Data curation,Writing -review&editing.
Funding
This research received the sponsor from the Academic Research Funding of Macao Polytechnic University(No.RP/ESS 02/2018).
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to thank all participants in the study for sharing their valuable information and feelings.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.09.005.
 International Journal of Nursing Sciences2022年4期
International Journal of Nursing Sciences2022年4期
- International Journal of Nursing Sciences的其它文章
- Effects of equine-assisted interventions on older adults’ health: A systematic review
- Nurses’ experiences of caring for preterm infants in pain: A metaethnography
- Mothers overcoming remorse to care for self and baby: An emerging concept
- Development and validation of the Nurse’s Workplace Mental Health Questionnaire
- A comprehensive health education plus monitoring support program for older adults with knee osteoarthritis coexisting with overweight and type 2 diabetes
- Nursing students’ knowledge and attitude toward diabetic ulcer care and their contributing factors in Indonesia
