Timing of endoscopic retrograde cholangiopancreatography in the treatment of acute cholangitis of different severity
Yao-Chi Huang, Chi-Huan Wu, Mu Hsien Lee, Sheng Fu Wang, Yung-Kuan Tsou, Cheng-Hui Lin, Kai-FengSung,Nai-Jen Liu
Abstract
Key Words: Acute cholangitis; Endoscopic retrograde cholangiopancreatography; severity; Timing; Thirtyday mortality; Length of hospital stay
lNTRODUCTlON
Without treatment, patients with acute cholangitis (AC) may progress to septicemia and organ failure resulting in mortality[1,2]. Over the past two decades, endoscopic retrograde cholangiopancreatography(ERCP) has been generally accepted as a first-line treatment for AC[3,4]. Although delayed biliary drainage may not affect the risk of complications in patients who respond well to antibiotics, some patients with AC require early ERCP to avoid (persistent) organ failure or mortality[2,5,6]. Despite consensus on the need for biliary drainage, the optimal timing for early ERCP remains unclear due to mixed results in the literature[7]. Different definitions of early ERCP have been used in the literature,ranging from 12 h to 72 h[2,5,8-11]. The varied definitions among studies have led to inconsistent conclusions. In addition, the definitions of AC are not uniform across studies. More importantly, most studies did not define the timing of ERCP by stratifying the severity of AC[7]. In this context, the recently published Tokyo Guidelines 2018 (TG18) provide not only a diagnosis of AC but also a severity grading, which is important for predicting prognosis and determining treatment strategies[3]. However,although TG18 recommends early or urgent biliary drainage for moderate or severe cholangitis, there is no specific timing for early or urgent ERCP. Therefore, this study aims to investigate whether the timing of ERCP is associated with improved outcomes in AC patients with different severities.
MATERlALS AND METHODS
This was a retrospective study conducted at Chang Gung Memorial Hospital Linkou Center. At our center, ERCP has been the first-line of treatment for patients with AC for the past two decades. This study was reviewed and approved by the Ethics Committee of the Chang Gung Memorial Hospital (IRB No. 202200881B0). Since this was a retrospective study using routine clinical treatment or diagnostic medical records, the Chang Gung Medical Foundation Institutional Review Board approved the waiver of the participant's consent. All methods were carried out under relevant guidelines and regulations.
Definition of acute cholangitis
The diagnostic criteria for AC were based on the 2018 Tokyo Guidelines, including systemic inflammation, cholestasis and imaging findings[3]. Systemic inflammation included fever (body temperature >38 °C) or evidence of an inflammatory response [white blood cell (WBC) count < 4000 or > 10000/µL or C-reactive protein ≥ 1 mg/dL]. Cholestasis included jaundice (serum total bilirubin ≥ 2 mg/dL) or abnormal liver function tests (serum alkaline phosphatase, r-glutamyl transferase, aspartate aminotransferase, or alanine aminotransferase > 1.5 times the upper limit of the normal value). Imaging findings included bile duct dilatation or imaging evidence of etiology such as strictures, stones or stents. A definite diagnosis of AC was defined as one item in systemic inflammation, one item in cholestasis and one item in imaging findings.
Definition of the severity of acute cholangitis
AC severity was divided into three grades based on the 2018 Tokyo Guidelines[3]. Grade III (severe) AC was AC associated with the onset of dysfunction in at least one of the following organs/systems:cardiovascular dysfunction (defined as hypotension requiring dopamine ≥ 5 µg/kg per min, or any dose of norepinephrine), neurological dysfunction (presence of conscious disturbance), respiratory dysfunction (defined as PaO2/FiO2ratio < 300), renal dysfunction (oliguria, serum creatinine > 2.0 mg/dL), hepatic dysfunction [defined as prothrombin time-international normalized ratio (PT-INR) >1.5] or hematological dysfunction (defined as platelet count < 100 × 103/µL). Grade II (moderate) AC was AC associated with any two of the following conditions: abnormal WBC count (> 12000/µL or <4000/µL), high fever (≥ 39 °C), old age (≥ 75 years), hyperbilirubinemia (serum total bilirubin ≥ 5 mg/dL), or hypoalbuminemia (< lower limit of normal value × 0.7). Grade I (mild) AC was AC that did not meet the criteria of “Grade III” or “Grade II” AC at initial diagnosis.
Definition of time to ERCP
Time to ERCP was defined as the time from the emergency department visit to the commencement of ERCP.
Patient selection and clinical variables
The study flow chart is shown in Figure 1. Between 2016 and 2017, 2121 patients who underwent ERCP in our center were retrospectively collected from the computer database of the Therapeutic Endoscopy Center. The inclusion criteria were patients who met the TG18/TG13 criteria for a definite diagnosis of AC. The exclusion criteria were: (1) Patients who did not meet the criteria for a definite diagnosis of AC;(2) inpatients who developed AC after hospitalization; and (3) patients who received ERCP 7 or more days after an emergency department visit. For patients readmitted for AC during the study period, we included only the first admission and the ERCP procedure.
Medical records were reviewed, and the following data were obtained: sex; age; clinical manifestations, including body temperature, systolic blood pressure, heart rate, saturation, respiratory rate and urine output; laboratory values including WBC count, platelet count, PT-INR, C-reactive protein,creatinine, bilirubin, alkaline phosphatase, r-glutamyl transferase, aspartate aminotransferase, alanine aminotransferase and albumin; diagnosis and treatment of ERCP, including causes of obstruction (such as stones, malignant strictures or stent dysfunction); and the timing of ERCP.
Outcome assessments
The primary outcome was 30-d mortality. Secondary outcomes were ICU admission rate, length of hospital stay (LOHS) and 30-d readmission rate. The results were first compared for patients receiving ERCP ≤ 24 hvs> 24 h and then for patients receiving ERCP ≤ 48 hvs> 48 h. Subgroup analyses were also performed in patients with grade I, II, and III AC.
Statistical analysis
Continuous variable data are represented by the median and interquartile range (IQR); categorical variables are presented as a number (%). For comparisons, the Kruskal-Wallis test was used for continuous variable data and the chi-square test or Fisher’s exact test was used for suitable categorical variables. Logistic regression analysis was performed to identify factors associated with 30-d mortality.Only variables with aPvalue < 0.05 in the univariate analysis were included in the multivariate analysis. Two-tailedPvalues < 0.05 were considered statistically significant andPvalues = 0.05 were considered marginally significant. Statistical analysis was performed using SPSS software (version 22.0;SPSS, Inc., Chicago, IL, United States).

Figure 1 Study flow chart. AC: Acute cholangitis; ERCP: Endoscopic retrograde cholangiopancreatography.
RESULTS
A total of 683 patients who met the eligibility criteria were included in the study. Among them, there were 170 (24.9%) grade III AC patients, 179 grade II AC patients (26.4%) and 334 grade I AC patients(48.9%).
Patient characteristics
The baseline characteristics of the patients are presented in Table 1. The median (IQR) age of the patients was 66 (53-78) years; 57.2% were male. The median body temperature was 37.5 (36.8-38.4) °C and 58.4% of patients had abnormal WBC counts. The median platelet count was 198 × 103(148 × 103-251× 103)/µL. The median serum levels of aspartate aminotransferase, alanine aminotransferase and alkaline phosphatase were 150 U/L, 166 U/L and 265 U/L, respectively. Serum amylase and lipase data were available for 307 (44.9%) and 487 (71.3%) patients with median levels of 65 U/L and 37 U/L,respectively. The median serum bilirubin level was 3.7 (2.3-6.3) mg/dL and the median creatine level was 0.93 (0.73-1.24) mg/dL. The median PT/INR was 1.1 (1.1-1.2). Only 133 (19.5%) patients had data on serum albumin and the median level was 3.56 (3.05-3.98) g/dL. Twenty-nine (4.2%) patients had cardiovascular dysfunction, 35 (5.1%) patients had neurological dysfunction and 48 (7%) patients had respiratory dysfunction.
Comparisons between ERCP ≤ 24 h and ERCP > 24 h:Compared with ERCP > 24 h, patients with ERCP ≤ 24 h had significantly lower body temperature (median, 37.2 °Cvs37.5 °C.P= 0.003),significantly higher serum alanine aminotransferase (median, 194 U/Lvs156 U/L,P= 0.02) and serum creatinine levels (median, 0.96vs0.93,P= 0.004), and significantly higher proportions of abnormal WBC counts (70.9%vs55.4%,P= 0.001), cardiovascular dysfunction (11.2%vs2.6%,P< 0.001) and respiratory dysfunction (14.2%vs5.3%,P< 0.001).
Comparisons between ERCP ≤ 48 h and ERCP > 48 h:Compared with ERCP > 48 h, patients with ERCP ≤ 48 h had significantly lower body temperature (median, 37.4 °Cvs37.6 °C,P= 0.009),significantly higher serum alanine aminotransferase levels (median, 188 U/Lvs142 U/L,P= 0.004) and significantly lower PT/INR (median, 1.1vs1.2,P= 0.001).
ERCP characteristics and causes of AC
The characteristics of ERCP are listed in Table 2. Causes of AC included common bile duct stones(CBDS, 74.4%), malignant biliary obstruction (MBO, 10.2%), biliary stent dysfunction (8.9%), benign biliary stricture (4.5%) and others (1.9%). ERCP failed in 1% of patients. For patients with successful ERCP, endoscopic treatments during ERCP included endoscopic sphincterotomy (81.7%), endoscopic papillary balloon dilatation (0.7%), bile duct stone retrieval (73.5%), stone-free bile duct clearance (5.4%),removal of old biliary stents (8.8%), insertion of new biliary stents (27.4%), dilation of biliary strictures(1%) and others (0.4%).
Comparisons between ERCP ≤ 24 h and ERCP > 24 h:The median time to ERCP was 17.7 (9.0-20.4) h in the ERCP ≤ 24 h group and 67.6 (43.6-98.9) h in the ERCP > 24 h group. Only malignant biliary obstruction as a cause of AC was significantly less common in the ERCP ≤ 24 h group (5.2%vs11.5%,P= 0.032). In therapeutic ERCP, bile duct stone retrieval was higher in the ERCP ≤ 24 h group (80.6%vs71.8%,P= 0.038) whereas the old biliary stent removal rate was lower (4.5%vs9.8%,P= 0.049).
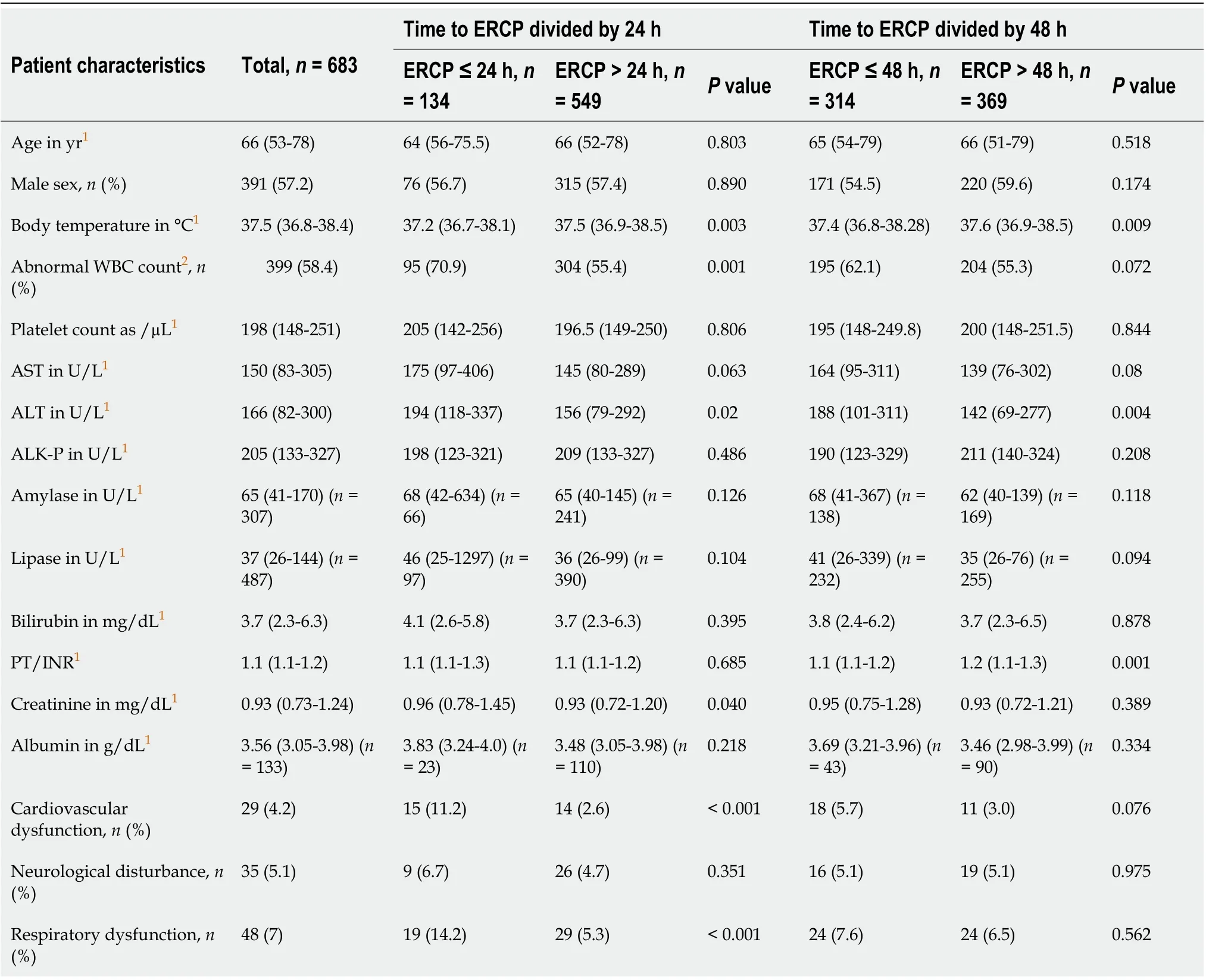
Table 1 Characteristics of the patients
Comparisons between ERCP ≤ 48 h and ERCP > 48 h:The median time to ERCP was 26.0 (18.8-40.1) h in the ERCP ≤ 48 h group and 88.5 (67.2-114.6) h in the ERCP > 48 h group. Regarding indications for ERCP, CBDS was more common in the ERCP ≤ 48 h group (81.5%vs68.3%,P< 0.001) whereas malignant biliary obstruction (6.1%vs13.8%,P< 0.001) and stent dysfunction were less common (5.4%vs11.9%,P= 0.003). In therapeutic ERCP, endoscopic sphincterotomy (85.7%vs78.3%,P= 0.013) and bile duct stone retrieval (79.6%vs68.3%,P= 0.001) were more frequent in the ERCP ≤ 48 h group whereas the removal of old biliary stents (5.4%vs11.7%,P= 0.004) and the insertion of new biliary stents (22.3%vs31.7%,P= 0.006) were less frequent.
Primary and secondary outcomes
The primary and secondary outcomes are summarized in Table 3.
Overall patients:Overall, the 30-d mortality rate was 1.02% (or 7/683). The ICU admission rate was 5.4%; the median LOHS was 7 (5-10) d; and the 30-d readmission rate was 12.7%.
(1) Comparisons between ERCP ≤ 24 h and ERCP > 24 h: The overall 30-d mortality rate was 0 in the ERCP ≤ 24 h group and 1.3% in the ERCP > 24 h group. However, the difference did not reach statistical significance (P= 0.356). Regarding secondary outcomes, the ERCP ≤ 24 h group had significantly higher ICU admission rates (11.2%vs4.0%,P= 0.001) and shorter LOHS (median, 6 dvs7 d,P= 0.018).
(2) Comparisons between ERCP ≤ 48 h and ERCP > 48 h: Overall, the 30-d mortality rate was significantly lower in the ERCP ≤ 48 h group than in the ERCP > 48 h group (0vs1.9%,P= 0.017). For secondary outcomes, the ERCP ≤ 48 h group had a significantly shorter LOHS (median, 6 dvs8 d,P<0.001).
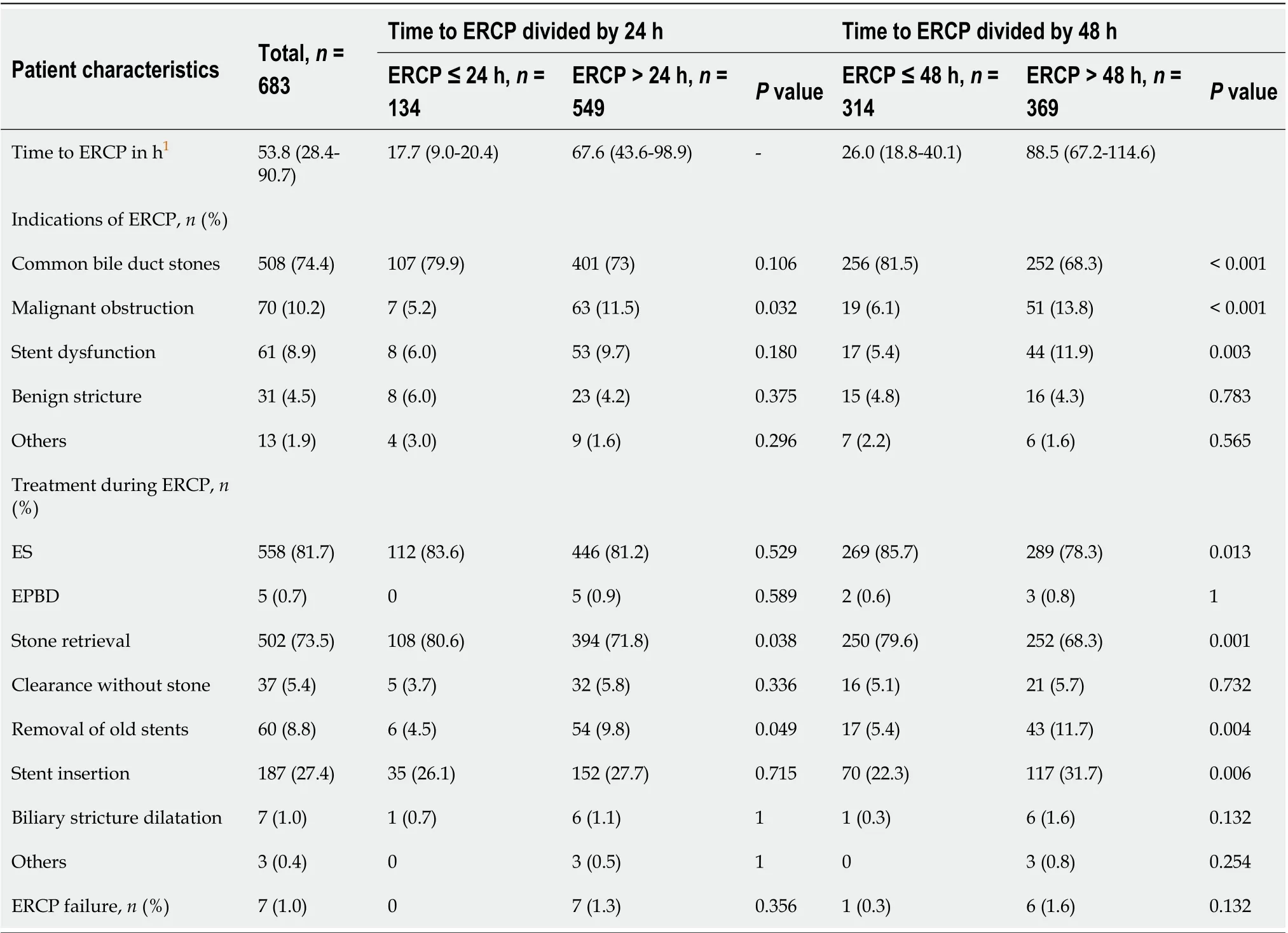
Table 2 Characteristics of endoscopic retrograde cholangiopancreatography
Patients with Grade III AC:The 30-d mortality rate was 3.5% (or 6/170) for patients with grade III AC.The ICU admission rate was 15.3%; the median LOHS was 7 (7-14) d; and the 30-d readmission rate was 13.5% in this patient group.
(1) Comparisons between ERCP ≤ 24 h and ERCP > 24 h: The 30-d mortality rate for grade III AC patients was 0 in the ERCP ≤ 24 h group and 4.6% in the ERCP > 24 h group. However, the difference did not reach statistical significance (P= 0.338). Regarding secondary outcomes, the ERCP ≤ 24 h group had significantly higher ICU admission rates (9.0%vs2.6%,P= 0.002).
(2) Comparisons between ERCP ≤ 48 h and ERCP > 48 h: Among grade III AC patients, the 30-d mortality rate was significantly lower in the ERCP ≤ 48 h group than in the ERCP > 48 h group (0vs6.1%,P= 0.039). Regarding secondary outcomes, the ERCP ≤ 48 h group had significantly higher ICU admission rates (22.2%vs10.2%,P= 0.031).
Patients with Grade II AC:The 30-d mortality rate was 0 for patients with grade II AC. The ICU admission rate was 2.8%; the median LOHS was 7 (5-10) d; and the 30-d readmission rate was 13.4% in this patient group.
(1) Comparisons between ERCP ≤ 24 h and ERCP > 24 h: The only significant finding in grade II AC patients was that the LOHS was shorter (median, 6 dvs7 d,P= 0.047) in the ERCP ≤ 24 h group.
(2) Comparisons between ERCP ≤ 48 h and ERCP > 48 h: Among grade II AC patients, the only significant finding was that the LOHS was shorter (median, 6 dvs8 d,P= 0.001) in the ERCP ≤ 48 h group.
Patients with Grade I AC:The 30-d mortality rate was 0.3% (or 1/334) for patients with grade I AC. The ICU admission rate was 1.8%; the median LOHS was 6 (5-9) d; and the 30-d readmission rate was 12% in this patient group.
(1) Comparisons between ERCP ≤ 24 h and ERCP > 24 h: The only significant finding in grade I AC patients was that the LOHS was shorter (median, 6 dvs7 d,P= 0.005) in the ERCP ≤ 24 h group.

Table 3 Primary and secondary outcomes
(2) Comparisons between ERCP ≤ 48 h and ERCP > 48 h: Among grade I AC patients, the only significant finding was that the LOHS was shorter (median, 6 dvs7 d,P< 0.001) in the ERCP ≤ 48 h group.
Factors associated with 30-d mortality
The results of the univariate and multivariate analyses are listed in Table 4. The univariate analysis revealed that malignant biliary obstruction (OR: 6.817, 95%CI: 1.494-31.109,P= 0.013), hepatic dysfunction (OR: 8.896, 95%CI: 1.645-48.119,P= 0.011), respiratory dysfunction (OR: 10.517, 95%CI:2.284-48.431,P= 0.003), neurological dysfunction (OR: 15.094, 95%CI: 3.241-70.298,P= 0.001),cardiovascular dysfunction (OR: 18.750, 95%CI: 3.990-88.112,P< 0.001), severity of AC (severevsmoderate + mild, OR: 18.732, 95%CI: 2.239-156.728,P= 0.007), ICU admission (OR: 7.326, 95%CI: 1.373-39.101,P= 0.02), and time to ERCP (every 1-d delay, OR: 1.950, 95%CI: 1.252-3.038,P= 0.003) were associated with 30-d mortality. The multivariate analysis revealed that time to ERCP (every 1-d delay,OR: 2.081, 95%CI: 1.154-3.753,P= 0.015) was the only independent factor associated with 30-d mortality.However, cardiovascular dysfunction (OR: 17.756, 95%CI: 0.994-317.241,P= 0.050) was of marginal significance.
DlSCUSSlON
Kiriyamaet al[3] reported that early or urgent ERCP significantly reduced 30-d mortality only in patients with grade II AC compared with patients who did not receive early or urgent ERCP. This result may be due to the lack of well-defined timing for early or urgent ERCP. In a meta-analysis published in 2020, Duet al[7] reported that early ERCP reduced in-hospital mortality regardless of whether it was defined as < 24 h, < 48 h or < 72 h. In the present study, we found that ERCP ≤ 48 h but not ERCP ≤ 24 hsignificantly reduced 30-d mortality. Our results were consistent with the 2021 American Society for Gastrointestinal Endoscopy guidelines recommending ERCP ≤ 48 h in AC patients[12]. In that study,however, the data were insufficient to stratify by disease severity. In a subgroup analysis, we found that the same survival benefit was observed only in patients with grade III AC but not in patients with grade II or I AC. These results were because patients with grade III AC had significantly higher 30-d mortality than those with grade II or I AC (3.5%vs0vs0.3%,P= 0.001). Hakutaet al[10] reported that time to ERCP was not associated with clinical outcomes (including in-hospital mortality) in patients with nongrade III AC. Therefore, we recommend emergent ERCP (≤ 48 h) for patients with grade III AC in terms of survival benefit.
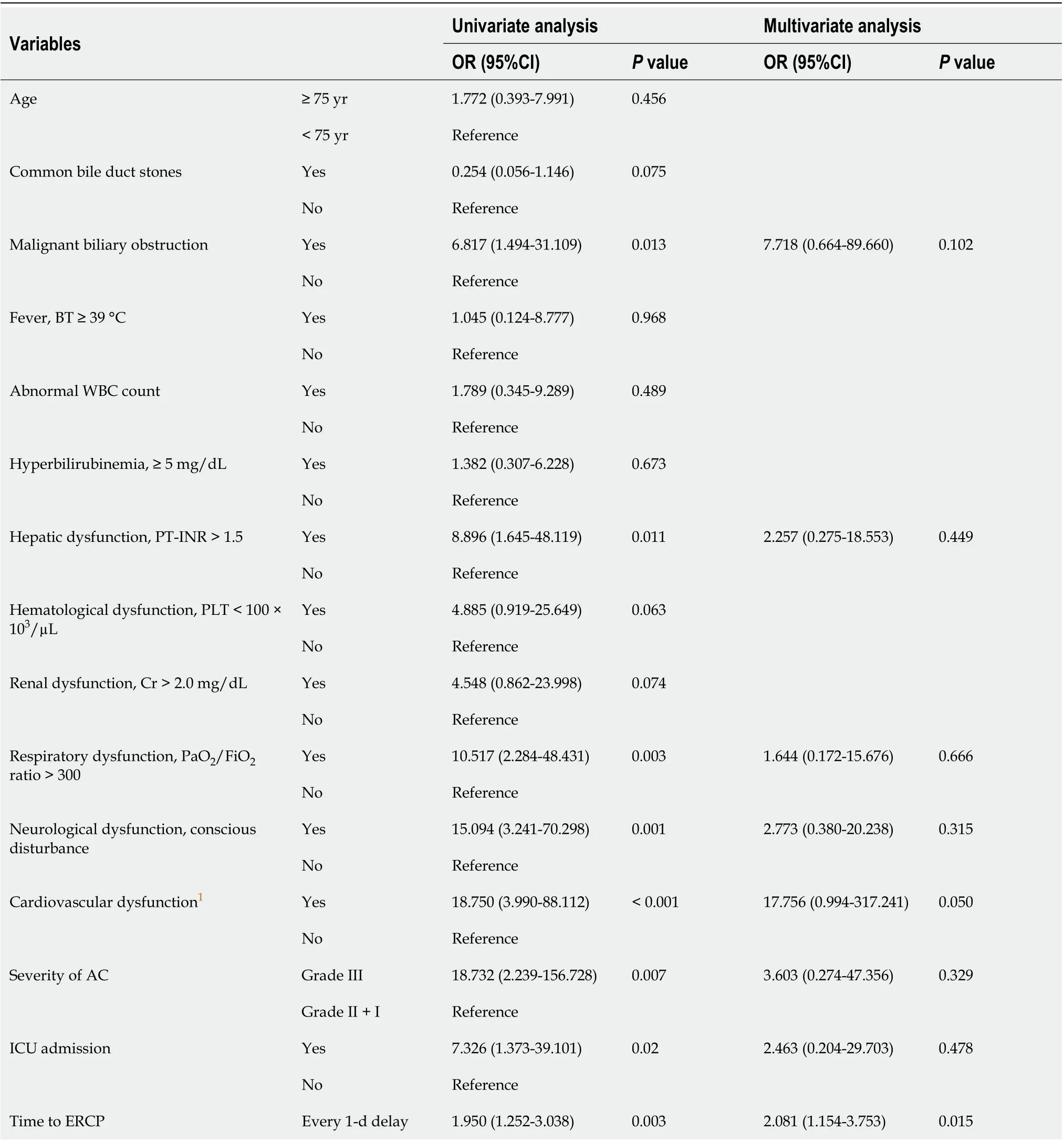
Table 4 Univariate and multivariate analyses of the factors associated with 30-d mortality
However, 30-d mortality in AC has been reported to range from 1% to 16% between studies, which may be one of the reasons leading to inconsistent conclusions about the optimal timing of ERCP[11,13-15]. Differences in mortality may be due to different patient populations in different studies,e.g.,patients with AC due to CBDS and MBO may have different clinical courses and prognoses. Kiriyamaet al[14] reported that patients with AC associated with MBO had a higher 30-d mortality rate than those with AC associated with CBDS. In our univariate analysis, MBO was a factor associated with 30-d mortality. Therefore, one of the reasons for the low 30-d mortality in our study was the low proportion of patients with MBO (10.2%). In contrast, Tanet al[11] included 43% of MBO patients in their study and reported a 30-d mortality rate of 16%. However, Parket al[15] included only patients with AC associated with distal MBO and reported an overall 30-d mortality rate of 4.8%. Therefore, there may be some other factors associated with 30-d mortality between studies.
Of the five organ failure criteria used to diagnose grade III AC, cardiovascular dysfunction was the only independent factor associated with 30-d mortality in the current study. Therefore, among grade III AC patients, those with cardiovascular dysfunction may need to be treated differently[16,17]. Karvellaset al[17] reported an overall mortality rate of 37% in 260 patients with AC-related septic shock. They found that delayed biliary decompression > 12 h from the onset of shock was one of three independent factors associated with mortality. The 2019 European Society of Gastrointestinal Endoscopy guidelines recommend biliary drainage (preferably endoscopic) within 12 h of shock onset for AC patients with CBDS-related septic shock[16]. Therefore, cardiovascular dysfunction should be weighed when developing new guidelines in the future.
Some studies found no survival benefit but did find early ERCP to reduce the LOHS[18-21]. Houet al[20] reported that in a multivariate analysis, the LOHS increased by 1.44 d for every 1-d delay in ERCP (P< 0.001). Similar results were seen in the study by Zhuet al[18]: LOHS increased by 1.49 d for every 1-d delay in biliary drainage (P< 0.0001). However, these findings were not stratified by disease severity.Although we did not perform a multivariate analysis of the LOHS, our results suggested that the LOHS could be significantly reduced regardless of ERCP ≤ 24 h or ≤ 48 h. In subgroup analyses stratified by disease severity, this benefit was only observed in patients with grade I or II AC. The benefit of early ERCP in shortening the LOHS might be offset by higher ICU admission rates in grade III AC patients.Similar findings were found by Janget al[19], who recommended urgent ERCP (≤ 24 h) for patients with grade I or II AC because it can shorten the LOHS.
This study has several limitations. First, this retrospective, single-center study might have inherent selection bias. Patients with cardiovascular dysfunction and respiratory dysfunction tended to receive ERCP ≤ 24 h. Therefore, caution is required when interpreting the results of this subgroup analysis.Second, we identified patients from the endoscopy database. AC patients who died before receiving ERCP might not have been included in this study, resulting in an underestimation of 30-d mortality.Third, data on albumin, one of the criteria for class II AC, were available in only 19.5% of patients.Therefore, some patients with grade II AC may be misclassified as grade I AC and vice versa.
CONCLUSlON
ERCP ≤ 48 h but not ≤ 24 h has a survival benefit in AC patients; this benefit is only observed in patients with grade III AC. Early ERCP is also recommended for patients with grade I or II AC because it shortens the LOHS.
ARTlCLE HlGHLlGHTS
Research methods
The retrospective cohort study included 683 patients who met the diagnostic criteria for acute cholangitis defined by the 2018 Tokyo Guidelines. Among them, there were 170 (24.9%) grade III acute cholangitis patients, 179 grade II acute cholangitis patients (26.4%) and 334 grade I acute cholangitis patients (48.9%). Results are first compared between patients receiving ERCP ≤ 24 h and > 24 h, and then between patients receiving ERCP ≤ 48 h and > 48 h. Subgroup analyses are performed on patients with grade III, II or I acute cholangitis.
Research results
When 24 h was considered a critical value for ERCP timing, we found that patients with malignant biliary obstruction received ERCP ≤ 24 h less frequently when compared with ERCP > 24 h (5.2%vs11.5%). Patients with organ dysfunction such as cardiovascular dysfunction (11.2%vs2.6%) and respiratory dysfunction (14.2%vs5.3%) or those admitted to the ICU (11.2%vs4%) tended to receive ERCP ≤ 24 h. Patients with ERCP ≤ 24 h had significantly shorter hospital stays (median, 6 dvs7 d).Stratified by the severity of acute cholangitis, higher ICU admission was only observed in grade III acute cholangitis and a shorter length of hospital stay was only observed in grade I and II acute cholangitis. Regarding 30-d mortality, the results of ERCP ≤ 24 h and > 24 h were not significantly different, either in the overall population or in patients with grade I, II or III acute cholangitis. When 48 h was considered a critical value for ERCP timing, patients with choledocholithiasis received ERCP ≤ 48 h more frequently (81.5%vs68.3%). Patients who received ERCP ≤ 48 h had significantly lower 30-d mortality (0vs1.9%) and shorter hospital stays (6 dvs8 d). Stratified by the severity of acute cholangitis,lower 30-d mortality (0vs6.1%) and higher ICU admission rates (22.2%vs10.2%) were only observed in grade III acute cholangitis and a shorter length of hospital stay was only observed in grade I and II acute cholangitis. In the multivariate analysis, cardiovascular dysfunction and time to ERCP were two independent factors associated with 30-d mortality.
Research conclusions
ERCP ≤ 48 h but not ≤ 24 h has a survival benefit in acute cholangitis patients; this benefit is only observed in patients with grade III acute cholangitis. Early ERCP is also recommended for patients with grade I and II acute cholangitis because it shortens the length of hospital stay.
Research perspectives
Of the five organ failure criteria used to diagnose grade III AC, cardiovascular dysfunction was the only independent factor associated with 30-d mortality in the current study. Therefore, cardiovascular dysfunction should be weighed more heavily in the development of new guidelines in the future.
FOOTNOTES
Author contributions:Huang YC contributed to the conceptualization of the study and original manuscript; Wu CH,Lee MH and Wang SF contributed to data planning, interpretation and formal analysis; Lin CH and Sung KF contributed to data collection; Tsou YK is committed to the conceptualization of the study, manuscript writing,review and editing; Liu NJ contributed to revising the final version of the manuscript for submission.
lnstitutional review board statement:This study was reviewed and approved by the Ethics Committee of the Chang Gung Memorial Hospital (IRB No. 202200881B0).
lnformed consent statement:Since this was a retrospective study using clinical routine treatment or diagnostic medical records, the Chang Gung Medical Foundation Institutional Review Board approved the waiver of the participant's consent.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:Technical appendix, statistical code and dataset available from the corresponding author at flying@adm.cgmh.org.tw.
STROBE statement:The authors have read the STROBE Statement-checklist of items, and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Taiwan
ORClD number:Chi-Huan Wu 0000-0002-3913-8010; Mu Hsien Lee 0000-0003-3664-5313; Sheng Fu Wang 0000-0002-7856-2957; Yung-Kuan Tsou 0000-0002-7254-7369; Cheng-Hui Lin 0000-0001-8102-0625; Kai-Feng Sung 0000-0001-6118-0234;Nai-Jen Liu 0000-0002-7992-0234.
S-Editor:Gong ZM
L-Editor:Filipodia
P-Editor:Gong ZM
 World Journal of Gastroenterology2022年38期
World Journal of Gastroenterology2022年38期
- World Journal of Gastroenterology的其它文章
- Ultrasound-based artificial intelligence in gastroenterology and hepatology
- Comparison of evaluation indexes for Gastroenterology and Hepatology journals in different databases
- A new scoring system to evaluate adjuvant chemotherapy for patients with T2N0M0 gastric cancer after D2 gastrectomy
- Effect of low-dose radiation on thyroid function and the gut microbiota
- Oxidative stress bridges the gut microbiota and the occurrence of frailty syndrome
- Red blood cell distribution width derivatives in alcohol-related liver cirrhosis and metabolic-associated fatty liver disease
