Culture-positive urinary tract infection following micturating cystourethrogram in children
Simon Ngwso *,Munyrzi Nynoro ,Ttn Nznz ,Ting Yi Chow ,Fion Bttny ,Anrw Brkr ,Jpinr Khos ,Nm Smnky ,f
a Fiona Stanley Hospital.Murdoch,Western Australia,Australia
b Young Urology Researchers Organisation,Melbourne,Australia
c Austin Hospital,Heidelberg,Victoria,Australia
d Royal Perth Hospital,Perth,Western Australia,Australia
e Princess Margaret Hospital,Subiaco,Western Australia,Australia
f School of Medicine,University of Western Australia,Dalkeith,Western Australia,Australia
KEYWORDS Micturating cystourethrogram;Voiding cystourethrogram;Paediatric urology;Functional urology
Abstract Objective:To determine the incidence of culture-positive urinary tract infection(UTI)after micturating cystourethrogram(MCUG).We further wanted to identify risk factors for developing a culture-positive UTI following MCUG.
1.Introduction
Micturating cystourethrogram(MCUG)is a fluoroscopic investigation performed to investigate the anatomy and function of the lower urinary tract system[1].MCUG is commonly performed in paediatric patients for evaluating a range of urological conditions with structural and neurogenic aetiology,such as investigation of hydronephrosis,hydroureter,or bladder status in children with spina bifida.MCUG is the gold standard test to assess for the presence and severity of vesicoureteric reflux(VUR)after urinary tract infection(UTI)[1].Following UTI,30% to 40% of children will have VUR detected on MCUG[2].MCUG is recommended by the National Institute for Health and Care Excellence(NICE),American Academy of Pediatrics,and the Royal Australasian College of General Practitioners for the investigation of atypical and recurrent UTI in children[3-5].
There are few published articles addressing the risk of developing UTI after MCUG.However,it is widely believed by clinicians,patients,and parents of patients that MCUG may increase the risk of UTI and/or urosepsis[6-8].This concern may result in a reluctance to investigate with a MCUG when clinically indicated.It is important to ensure paediatric patients obtain timely investigation of suspected urological pathology to reduce delays in management and optimise treatment outcomes.Specifically,in regards to investigation of UTI,delay in timely and appropriate investigation has been associated with poorer compliance with follow-up[9,10].
The purpose of this study was to determine what the actual incidence of culture-positive UTI after MCUG is in an Australasian paediatric hospital setting.We further assessed risk factors for developing culture-positive UTI following MCUG.To the authors’knowledge,this is the first study conducted in Australia addressing UTI risk after MCUG in children.
2.Patients and methods
A retrospective review of patients who underwent MCUG at Princess Margaret Hospital(PMH)in Perth,Western Australia,Australia was performed.PMH is the sole tertiary paediatric hospital in the state of Western Australia.At PMH,MCUG is performed in the radiology fluoroscopy suite using a standardised technique.The genitalia was prepped with povidone-iodine solution prior to insertion of an appropriately sized urinary catheter for age and weight,followed by instillation of a sterile solution containing urografin contrast.Patients were not routinely administered prophylactic antibiotics prior to the procedure;however,patients already taking prophylactic antibiotics continued their current prophylactic regimen.A urinalysis was performed prior to commencing the MCUG.Patients who had evidence of concurrent UTI did not proceed with the MCUG.
Five hundred sequential patients who had the procedure performed between January 2013 to December 2014 were selected with no exclusion criteria.Patient demographics,indication for MCUG,and number of pre-MCUG and post-MCUG culture-positive UTIs were recorded.The protocol and procedure for performing MCUG has not changed since 2013.
The medical records of all patients who underwent MCUG and developed culture-positive UTI within 14 days following the procedure were reviewed to determine why their urine was checked after MCUG,whether the UTI was a febrile UTI,if they required hospital admission,and whether oral or intravenous antibiotics were used.
Data were analysed using SPSS™Version 24(IBM.Armonk,New York,NY,USA).Descriptive statistics were used to describe the demographic characteristics of the cohort.Univariate analysis was conducted to test whether there was an association between post MCUG culture-positive UTI and specific independent variables.An alpha level of 0.05 was used for all statistical tests.The Chi-square value,degrees of freedom,and asymptotic significance(2-sided)were reported.Multivariate binary logistic regression was used to model the odds of post MCUG culture positive UTI while adjusting for potential confounders,such as age group,gender,procedure location,neurogenic bladder,history of pre-procedure UTI,known VUR,upper renal tract anatomical anomaly,and antenatal hydronephrosis.The independent variables selected to be included in the regression model were consistent with current literature reporting.
3.Results
A total of 44.8% of patients were female and 56.2% of patients who underwent MCUG were performed in patients at 0-6 months of age(56.2%).The most common indication for MCUG was further investigated following UTI(47.0%).Some patients had multiple indications for having MCUG performed(Table 1).
A total of 206(41.2%)patients who underwent MCUG had a previous culture-positive UTI,with Escherichia coli being the most common pathogen cultured(24.4%)(Table 2).
In our study cohort,52(10.4%)patients had a formal urine sample sent for analysis within 14 days following MCUG.Of the 52 patients who had their urine checked,28(5.6% of total population)had culture-positive UTI;however,only 13(2.6% of total population)had their urine checked after presenting with urinary tract symptoms.Seven patients(1.4%,comprised of four females and three males)presented with urinary symptoms and were also febrile(Table 3).All urines collected were obtained as a clean catch or a catheter specimen in the emergency department as per hospital protocol.

Table 1 Patient demographics and indication for micturating cystourethrogram.
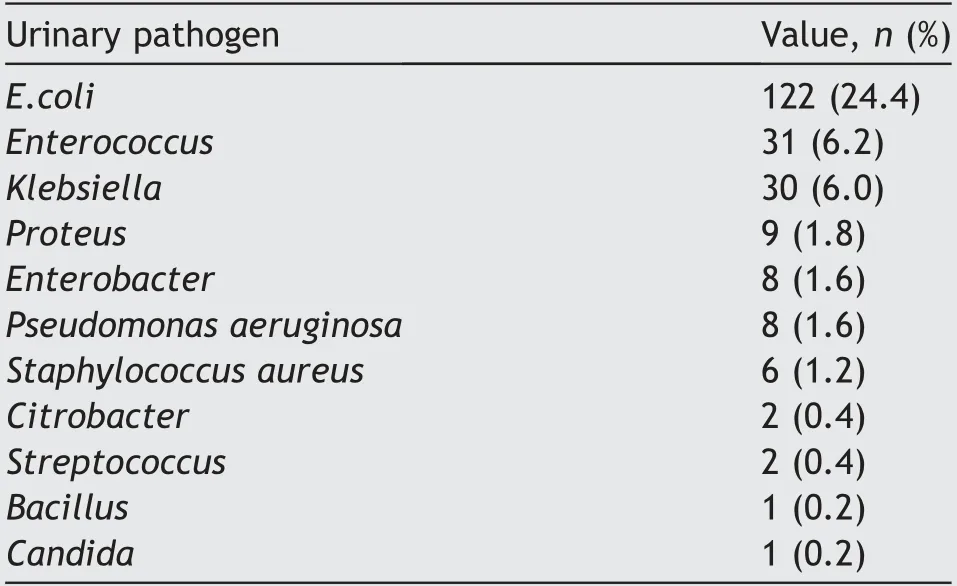
Table 2 Urine culture results of patients who had culturepositive urinary tract infection before micturating cystourethrogram.
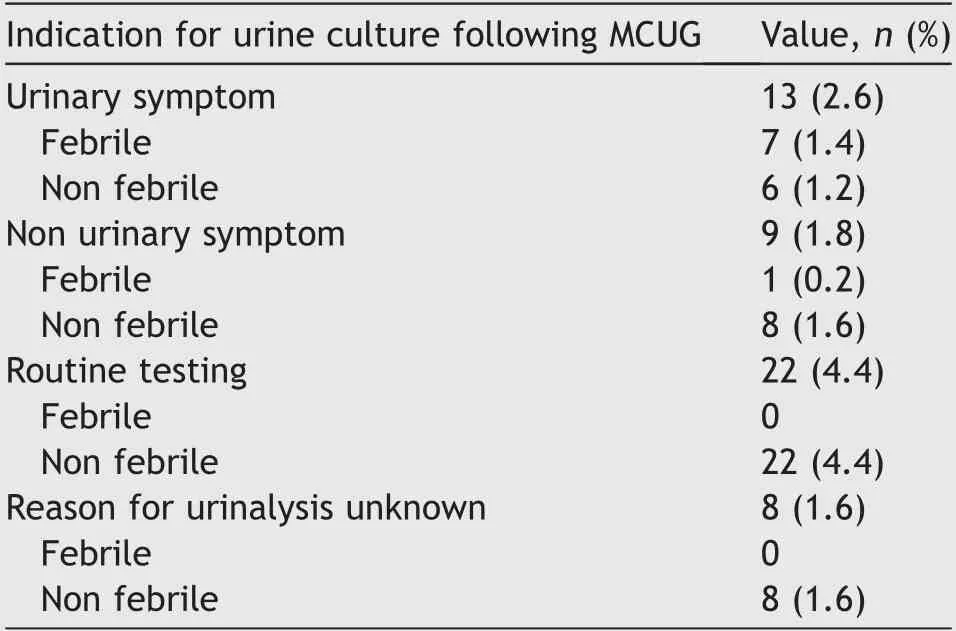
Table 3 Indication for performing urine culture within 14 days following micturating cystourethrogram.
Eighteen of the 28 patients(64.3%)who developed a post-MCUG culture-positive urine result had documentedculture-positive UTI prior to undergoing the MCUG.Seventeen(60.7%)patients who developed post-MCUG culturepositive UTI were female and 11(39.3%)were male.The most common pathogen isolated was E.coli(52.0%).
A total of 20 patients(4.0%)who had a culture-positive or mixed growth in their urine sample were treated with antibiotics,with 12 patients(2.4% of total population)treated with intravenous antibiotics and eight patients with oral antibiotics.
Univariate analysis found patients with a neurogenic bladder,patients with a previous culture-positive UTI and female patients as having an increased risk of developing culture positive UTI following MCUG(Table 4).
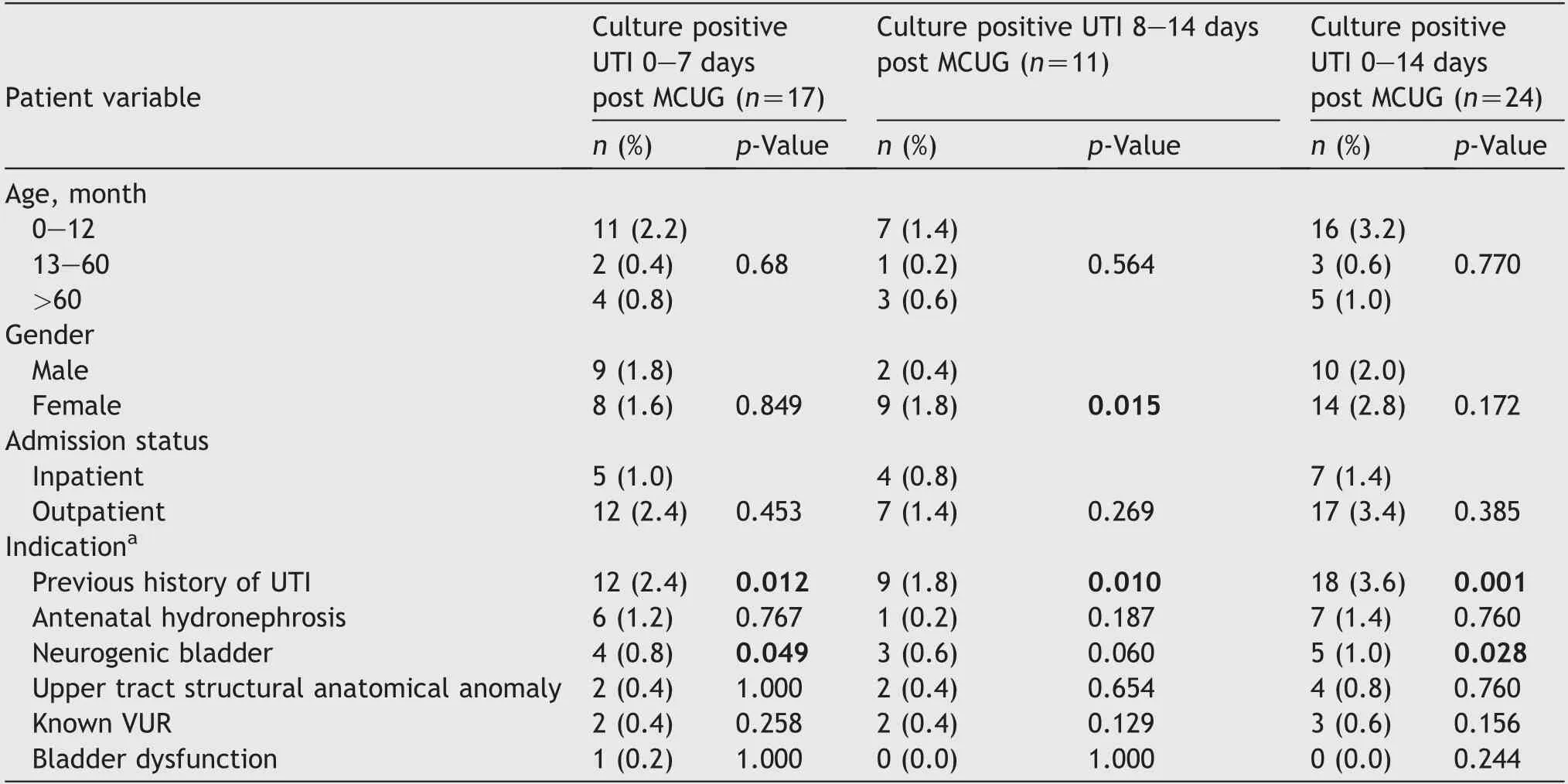
Table 4 Univariate analysis of patient subgroups-with likelihood of UTI post MCUG as the dependent variable.
Multivariate logistic regression showed that after controlling for age,gender,MCUG location,upper tract structural anatomical anomaly,bladder dysfunction,known VUR,anorectal malformation,bladder structural anatomical anomaly,previous posterior urethral valve resection,and antenatal hydronephrosis as potential confounders,patients were more likely to have culturepositive UTI within 14 days following MCUG if they had a known history of UTIs(odds ratio:5.0,95% confidence interval:1.5-17.3,p=0.010),or had a neurogenic bladder(odds ratio:4.2,95% confidence interval:1.0-17.9,p=0.049).
4.Discussion
The incidence of developing UTI is often considered to be increased after MCUG.Our study shows that following a MCUG,the incidence of culture-positive UTI is only 5.6%and the risk of developing febrile,culture-positive UTI is only 1.4%.These findings corroborate the small amount of data published on the subject.A retrospective study performed by Spencer et al.[11]determined that early MCUG following admission or presentation with febrile UTI was not associated with an increased risk of bacterial dissemination or urosepsis compared with patients who underwent MCUG at a later stage.Of note,patients who had a complex past medical history or previous MCUG were excluded from their study[11].
Similarly,researchers have suggested that performing MCUG soon after UTI provides early diagnosis to assist with the provision of a rapid treatment and management plan and is safe[12].A recent study performed by Johnson et al.[13]found that the risk of post MCUG UTI was low with an incidence of 1%in their cohort[12].This large study notably excluded patients with neurogenic bladder whom we found to be at a statistically significant,higher risk of infection[13].
A recent open-labelled,randomised control trial assessing the development of culture-positive UTI in 120 children aged 2 months to 5 years old,found prophylactic antibiotics to reduce post-MCUG acquired UTI compared to not administering prophylactic antibiotics[14].This particular trial was limited by patient age and did not specifically report on individual indications for performing MCUG including history of predisposing risk factors,e.g.neurogenic bladder or recurrent UTI.
Our study assessed all patients who had MCUG performed irrespective of the indication.Patients with neurogenic bladder and patients who had a previous,documented culture-positive UTI were found to be at greatest risk of developing post-MCUG UTI.Neurogenic bladder is a well-recognised risk factor for the development of UTI due to multifactorial dysfunction in bladder storage and emptying[15].Similarly,prior recurrence of UTI in children is associated with future recurrence[16].
Administration of prophylactic antibiotics for prevention of recurrent UTI remains a controversial topic.Consistent evidence suggesting that prophylactic antibiotics reduce recurrent UTI in children is lacking and routine use of prophylactic antibiotics is not recommended[16,17].At our institution,prior to MCUG patients are not routinely administered prophylactic antibiotics.However,patients already on antibiotic prophylaxis continued their usual regime prior to and after the MCUG.
There were recognized limitations to our study.For example,patients who underwent MCUG at our institution(the only children’s hospital in the entire state)would be provided with instructions to re-present to the emergency department at the hospital should they develop any infective signs or symptoms.However,medical records were not accessible for patients who may have presented at and been treated for a UTI at a different healthcare facility.Categorisation of patients according to MCUG indication was retrospectively based on patient records,so inadvertent selection bias is possible.Data were presented since 2013;however,process and technique for performing MCUG within the institution have remained the same.
Accurate detection and statistical analysis of adverse events following MCUG are appreciably difficult.Ideally,any child undergoing a urinalysis following MCUG should have the indication,symptoms,and presence of a fever documented.Additionally,the results of the urinalysis,management plan including duration,route,and type of antibiotic if required,and treatment response should similarly be recorded and centrally reviewed.Given the nature of the patient cohort and the retrospective data collection,complete and accurate records were to a degree limited.
5.Conclusion
These data provide important reassurance to patients,carers,and clinicians that for the vast majority of patients,MCUG is a safe procedure with very low risk of febrile culture-positive UTI.Further prospective studies are necessary to determine the clinical need of prophylactic antibiotics for high-risk patients,e.g.,neurogenic bladder patients and patients with prior,culture-positive UTI.
Author contributions
Study design:Simeon Ngweso,Munyaradzi Nyandoro,Naeem Samnakay.
Data acquisition:Simeon Ngweso,Munyaradzi Nyandoro,Ting Yi Cheow.
Data analysis:Simeon Ngweso,Munyaradzi Nyandoro,Tatenda Nzenza.
Drafting of manuscript:Simeon Ngweso,Munyaradzi Nyandoro,Tatenda Nzenza,Naeem Samnakay.
Critical revision of the manuscript:Simeon Ngweso,Fiona Bettenay,Andrew Barker,Japinder Khosa,Naeem Samnakay.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2022年3期
Asian Journal of Urology2022年3期
- Asian Journal of Urology的其它文章
- Burned-out testicular seminoma with retroperitoneal metastasis and contralateral sertoli cell-only syndrome
- Endoscopic management of adolescent closed Cowper’s gland syringocele with holmium:YAG laser
- Transcutaneous dorsal penile nerve stimulation for the treatment of premature ejaculation:A novel technique
- Bilateral calcified Macroplastique® after 12 years
- A phase II study of neoadjuvant chemotherapy followed by organ preservation in patients with muscle-invasive bladder cancer
- Augmentation cystoplasty in children with stages III and IV chronic kidney disease secondary to neurogenic bladder
