Assessment of structural brain changes in patients with type 2 diabetes mellitus using the MRI-based brain atrophy and lesion index
Heng Zhao, Fang Wang, Guang-Hua Luo, Hao Lei, Fei Peng, Qiu-Ping Ren,Wei Chen, Yan-Fang Wu, Li-Chun Yin, Jin-Cai Liu,*, Shi-Nong Pan
Abstract Patients with type 2 diabetes mellitus (T2DM) often have cognitive impairment and structural brain abnormalities.The magnetic resonance imaging (MRI)-based brain atrophy and lesion index can be used to evaluate common brain changes and their correlation with cognitive function, and can therefore also be used to reflect whole-brain structural changes related to T2DM.A total of 136 participants (64 men and 72 women, aged 55–86 years) were recruited for our study between January 2014 and December 2016.All participants underwent MRI and Mini-Mental State Examination assessment (including 42 healthy control, 38 T2DM without cognitive impairment, 26 with cognitive impairment but without T2DM, and 30 T2DM with cognitive impairment participants).The total and sub-category brain atrophy and lesion index scores in patients with T2DM with cognitive impairment were higher than those in healthy controls.Differences in the brain atrophy and lesion index of gray matter lesions and subcortical dilated perivascular spaces were found between non-T2DM patients with cognitive impairment and patients with T2DM and cognitive impairment.After adjusting for age, the brain atrophy and lesion index retained its capacity to identify patients with T2DM with cognitive impairment.These findings suggest that the brain atrophy and lesion index, based on T1-weighted and T2-weighted imaging, is of clinical value for identifying patients with T2DM and cognitive impairment.Gray matter lesions and subcortical dilated perivascular spaces may be potential diagnostic markers of T2DM that is complicated by cognitive impairment.This study was approved by the Medical Ethics Committee of University of South China (approval No.USC20131109003) on November 9, 2013,and was retrospectively registered with the Chinese Clinical Trial Registry (registration No.ChiCTR1900024150) on June 27, 2019.
Key Words: brain atrophy and lesion index; cognitive impairments; gray matter lesions; magnetic resonance imaging; Mini-Mental State Examination; structural brain; subcortical dilated perivascular spaces; T1-weighted image; T2-weighted image; type 2 diabetes mellitus
Introduction
Typically, type 2 diabetes mellitus (T2DM) has a negative impact on cognitive function, especially in aging individuals,and increases the risk of cognitive impairment (CI), including Alzheimer’s disease (AD) and vascular dementia (Wang et al., 2014; Bangen et al., 2018; Biessels and Despa, 2018;Agatonovic-Kustrin et al., 2019; Callisaya et al., 2019;Chornenkyy et al., 2019; Groeneveld et al., 2019; International Diabetes Federation, 2020; Popa-Wagner et al., 2020).Previous research has indicated that individuals with T2DM are at ~60% greater risk for the development of dementia compared with those without diabetes (Kanaya et al., 2004).For vascular dementia, this risk is even greater in women with diabetes (Chatterjee et al., 2016).However, the difference between men and women has not been observed consistently in some similarly large, contemporary studies (Shah et al.,2015; Wright et al., 2019).
Both CI and structural brain abnormalities have been reported in T2DM.Previous research suggests that patients with diabetes mellitus represent a large proportion of adults with cerebral small vessel disease, the structural brain abnormalities correlates of which include lacunar infarcts, white matter hyperintensities, enlarged perivascular spaces, microbleeds, and brain atrophy (Funnell et al., 2017;Mankovsky et al., 2018).Compared with healthy older people,older patients with T2DM have more severe structural brain changes (Moran et al., 2013).
The brain atrophy and lesion index (BALI), which is a validated semi-quantitative global measure of structural degeneration,has been used to collectively assess common brain changes and their association with cognitive function.Previous studies have shown that BALIs are significantly associated with age and dementia progression (Chen et al., 2010; Zhang et al.,2012; Guo et al., 2014a, b, 2017).Thus, it is possible that the BALI could also be applied to assess T2DM-related wholebrain structural changes.The present study was designed to rapidly assess structural brain changes in patients with T2DM using the BALI, and to evaluate the ability of T1-weighted(T1WI) and T2-weighted (T2WI)-based BALI to identify which patients with T2DM have CI.
Participants and Methods
This retrospective observational study was approved by the Medical Ethics Committee of University of South China(approval No.USC20131109003) on November 9, 2013(Additional file 1), and written informed consent (Additionalfile 2) was obtained from all participants.All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.This study followed the Strengthening the Reporting of Оbservational Studies in Epidemiology (STRОBE)guidance (Additional file 3).The study was retrospectively registered with the Chinese Clinical Trial Registry (registration No.ChiCTR1900024150) on June 27, 2019.
Participants
The study was conducted between January 2014 and December 2016.All participants were recruited from The First Affiliated Hospital of University of South China.The inclusion criteria were as follows: aged more than 50 years and less than 90 years.The exclusion criteria were as follows:(1) patients who could not complete the Mini-Mental State Examination (MMSE); (2) patients with a history of mental and/or neurological diseases; (3) those with organic diseases of the nervous system; (4) a history of alcohol, smoking, or drug abuse; (5) patients with contraindications for magnetic resonance imaging (MRI).Diabetes was confirmed based on clinical records.A diagnosis of CI was established using the MMSE.A total of 141 randomly recruited participants completed MRI scanning and the MMSE assessment, but 5 participants were excluded because of poor MR image quality.The final 136 participants were divided into four groups (Figure1), as follows: (a) the healthy control (HC) group (n= 42),with normal cognitive function and without T2DM; (b) the T2DM-nonCI group (n= 38), which comprised patients with T2DM without CI; (c) the nonT2DM-CI group (n= 26), which comprised participants with CI but without T2DM; and (d) the T2DM-CI group (n= 30), which included patients with both T2DM and CI.The enrolled participants included 64 men and 72 women aged from 50 to 86 years.
MRI protocol
MRI was performed using either a 1.5-T (Brivo MR355, GE Healthcare, Milwaukee, WI, USA; MAGNETОM, Siemens Healthcare, Erlangen, Germany) or a 3.0-T scanner (Achieva,Philips Healthcare, Best, the Netherlands) using either an 8-channel or 16-channel phased-array coil.Both conventional T1WI and T2WI images were acquired in the axial plane.
Evaluation of the BALI
The BALI scale was used to assess several common structural brain changes.The first category is gray matter lesions and subcortical dilated perivascular spaces (GM-SV) (Chen et al., 2010; Zhang et al., 2012; Guo et al., 2014a, b, 2017).Subsequent categories assess deep white matter lesions,periventricular white matter lesions, lesions in the basal ganglia and surrounding areas, lesions in the infratentorial compartment, and global atrophy.An “other findings”category records changes such as neoplasm, trauma,malformations, and hydrocephalus.Each category was assigned a value between 0 and 3, whereby a higher score indicates a more severe change.In two categories (deep white matter lesions and global atrophy), values of 4 and 5 were used to represent greater severity (Chen et al., 2010;Zhang et al., 2012; Guo et al., 2014a, b, 2017).The total BALI was calculated separately for T1W1 and T2W1 images by adding scores for the seven sub-categories, with a maximum total score of 25.The BALI scoring was performed by two radiologists (HZ and FW) with 20 and 8 years of experience in neural imaging, respectively.Evaluations for the two different MRI sequences were separated by one week to minimize possible recall bias.Scoring was performed independently,and the reviewers were blinded to all information, including participant demographics, diagnosis, and MMSE score.The scoring standard is presented inAdditionalFigures 1and2,and example images showing the BALI rating are shown inFigure 2.
Cognitive test
The MMSE was used to assess global cognitive function and was implemented by trained physicians and nurses (Zhang et al., 1999).There are 30 items in the MMSE, with a total possible score of 30.The MMSE measures the five following aspects of cognition: orientation (10 items), registration (3 items), attention and calculation (5 items), recall (3 items),and language (9 items).The MMSE cut-off score for defining normal cognition was as follows: a score ≥ 19 in illiterate individuals; ≥ 22 in those with a primary school education(education duration ≤ 6 years); and ≥ 26 in those with a middle school education and above (education duration > 6 years) (Zhang et al., 1999).Scores below these cut-off values were considered to indicate CI.
Statistical analysis
SPSS 23.0 (IBM Corp., Armonk, NY, USA) was used for all data analysis.Non-normally distributed data, as determined by the Kolmogorov-Smirnov test, were transformed logarithmically prior to analysis and are expressed as the median and interquartile range.Reliability of the ratings was examined using the inter-reviewer agreement rate (Cohen’s kappa).Differences between groups regarding age, sex, and level of education were examined using Kruskal-Wallis nonparametric tests for interval data and the chi-square test for categorical/ordinal data.Comparisons of the BALI between groups were performed using Kruskal-Wallis nonparametric tests, and correlations between the MMSE score and BALI were assessed using Spearman’s correlation analysis.Evaluation of the ability of the BALI to identify patients with T2DM and CI was carried out using receiver operating characteristics curves.P< 0.05(two-tailed) was considered statistically significant.
Results
Participant demographics
No significant difference in education level was found between the four groups (χ2= 1.66,P> 0.05); however, significant differences were found in age (χ2= 21.65,P< 0.001), sex (χ2=8.03,P= 0.045), and MMSE score (χ2= 18.04 –85.40,P< 0.01)between the four groups (Table 1).
Intraclass correlation coefficient of BALI scoring between reviewers
With regard to reliability, the intraclass correlation coefficient of BALI scoring indicated an agreement that ranged from good to perfect (κvalue: 0.64–0.90,P< 0.001).Theκcoefficients for T1WI varied from 0.64, with lesions in GM-SV, to 0.90, with lesions in the infratentorial compartment.Theκcoefficients for T2WI varied from 0.65, with lesions in DWM, to 0.82, with lesions in global atrophy (Table 2).
Between-group differences in the total and sub-category BALIs
Total and sub-category BALIs of the different groups are compared inTable 3.The non-T2DM-HC group had lower total and all sub-categories BALIs than the T2DM-CI group(bothP< 0.05).Furthermore, the T2DM-HC group total BALI only was lower than that of the T2DM-CI group (P< 0.05),and sub-category BALIs exhibited no significant differences(P> 0.05).In addition, only the GM-SV index was significantly different between the nonT2DM-CI and T2DM-CI groups(reviewer 1: T1WIχ2= 24.54,P< 0.001; T2WIχ2= 23.02,P=0.017; reviewer 2: T1WIχ2= 17.76,P= 0.012; T2WIχ2= 5.30,P= 0.151).
Ability of the BALI to discriminate patients with T2DM and CI
In T2DM subjects, T1WI- and T2WI-based BALIs showed comparable accuracy for the classification of patients with T2DM and CI at the individual level.After adjusting for age,the area under the curve ranged from 0.550 to 0.749, and the total BALI had the highest sensitivity (Figure 3andTable 4; the cut-off value was 9 in T1WI: 73.33%vs.73.33% for reviewers 1 and 2; the cut-off value was 10.5 in T2WI: 70.00%vs.76.67%for reviewers 1 and 2).
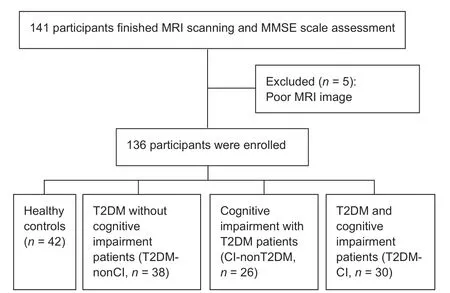
Figure 1|Trial flow chart.
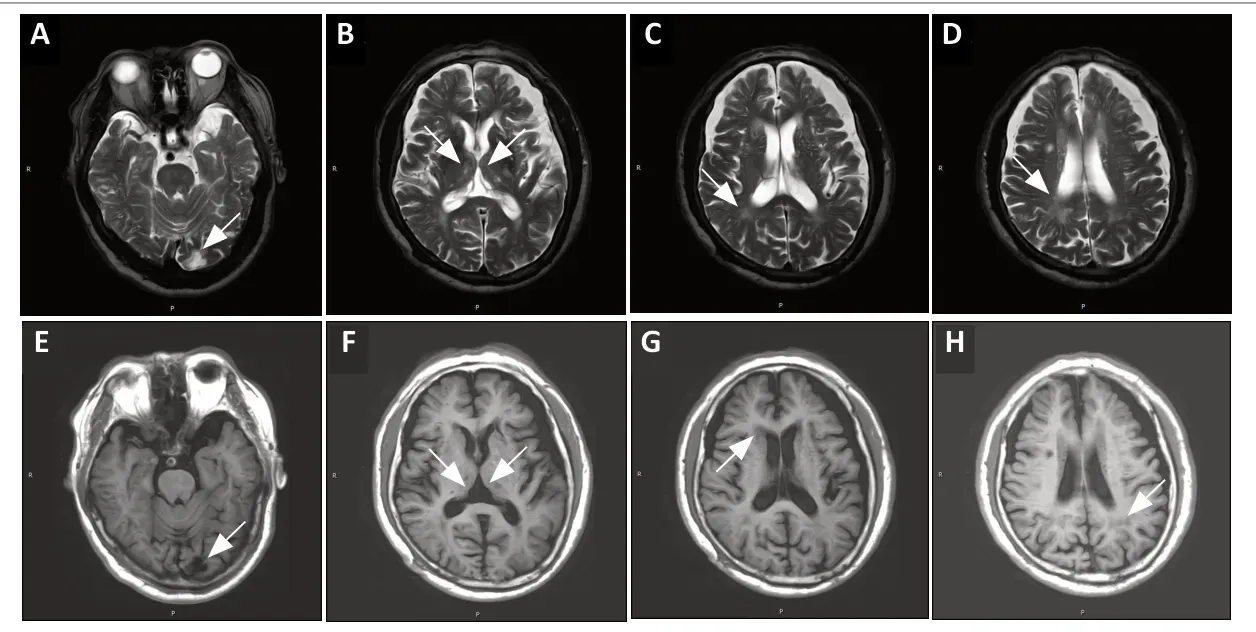
Figure 2|T1- and T2-weighted-based BALI scoring in a 72-year-old woman diagnosed with T2DM-CI.
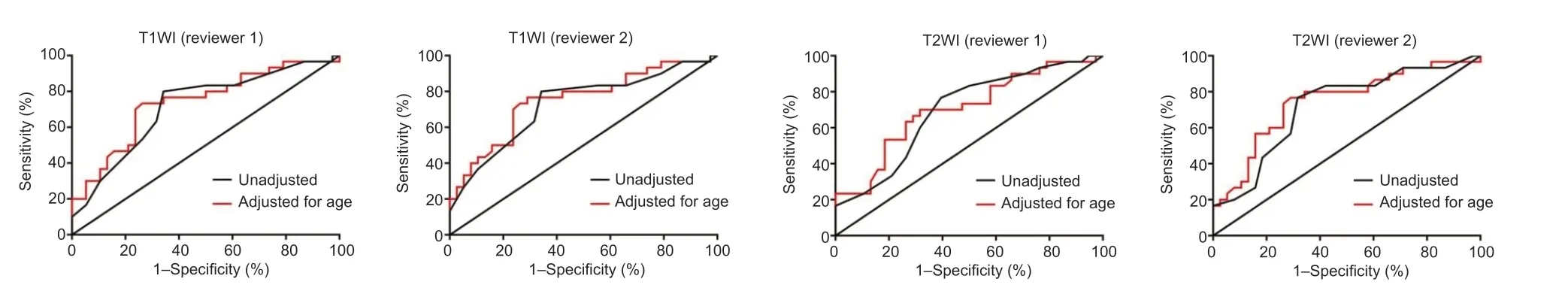
Figure 3|Receiver operating characteristics curve analysis for the prediction of type 2 diabetes mellitus with cognitive impairment.
Correlation between the MMSE score and BALI in T2DM and nonT2DM groups
In the T2DM and non-T2DM groups, most BALIs and MMSE scores were significantly correlated.However, the GM-SV score was significantly correlated with the MMSE total (|r|= 0.259–0.267,P< 0.05 for reviewer 1’s T1WI and T2WIbased score) and recall score (|r| = 0.306–0.325,P< 0.05 for reviewer 1’s and reviewer 2’s T1WI-based score and reviewer 1’s T2WI-based score) within the T2DM groups, but no significant correlations were found within the nonT2DM groups (Additional Tables 1and2).
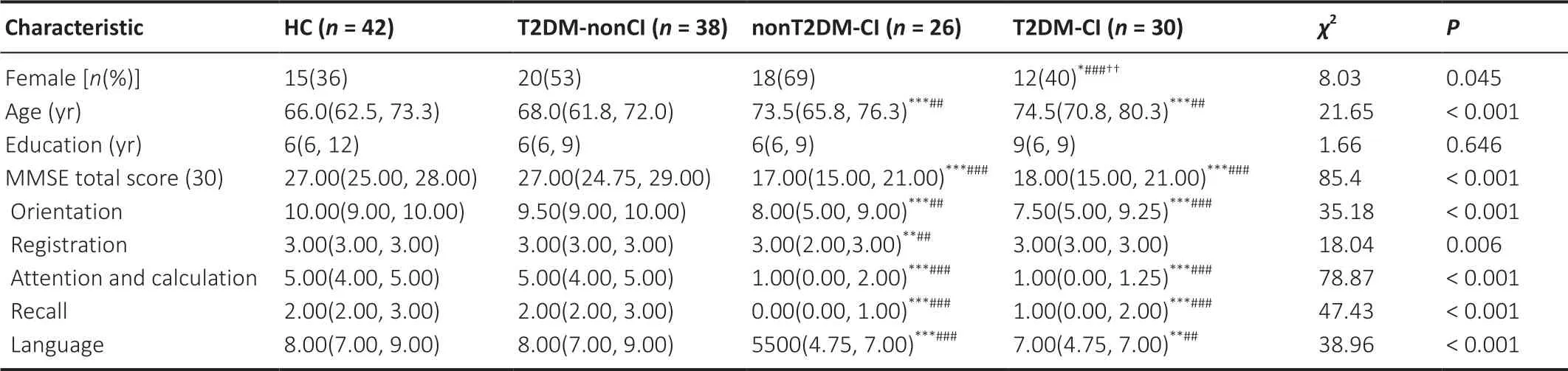
Table 1 |Demographic characteristics of participants
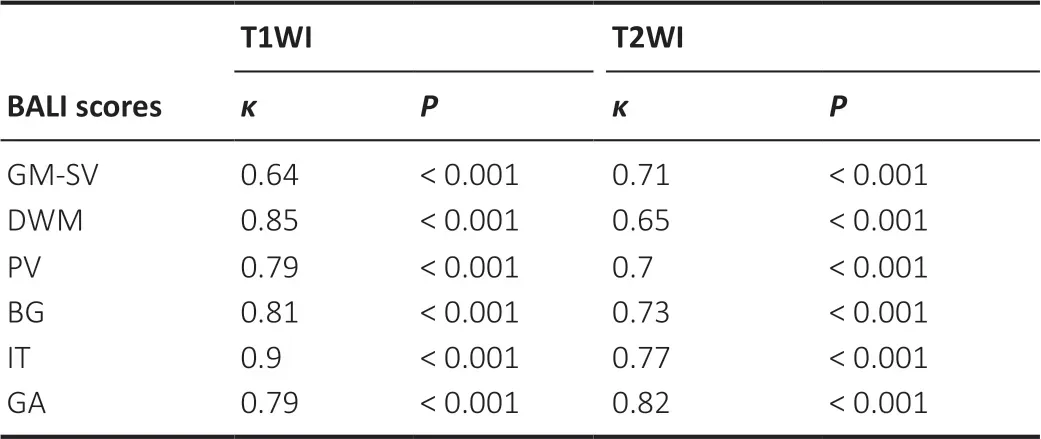
Table 2 | Agreement in the total and sub-category BALIs between the two reviewers
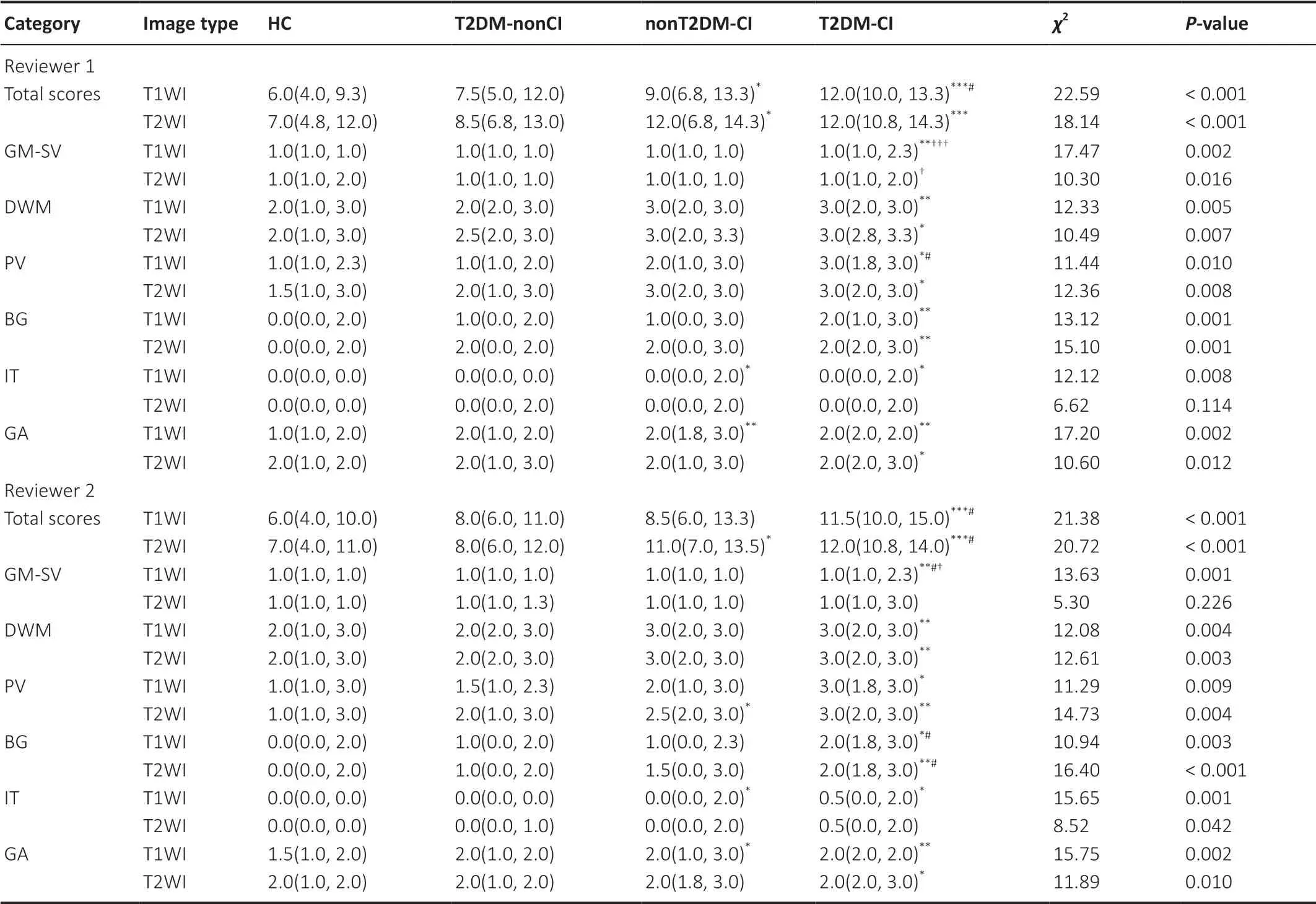
Table 3 |Between-group differences in the total and sub-category BALIs
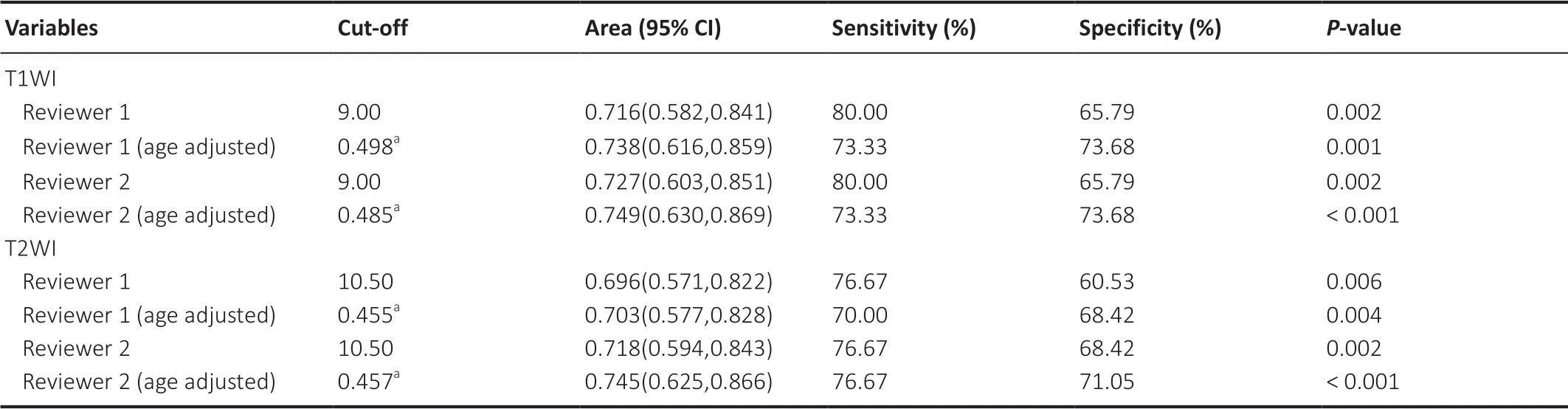
Table 4 |Sensitivity, specificity, and AUC for the BALI in predicting type 2 diabetes mellitus with cognitive impairment
Discussion
This study investigated the use of routine clinical MRI examinations in the evaluation of brain health in patients with T2DM.Previous research has shown that the BALI allows us to simultaneously assess multiple structural changes in the aging and AD brain (Guo et al., 2014a, 2017).This previous work has not only shown that both T1WI and T2WI at 1.5T or 3.0T have good reliability when evaluating global structural brain changes (Guo et al., 2014a), but also that this method is quick and easy to perform, which could be particularly beneficial to and have widespread usefulness in clinical contexts (Guo et al., 2014a).Оur data revealed the consistency of both T1WI and T2WI-based BALI total and sub-category scores between reviewers, which ranged from good to perfect.
In recent years, many studies have focused on the effect of structural brain changes on the progression of CI in older people, and have revealed that several common structural brain changes are related to CI (Li and Huang, 2016; Cuadrado-Godia et al., 2018; Shibata et al., 2019; Li et al., 2020; Lu and Deng, 2020).However, few recent studies have attempted to account for more than one type of structural brain change.For instance, the widely used Fazekas and Scholten scores only assess white matter hyperintensity and medial temporal lobe atrophy, and do not assess multiple changes.Previous research has shown that the BALI is a global measure that can evaluate multiple common changes that take place during aging and AD; furthermore, these changes can be independently related to dementia, and, when BALI sub-categories are evaluated together, the negative association with cognitive function becomes stronger (Manschot et al., 2006; Szémán et al., 2012;Guo et al., 2014b; Zhang et al., 2014; Bouvy et al., 2016; Hilal et al., 2018).Оur results not only showed that cognition was consistently correlated with multiple structural brain changes,but also indicated that T2DM-CI patients had more severe,or higher sub-category BALI values, than T2DM-HC patients.Therefore, we speculate that worsening cognitive function in T2DM patients indicates that structural brain changes are also worsening.
To our knowledge, this is the first study to use the BALI to evaluate the T2DM brain.Оne of the most important findings of the present study is that only the GM-SV score was significantly different between CI subjects with and without T2DM.We also found that the GM-SV score was significantly correlated with the MMSE total and recall score in T2DM subjects, but no such correlation was found in nonT2DM subjects.Previous research has highlighted cortical infarction and perivascular spaces as increasingly recognized markers of cerebral small vessel disease in aging and dementia (Martinez-Ramirez et al., 2013).Somein vivoMRI studies have not only shown an association between severe centrum semiovale perivascular spaces and lobar (micro) hemorrhages, which are markers of cerebral amyloid angiopathy (Peila et al.,2002; Charidimou et al., 2013, 2014, 2017), but have also found that cerebral amyloid angiopathy severity is linked to the dilation of juxtacortical perivascular spaces (van Veluw et al., 2016).In addition, diabetes has been associated with a higher prevalence of cerebral amyloid angiopathy (Wardlaw et al., 2013).Considering these previous findings and our own results, GM-SV could represent a potential imaging marker of patients with T2DM and CI.
Previous research has demonstrated that the total BALI can help to improve AD and mild cognitive impairment diagnoses in aging (Chen et al., 2010; Zhang et al., 2012; Guo et al.,2014a, b, 2017).After adjusting for age, we found that both the total and sub-category BALIs could predict which patients had T2DM with CI; the total BALI had the highest sensitivity and a good specificity.This indicates that several subtle structural changes, measured by the BALI sub-categories,can be collectively evaluated by the total BALI and that this achieved a greater ability to predict T2DM with CI.
This study has some limitations.First, the relatively small sample size in our study limits the generalizability of our results.Second, the lesion size judgment (e.g., “large patchy lesions”) may differ for different categories, because “large”can vary depending on brain structure.For example, a “large”change in the relatively smaller lesions in the infratentorial regions may not be considered “large” in the basal ganglia and surrounding areas or DWM.Future research could adopt quantitative measurements (in mm) to improve precision.In addition, several advanced MR techniques have more precise morphometric or volumetric quantifications than conventional MR sequences (Kanaan et al., 2012; Xie et al.,2017; Gatto and Weissmann, 2019; Sanjari Moghaddam et al., 2019).Adopting these more advanced measures in future studies could improve the detection of gray and white matter changes, especially for lesions that occur in the early stages of T2DM, which would in turn enhance the diagnostic specificity and sensibility.
In conclusion, we found associations between structural brain changes, T2DM, and cognitive function.T1WI- and T2WIbased BALIs have potential diagnostic value in the assessment of CI caused by T2DM.The total BALI exhibited the highest sensitivity, and the GM-SV BALI could be a potential imaging marker of T2DM with CI.Therefore, we suggest that BALI is an easy and convenient method that could provide more information to aid the clinical diagnosis and treatment of T2DM with CI.
Author contributions:Guarantors of integrity of entire study: HZ, FW,JCL, SNP; experiment implementation: HZ, FW, WC, YFW; statistical analysis: HZ, FW, FP, LCY; manuscript editing: HZ, FW, GHL, JCL, SNP.All authors have designed the study, collected and analyzed the data,drafted and revised the manuscript and approved the final version of the manuscript.
Conflicts of interest:There were no conflicts of interest.
Financial support:This study was supported by the National Natural Science Foundation of China, No.81271538 (to SNP); 345 Talent Project and the Natural Science Foundation of Liaoning Province of China,No.2019-ZD-0794 (to SNP); the Natural Science Foundation of Hunan Province of China, Nos.2017JJ2225 (to JCL), 2018JJ2357 (to GHL);Hunan Provincial Science and Technology Innovation Program of China,No.2017SK50203 (to HZ).The funders had no role in study design,data collection and analysis, decision to publish, or preparation of the manuscript.
Institutional review board statement:This study was approved by the Medical Ethics Review Form of University of South China (approval No.USC20131109003) on November 9, 2013, and was retrospectively registrated at Chinese Clinical Trial Registry (Registration No.ChiCTR1900024150) on June 27, 2019.
Declaration of patient consent:The authors certify that they have obtained all appropriate patient consent forms from the patients.In the forms, the patients have given their consent for their images and other clinical information to be reported in the journal.The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Reporting statement:This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidance.
Biostatistics statement:The statistical methods of this study were reviewed by the biostatistician of Shengjing Hospital of China Medical University.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement:Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix,tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:Rodolfo Gabriel Gatto, University of Illinois at Chicago, USA.
Additional files:
Additional file 1: Hospital Ethics Approval.
Additional file 2: Informed consent form.
Additional file 3: STROBE checklist.
Additional file 4: Open peer review report 1.
Additional Table 1: Spearman correlation coefficients between MMSE scores and BALI scores in type 2 diabetes mellitus patients.
Additional Table 2: Spearman correlation coefficients between MMSE scores and BALI scores in HC and nonT2DM-CI patients.
Additional Figure 1: Evaluation of the brain atrophy and lesion index(BALI) based on T1WI.
Additional Figure 2: Evaluation of the brain atrophy and lesion index based on T2WI.
- 中国神经再生研究(英文版)的其它文章
- Pathological mechanisms and therapeutic strategies for Alzheimer’s disease
- Pentadecapeptide BPC 157 and the central nervous system
- OTX2 stimulates adult retinal ganglion cell regeneration
- Mutations in GBA, SNCA, and VPS35 are not associated with Alzheimer’s disease in a Chinese population:a case-control study
- Role of microtubule dynamics in Wallerian degeneration and nerve regeneration after peripheral nerve injury
- Krüppel-like factor 7 attenuates hippocampal neuronal injury after traumatic brain injury