Changes in the esophagogastric junction outflow obstruction manometric feature based on the Chicago Classification updates
Yue-Yuan Li, Wen-Ting Lu, Jian-Xiang Liu, Li-Hong Wu, Meng Chen, Hong-Mei Jiao
Abstract
Key Words: Esophagogastric junction outflow obstruction; High-resolution manometry; Esophageal motility disorders; Upper esophageal sphincter; Proximal esophagus
lNTRODUCTlON
Esophagogastric junction outflow obstruction (EGJOO) is a common type of esophageal motility disorder in patients with dysphagia or chest pain. EGJOO includes a group of heterogeneous disorders with common manometric features for esophageal outflow obstruction. Progress has been made toward understanding the manometric features and symptoms of patients who meet the EGJOO criteria[1-5].The Chicago Classification version 4.0 (CCv4.0) updated the critical diagnostic criteria for the manometric diagnosis of EGJOO, including increased median-integrated relaxation pressure (IRP) in supine and upright positions, ≥ 20% elevated intrabolus pressure (IBP) in the supine position, and evidence of peristalsis[1]. A clinically relevant conclusive diagnosis of EGJOO requires a manometric diagnosis of EGJOO as described above, and clinically relevant symptoms with at least one of the complementary tests, including timed barium esophagram and functional lumen imaging probe.Additional provocative tests including rapid drink challenge (RDC), solid test swallows, or pharmacologic provocation may also strengthen the confidence in an EGJOO diagnosis and helps to identify the causes of symptoms, particularly in borderline cases. Compared with the previous version (v3.0)[6], the new diagnostic criteria provided a more rigorous definition for EGJOO by adding criteria for median IRP in the secondary position, IBP, clinically relevant symptoms, and complementary tests, which aid in distinguishing pathological motility disorder and abnormal manometry caused by mechanical effect,opioid use, or other nonpathological motility disorders[7]. However, the change in manometric features of EGJOO with the diagnostic criteria modification remained unclear. This study aims to investigate the esophageal motility features of patients with the manometric diagnosis of EGJOO and to identify highresolution manometry (HRM) parameters that are supportive for confirming the diagnosis of EGJOO.
MATERlALS AND METHODS
Patient and data selection
Patients who completed esophageal HRM and upper gastrointestinal endoscopy from November 2016 to November 2021 at Peking University First Hospital were retrospectively analyzed. Exclusion criteria included: (1) Patients under 18 years of age; (2) A history of upper gastrointestinal or mediastinal surgery; (3) Previous endoscopic treatment for esophageal motor disorders; (4) Diseases with abnormal intraabdominal pressure, such as intestinal obstruction or ascites; (5) Use of opiates; and (6) Secondary factors identified by upper gastrointestinal endoscopy or endoscopic ultrasonography, especially for hiatal hernia, infiltrative disease, mechanical obstruction, and extrinsic compression. The normal HRM group was obtained from patients who underwent HRM for mild symptoms such as dysphagia,retrosternal pain, regurgitation, or heartburn, with normal HRM results. The patients also fulfilled normal results in pH-monitoring and upper gastrointestinal endoscopy, in order to exclude the possibility of organic diseases. Demographic data, including age, gender, body mass index (BMI),previous medical and surgical history were collected, and symptoms were extracted from self-report questionnaires completed by patients before HRM. The Institutional Review Board (IRB) of the Peking University First Hospital approved the study protocol (2022-099). The IRB waived the requirement for informed consent because our retrospective analysis used completely anonymized data.
HRM protocol
HRM studies were conducted according to standard clinical protocol, using a 4.2-mm outer diameter,36-sensor solid-state HRM catheter (ManoScan™, Medtronic, Los Angeles, CA, United States)[8].Experienced nurses performed nasal canal anesthesia and transnasal placement of the solid-state manometry catheter with the patient sitting upright after an 8-h fast. Sensors were positioned to ensure a complete record of the hypopharynx, esophagus, and proximal stomach. The manometric protocol consisted of a landmark phase captured during a quiet rest in the supine position at the beginning,followed by ten 5-mL ambient temperature water swallows in the supine position, then five 5-mL water swallows in the upright position, with 30 s between each swallow, and finally a RDC of 200 mL water in the upright position.
HRM data analysis
HRM Clouse plots were analyzed using computerized HRM analysis software (Manoview, Medtronic).All pressure measurements were referenced to the gastric pressure.
Upper esophageal sphincter parameters[9,10]: Upper esophageal sphincter (UES) parameters were measured within the UES high-pressure zone defined by a 20-mmHg isobaric contour, consisting of UES length (UESL), UES resting pressure (UESP), nadir pressure (UESNP), and postdeglutitive UES contractile integral (PD-UESCI). PD-UESCI was measured by the smart mouse at the beginning of the deglutitive UES relaxation to the end of the proximal esophageal contraction or the beginning of the transition zone (Figure 1).
Proximal esophageal parameters[9,11]: Proximal esophageal parameters measured from the lower border of the UES to either a break between the proximal and distal segment or the area with the lowest pressure between the proximal and distal segment of the contraction in patients showed no break in the 20-mmHg isobaric contour. Measurements of the proximal esophageal segment included proximal esophageal segment length (PEL), proximal latency (PL, defined as the time interval between UES relaxation to the transition zone), and proximal esophageal contractile integral (PECI, = amplitude ×duration × length, measured using a 20-mmHg pressure threshold).
Esophageal body parameters[12]: Esophageal shortening during RDC (ES-RDC) was defined as an upward lift of lower esophageal sphincter (LES) for more than 1 cm, as measured by the length variation between the baseline position of the LES before RDC and its maximal axial position during RDC or within 60 s after the start of RDC. The distal latency (DL) and distal contraction integral (DCI)were calculated automatically using the ManoView system.
Esophagogastric junction parameters[13]: The LES resting pressure (LESP), IBP were calculated automatically using the ManoView system. The median IRP in the supine and upright positions was selected from a list of IRP in each position. The IRP on RDC was assessed in the window beginning with dilatative UES relaxation to the end of esophagogastric junction (EGJ) relaxation for free drinking lasting less than 30 s, or during the first 30 s of the window for free drinking lasting longer.
Statistical analysis
Statistical analysis was performed using SPSS 25.0, and GraphPad Prism 8.0. The chi-square test was used for the comparison of categorical variables. The Student’st-test and analysis of variance were used to compare quantitative data with normal distribution between groups, and the results are expressed as mean ± SD. Multivariate analysis was performed with stepwise variable selection. The receiveroperating characteristics (ROC) curve was used to illustrate the diagnostic ability of the HRM parameters for EGJOO. APvalue < 0.05 was considered statistically significant.
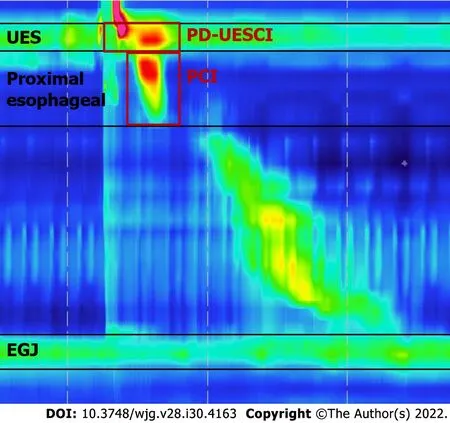
Figure 1 Key metrics of Clouse plots used in our study. The postdeglutitive upper esophageal sphincter (UES) contractile integral was measured using a 20-mmHg pressure threshold from the beginning of the deglutitive UES relaxation to the end of the proximal esophageal contraction or the beginning of the transition zone. The proximal esophageal contractile integral was measured using a 20-mmHg pressure threshold from the lower border of the UES to either a break between the proximal and distal segment or the area with the lowest pressure between the proximal and distal segment of the contraction in patients showed no break in the 20-mmHg isobaric contour. UES: Upper esophageal sphincter; PD-UESCI: Postdeglutitive upper esophageal sphincter contractile integral; PCI: Proximal contractile integral; EGJ: Esophagogastric junction.
RESULTS
Patient characteristics
Fifty-one patients (33 female, 59.5 ± 1.7 years) fulfilling the criteria of EGJOO (CCv3.0) were identified,with supine IRP ≥ 15 mmHg (Medtronic) and evidence of peristalsis. Among them, 24 patients (14 female, 62.7 ± 2.7 years) met the manometric definitions of EGJOO (CCv4.0), while 27 patients (19 female, 56.6 ± 11.1 years) failed to meet the updated EGJOO criteria formed the isolated supine IRP elevated group, with either normal median IRP in upright position or less than 20% of supine swallows with elevated IBP. The normal HRM group comprised 46 patients (24 female, 50.2 ± 2.2 years) with normal HRM results (Figure 2). Patients in the EGJOO group were older than the normal HRM group.There was no difference in gender or BMI between these three groups. As for symptoms, among the 24 patients with manometric diagnosis of EGJOO (CCv4.0), there were seven with dysphagia and five with retrosternal pain that might be clinically relevant. Symptoms were also counted in isolated supine IRP elevated group and normal HRM group as shown in Table 1. The occurrence of dysphagia, retrosternal pain, and regurgitation did not differ between these three groups. Among the 24 patients with manometric diagnosis of EGJOO (CCv4.0), there were five patients with spastic features, five with hypercontractile features, two with ineffective motility, and twelve with no evidence of peristalsis disorders.
Esophageal HRM parameters
Table 2 details the differences in manometric parameters among EGJOO, isolated supine IRP elevated group, and the normal HRM group.
UES parameters: UESNP was significantly higher in the EGJOO group and the isolated supine IRP elevated group than in the normal HRM group. There was no significant difference in UESL, UESP, and PD-UESCI between the three groups.
Proximal esophageal parameters: Proximal esophageal contractile function was weaker in the EGJOO group than in the normal HRM group, specifically PEL and PECI. Consistently, PEL was lower in the EGJOO group than in the isolated supine IRP elevated group. There was no difference in PL in the EGJOO group, isolated supine IRP elevated group, and the normal HRM group.

Table 1 Patient characteristics
Esophageal body parameters: There was no significant difference in DL, DCI, and ES-RDC among the three groups.
EGJ parameters: Patients with EGJOO exhibited stronger contractile function in EGJ than in the isolated supine IRP elevated group and the normal HRM group, including LESP, IBP, median supine IRP,median upright IRP, and IRP on RDC.
The multivariate analysis revealed that PEL, LESP, and IRP on RDC are factors associated with EGJOO (Table 3).
Relationship between symptoms and parameters
We compared parameters based on symptoms for the 51 patients with elevated IRP. Patients with dysphagia showed significantly lower PD-UESCI (377.60 ± 36.67vs517.14 ± 30.47 mmHg·s·cm,P=0.017), PECI (200.25 ± 39.18vs315.08 ± 30.24 mmHg·s·cm,P= 0.048) and PEL (4.43 ± 0.42vs5.75 ± 0.24 cm,P= 0.008) than patients without dysphagia. PEL was higher in patients with retrosternal pain,compared to patients without the symptom (6.43 ± 0.46vs 5.23± 0.24 cm,P= 0.046) (Figure 3).
Predictors of EGJOO
The ROC analysis discovered HRM parameters that helped identify EGJOO (Table 4). The area under the curve (AUC) of LESP in predicting EGJOO is 0.85, with the optimal cutoff at 40.20 mmHg, yielding asensitivity of 68.2% and specificity of 85.1%. IRP on RDC achieved an AUC value of 0.81, with the optimal cutoff at > 10.75 mmHg and sensitivity and specificity of 50.0% and 98.5%, respectively.UESNP, PEL, and PECI showed the best predictive value for EGJOO, with cutoff values of 1.15 mmHg(AUC 0.66), 4.76 cm (AUC 0.67), 312.35 mmHg·s·cm (AUC 0.67), respectively.
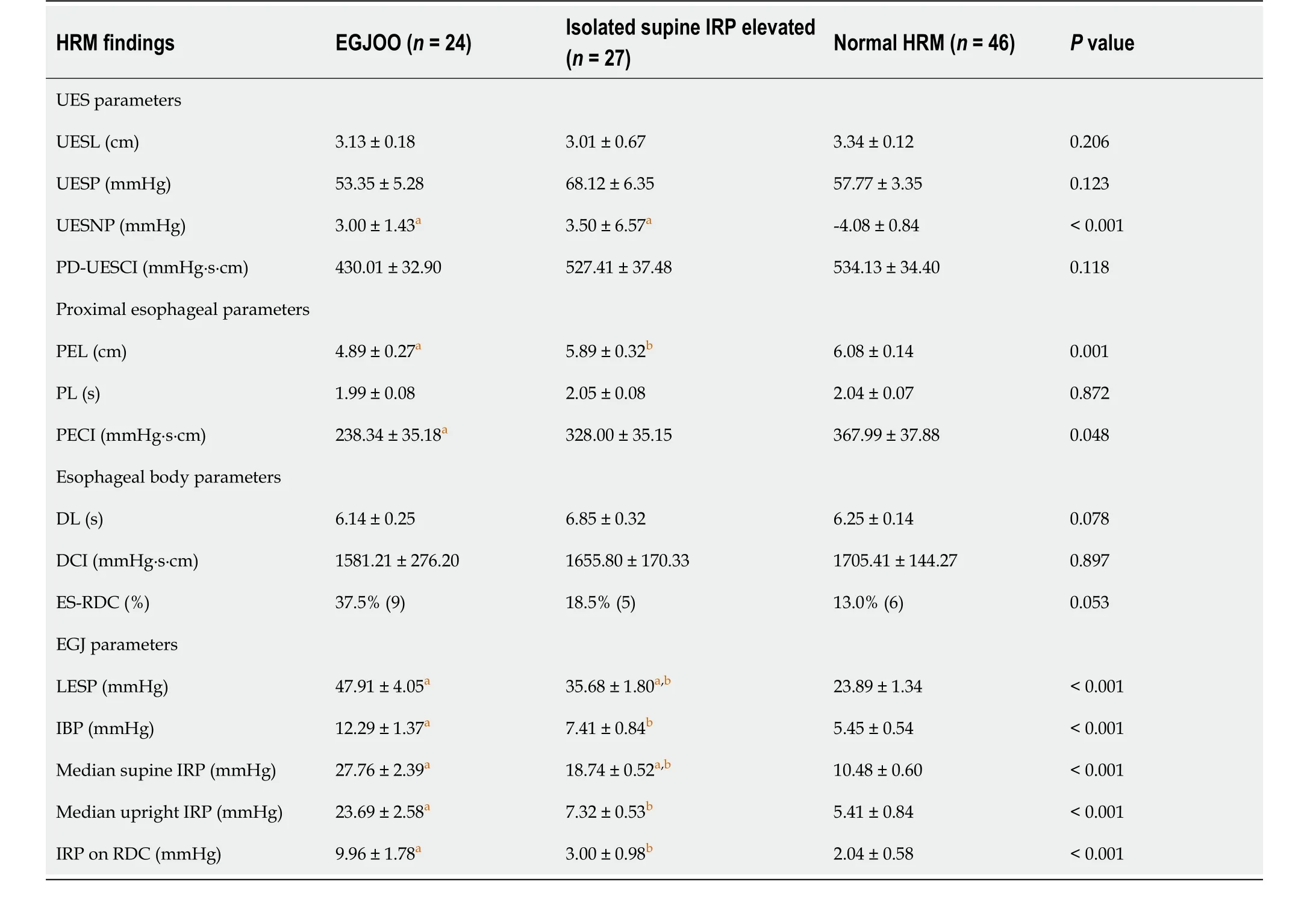
Table 2 High-resolution manometry parameters of the patients
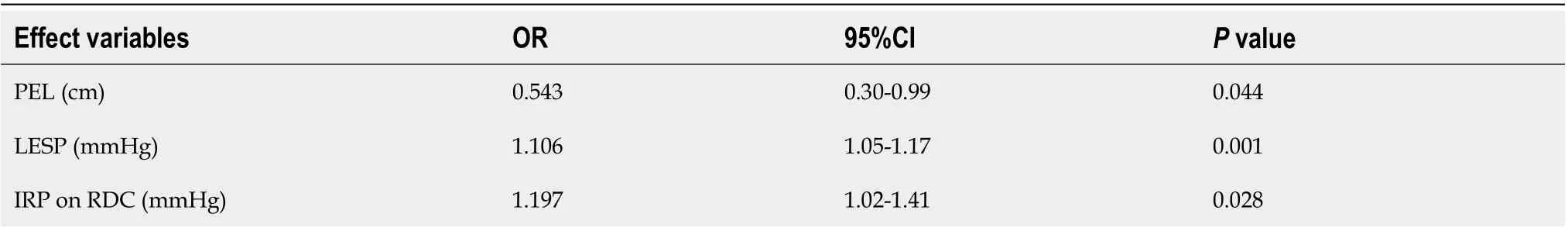
Table 3 Multivariate logistic regression analysis for factors associated with esophagogastric junction outflow obstruction
DlSCUSSlON
In this study, we mainly assessed the clinical and manometric characteristics of EGJOO based on the Chicago Classification version 4.0 (CCv4.0) to reveal potential changes in esophageal dynamics based onthe new diagnostic criteria, and we identified parameters that help distinguish the EGJOO.
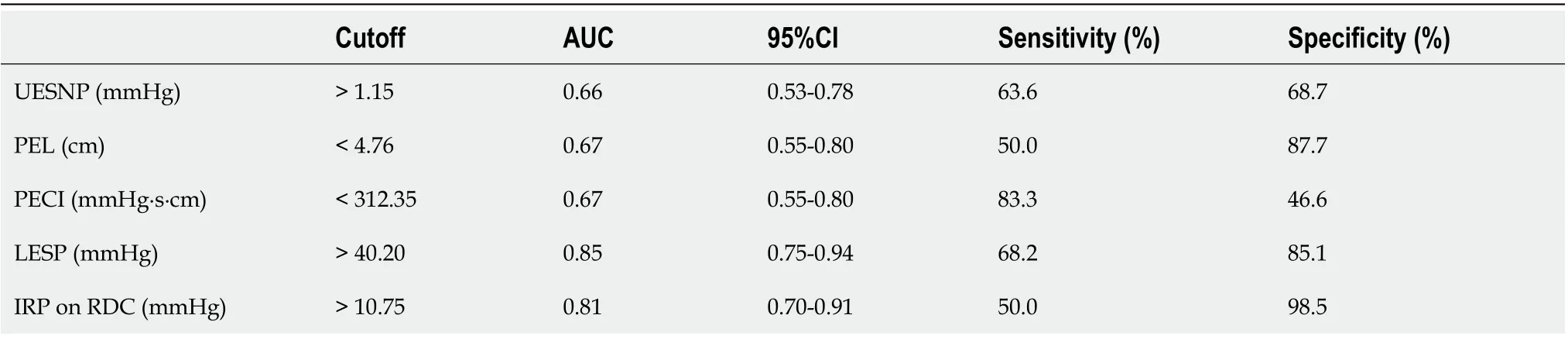
Table 4 Receiver-operating characteristic analysis for esophagogastric junction outflow obstruction
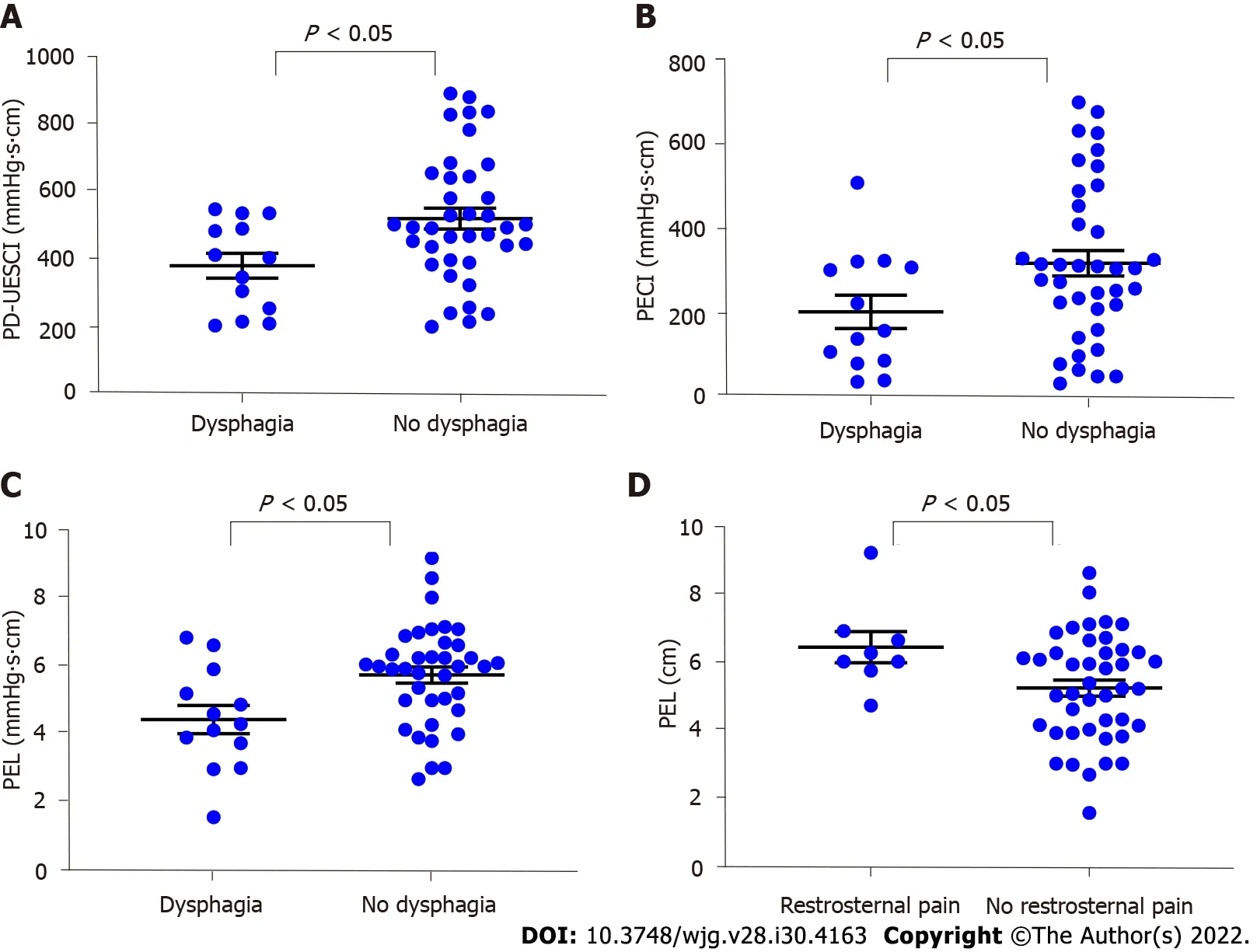
Figure 3 Comparisons of parameters according to symptoms in 51 patients with elevated integrated relaxation pressure. A: Patients with dysphagia showed lower postdeglutitive upper esophageal sphincter contractile integral than patients without dysphagia; B: Patients with dysphagia showed lower proximal esophageal contractile integral than patients without dysphagia; C: Patients with dysphagia showed lower proximal esophageal length (PEL) than patients without dysphagia; D: Patients with retrosternal pain showed higher PEL than patients without retrosternal pain. PD-UESCI: Postdeglutitive upper esophageal sphincter contractile integral; PECI: Proximal esophageal contractile integral; PEL: Proximal esophageal length.
Based on our observations, older people had a higher likelihood of being diagnosed with EGJOO according to manometric results. The EGJOO group showed no significant difference in symptom distribution pattern compared with the isolated supine IRP elevated group and the normal HRM group.Therefore, more manometric features and additional examinations are required for a better understanding of EGJOO.
The nadir UES residual pressure (UESNP) was reported to be higher in EGJOO (CCv3.0) than in normal controls[2,14]. Within EGJOO, higher UESNP was observed in motor disorders compared to mechanical etiologies and was a potential predictor of symptom recurrence after myotomy, with a cutoff level of 2 mmHg[2]. Based on our initial findings, patients with EGJOO and isolated supine IRP had significantly higher UESNP than the normal HRM group. The findings support the hypothesis that the UES is hypertonic with impaired relaxation, which may serve as a protective mechanism to facilitate esophageal clearance and prevent aspiration pneumonitis under IRP elevation[15]. Further ROC analysis revealed that UESNP elevation might serve as a feature for confirming EGJOO.
Previous studies have linked proximal esophageal motility abnormalities to achalasia[9]. The PECI of type 1 achalasia patients was weaker than that of healthy volunteers, but there was no difference between EGJOO (CCv3.0) and health volunteers, and patients with aberrant PECI had more severe upper gastrointestinal symptoms than patients with normal PECI[9]. It is worth noting that EGJOO(CCv4.0) group had weaker PECI than the normal HRM group, while patients with isolated IRP elevation had no difference compared to the normal HRM group. PECI resulted in a limited value for confirming the diagnosis of EGJOO. Furthermore, our findings suggest that PEL is lower in patients with EGJOO than patients with isolated elevated supine IRP or normal HRM, which might also serve as a feature that strengthens the confidence in an EGJOO diagnosis. The above results indicate that based on the updated criteria, EGJOO dysfunction may involve the proximal esophagus, while patients with isolated supine IRP elevated had no such features. It is reasonable to speculate that patients with EGJOO have common changes in proximal esophageal dynamic features, although further studies are required to reveal the underlying pathophysiological mechanism.
With our current analysis of symptoms, postdeglutitive contraction of the UES and proximal esophagus were weaker, and PEL was significantly lower in patients with dysphagia compared to patients without the symptom, indicating that in patients with impaired EGJ relaxation, dysphagia may represent a potential dysfunction of the UES and proximal esophagus.
Esophageal shortening has been proposed as an outcome of longitudinal muscle contraction, and esophageal shortening during the rapid drink test was mainly associated with impaired EGJ relaxation or major peristalsis disorders, particularly achalasia[12]. In our study, the incidence of ES-RDC had a marginal difference between the three groups, which is comparable with the motor pattern observed in achalasia.
In this study, LESP increased progressively from normal HRM to the isolated supine IRP elevated and EGJOO groups, with significant differences between groups. LESP was critical in the evaluation of EGJ obstruction. Furthermore, ROC curve analysis revealed that LESP had the highest differential diagnostic efficacy of EGJOO, indicating that the value of LESP is helpful in the assessment of EGJOO.
CCv4.0 also highlights the role of ancillary manometric evaluations, such as RDC, to identify the causes of symptoms and elicit evidence of obstruction. Our study performed IRP on RDC, which was significantly higher in the EGJOO group than in other groups, while the isolated supine IRP elevated group showed no difference compared with the normal HRM group, indicating that Chicago Classification updates filtered out EGJ dysfunction with more severe obstruction. It is worth noting that IRP on RDC greater than 12 mmHg (Medtronic software) indicates achalasia and may correlate with symptom severity[1,13,16]. The ROC analysis revealed that a high IRP on RDC is useful for confirming the diagnosis of EGJOO with high specificity (98.5%), but low sensitivity (50.0%).
Based on CCv3.0, a significant proportion of EGJOO is associated with the effect of artifact, hiatal hernia, mechanical obstruction, opioid effect, or gastric volvulus, but not primary LES dysfunction.Hence, numerous studies focused on the identification of primary motility disorders and excluded motility patterns secondary to medication use, mechanical obstruction, previous surgery, or endoscopic interventions[3,4,17], which are critical in making appropriate therapeutic decisions. Since the morphology of LES is affected by position, the CCv4.0 defines IRP in the upright position and IBP; thus,the Chicago Classification update has reduced the number of clinically irrelevant diagnoses and improved the specificity for EGJOO diagnosis[7,17,18], enabling us to avoid irreversible treatment for these conditions. According to the results of this study, patients with EGJOO had multiple abnormalities in EGJ parameters compared with the isolated supine IRP elevated group, including LESP, IBP, median supine IRP, median upright IRP, and IRP on RDC, implying that the Chicago Classification update aids in the selection of EGJOO with more severe EGJ dysfunction.
Due to the limitations of the retrospective study, our study lacked data on treatment and outcomes of patients, larger cohorts are required to explore the prognostic value of the parameters mentioned above.Based on CCv4.0, additional provocative tests such as solid test swallows, or pharmacologic provocation were recommended, and complementary tests are required for a conclusive, actionable diagnosis of clinically relevant EGJOO, while our study did not include the tests mentioned above and mainly focused on the changes in the manometric diagnosis of EGJOO. Moreover, it is necessary to further investigate the pathophysiological mechanism of the changes in proximal esophageal motility of patients with EGJOO.
CONCLUSlON
Conclusively, our current analysis revealed that patients with EGJOO had multiple changes in esophageal parameters based on Chicago Classification updates, especially more severe dysfunction at the esophagogastric junction than the previous diagnostic criteria, and showed multiple abnormalities at the proximal esophagus. The results illustrate that EGJOO is implicated in the proximal esophagus,and Chicago Classification updates improved the specificity for EGJOO diagnosis. Accordingly, we have expanded the valuable parameters for confirming the diagnosis of EGJOO based on CCv4.0,including UESNP, PEL, PECI, LESP, and IRP on RDC. With the advancement of EGJOO research, more contributions will be provided to the diagnosis and treatment of this type of disorder.
ARTlCLE HlGHLlGHTS
FOOTNOTES
Author contributions:Li YY and Lu WT contributed equally to this work; Li YY, Lu WT, and Jiao HM conception and designed of research; Li YY and Lu WT analyzed data; Lu WT and Chen M performed the HRM and provided clinical information; Li YY, Liu JX, and Jiao HM interpreted of research; Li YY drafted manuscript; Jiao HM revised manuscript and approved the final version of manuscript; all authors approved the final version of the article.
Supported bythe China Central Health Research Fund, No. W2013BJ29; and the Interdisciplinary Clinical Research Project of Peking University First Hospital, No.2019CR40.
lnstitutional review board statement:This study was reviewed and approved by the Institutional Review Board of the Peking University First Hospital, No. 2022-099.
lnformed consent statement:A waiver of informed consent was granted by our Institutional Review Board because our retrospective analysis used completely anonymized data.
Conflict-of-interest statement:All authors have declared no conflicts of interest.
Data sharing statement:Data sharing available, please require through email.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Yue-Yuan Li 0000-0003-4973-8906; Wen-Ting Lu 0000-0002-6483-8342; Jian-Xiang Liu 0000-0003-0196-6459; Li-Hong Wu 0000-0002-2885-7482; Meng Chen 0000-0002-7882-008X; Hong-Mei Jiao 0000-0002-9139-9744.
Corresponding Author's Membership in Professional Societies:Association of Digestive Disease, Chinese Geriatrics Society.
S-Editor:Yan JP
L-Editor:A
P-Editor:Yan JP
 World Journal of Gastroenterology2022年30期
World Journal of Gastroenterology2022年30期
- World Journal of Gastroenterology的其它文章
- Role of one-step nucleic acid amplification in colorectal cancer lymph node metastases detection
- Current perspectives on the role of liver transplantation for Langerhans cell histiocytosis: A narrative review
- Gut microbiota, inflammatory bowel disease and colorectal cancer
- Thrombocytopenia in chronic liver disease: Physiopathology and new therapeutic strategies before invasive procedures
- P2X7 receptor blockade decreases inflammation, apoptosis, and enteric neuron loss during Clostridioides difficile toxin A-induced ileitis in mice
- Serological profiling of Crohn’s disease and ulcerative colitis patients reveals anti-microbial antibody signatures
