Cumulative incidence and risk factors for pouch adenomas associated with familial adenomatous polyposis following restorative proctocolectomy
Hyo Seon Ryu, Chang Sik Yu, Young Il Kim, Jong Lyul Lee, Chan Wook Kim, Yong Sik Yoon, In Ja Park,Seok-Byung Lim, Jin Cheon Kim
Abstract
Key Words: Adenomatous polyposis coli; Familial adenomatous polyposis; Adenoma; Intestinal polyps;Proctocolectomy, restorative; Ileal pouch anal anastomosis
lNTRODUCTlON
Familial adenomatous polyposis (FAP) is a genetic syndrome caused by an adenomatous polyposis coli(APC) gene mutation that has an incidence of 1 in 10000 births[1]. This genetic variation is characterized by extensive polyposis in the colon and rectum, and patients with FAP have a lifetime colorectal cancer risk of 100% by the age of 35 to 40 years[2]. Hence, prophylactic surgical intervention is required for these individuals, and the currently favorable therapeutic option is a total proctocolectomy and ileal pouch-anal anastomosis (TPC/IPAA)[2]. TPC/IPAA increases life expectancy among patients with FAP by eliminating their metachronous colorectal cancer risk[3]. The postoperative disease course is determined by extracolonic manifestations, including duodenal adenoma and carcinoma, and desmoid tumors[4].
Cancers of the terminal ileum are extremely rare, and this region thus represents a far lower disease risk than the remaining rectal mucosa after ileorectal anastomosis. Notably, however, several studies have found a 35%-57% incidence of ileal pouch adenomas associated with FAP, which can progress to malignancy[5-11]. Given that most of these prior studies involved small sample sizes and were retrospective in nature, definitive results on these cancers are lacking, and the risk factors associated with pouch adenoma development remain to be established. Although these data are limited, the pouch adenoma incidence is reported to be quite high; therefore, long-term periodic surveillance is required.Most clinical guidelines recommend annual endoscopic surveillance of the anal transition zone (ATZ)mucosa after TPC/IPAA as a surgical management strategy for FAP patients. According to the National Comprehensive Cancer Network guidelines, this surveillance interval should be shortened to 6 mo if the adenoma is large or has advanced histology. However, there are currently no specific criteria directing more frequent surveillance. Moreover, with the currently implemented management approaches for pouch adenoma, uncertainty remains regarding the specific indications for endoscopic or surgical intervention[12-14]. More information is, therefore, needed regarding the incidence, natural course, and risk factors associated with pouch adenoma.
We investigated the cumulative incidence and time to development of pouch adenomas. In an FAP cohort after TPC/IPAA, we analyzed the clinical factors associated with pouch adenoma development.
MATERlALS AND METHODS
Study sample
Data on all patients with FAP who underwent pouch surgery at Asan Medical Center, Seoul, South Korea between November 1989 and December 2018 were identified from the hospital database. The FAP patients were identified by the presence of more than 100 colorectal adenomas. The indication for TPC/IPAA was FAP with or without malignancy. We excluded patients with attenuated FAP with fewer than 100 polyps (as per histopathology reports), as well as patients who did not receive TPC/IPAA. Demographic data, surgical details, original histopathology, and details of follow-up pouch endoscopic and pathologic findings were captured retrospectively. The definition of pouch adenoma included lesions that occurred in the ileum above the anastomosis site. Pouch adenoma progression was defined as an increase in the number or size of these lesions, as well as the development of dysplasia or malignancy, evident on histopathological examination. The severity of the duodenal polyposis in each case was assessed using the Spigelman classification[15] (Table 1). The study protocol was approved by the institutional review board of Asan Medical Center (registration No. 2021-0309) in accordance with the Declaration of Helsinki.
Surgical techniques of IPAA
An anal mucosectomy leaving a short rectal muscular cuff above the dentate line and transanal handsewn ileoanal anastomosis were performed for 72 of our enrolled FAP patients (75.8%). The remaining 23 patients (24.2%) underwent double-stapled anastomosis adjacent to the dentate line at the ATZ. The pouch construction in all patients was J-shaped using two ileal limbs of 15 cm in length.
Follow-up protocols
The regular follow-up protocols for our study patients included clinical examinations, pouch and upper gastrointestinal endoscopy, and abdominoperineal computed tomography. Pouch endoscopy was performed within 1 postoperative year. Subsequently, for patients who underwent a mucosectomy,endoscopic examinations were performed once every 2 years in the absence of any polyps. If polyps were observed during endoscopic follow-up, they were removed regardless of size. In patients with multiple polyps, those larger than 5 mm in diameter were removed, or a biopsy specimen was collected.More intensive follow-up was performed, at intervals of 6-12 mo, if warranted by the size, number, or pathologic characteristics of identified polyps. Patients with colorectal cancer in our cohort were followed at 6-mo intervals for 5 years and annually thereafter. Additionally, testing for carcinoembryonic antigens was conducted every 6 mo, and chest computed tomography was performed annually.
Statistical analysis
The quantitative variables in this study are expressed as medians with interquartile ranges (IQRs) or ranges, and categorical variables are summarized as frequencies and percentages. The clinicopathological variables for the patients with and without pouch adenomas were compared using the Kruskal-Wallis test and Fisher’s exact test. The time to pouch adenoma formation was defined as the time from the date of surgery to the date of detection of the first histologically confirmed adenoma. Pouch adenoma-free survival was calculated using the Kaplan-Meier method. Multivariate Cox regression analysis based on backward elimination was used to assess the impact of variables on pouch adenoma-free survival with adjustment for variables reported to be associated with pouch adenoma-free survival in previous reports (colorectal polyp burden, time interval after IPAA, presence of desmoid tumors, and presence of gastric polyps and duodenal adenomas) in addition to basic patient characteristics, such as age and sex. Hazard ratios (HRs) with 95% confidence intervals (CIs) were also calculated. Statistical significance was established with a two-sided test atP< 0.05. All statistical analyses were performed using SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY,United States).
RESULTS
A total of 175 patients with FAP who underwent pouch surgery were identified from the hospital database. Among these patients, we excluded 48 with attenuated FAP with fewer than 100 polyps according to histopathology reports. We also excluded six patients who underwent total colectomy procedures with ileorectal anastomosis, two who underwent end-ileostomy without ileal pouches, and one whose pouch was removed due to postoperative bleeding. We further excluded 23 patients who did not undergo postoperative follow-up sigmoidoscopy. The final study cohort, thus, comprised 95 patients with FAP who underwent TPC/IPAA (Figure 1).
The characteristics of the 95 FAP patients enrolled in this study are summarized in Table 2. The median follow-up period after pouch surgery was 88 mo (IQR, 61-141 mo). The median age at the time of IPAA was 32 years (IQR, 24-41 years). The median number of follow-up endoscopies was 5 (IQR, 3-7).We observed that 24 (25.3%) of our study patients had adenomas that had been histologically confirmed in the pouch mucosa above the anastomosis. The median time to first pouch adenoma detection was 52 mo (IQR, 28.3-114.3 mo). Adenomas arising from the ATZ below the anastomosis were detected in seven (7.4%) patients. Upper gastrointestinal endoscopy was also performed for all patients. Gastric polyps were present in 70 (73.3%) patients; these were mainly fundic gland polyps (75.7%) as per biopsy results. Duodenal adenomas were confirmed in 46 (48.5%) patients. Twenty-four, 12, and 10 patients were classified as having Spigelman stages I, II, and III lesions, respectively, and there were no stage IV cases. Twenty-three (24.2%) patients developed desmoid tumors. At the time of surgery, 43 (45.3%)patients had colorectal cancer.
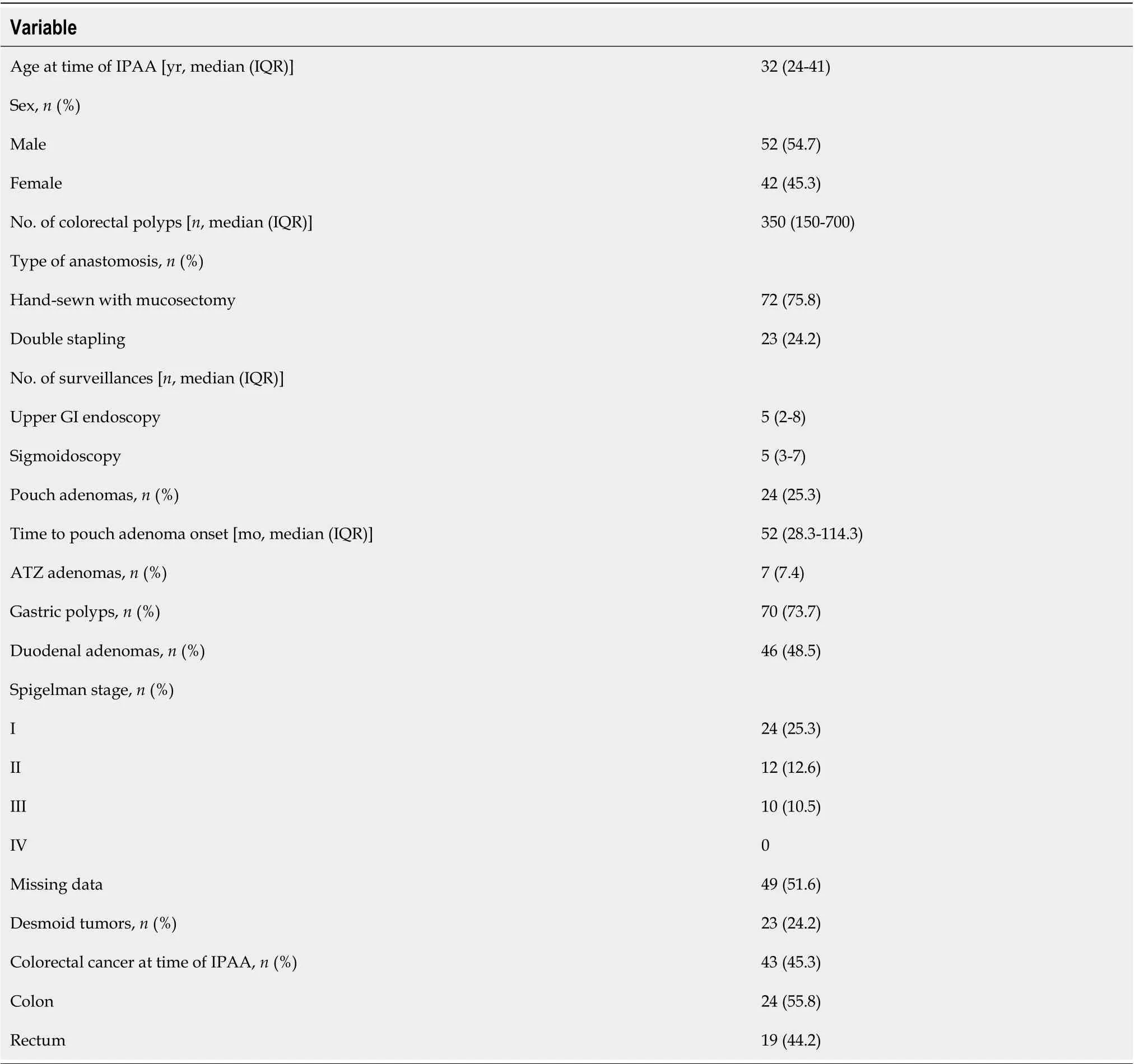
Table 1 Characteristics of familial adenomatous polyposis patients analyzed in this study
Mutation analysis
Information on the underlying germline mutation was available for 40 (42.1%) FAP patients, among whom 28 (70.0%) harboredAPCmutations, most commonly within exon 15 of theAPCgene (64.3%). No significant difference was found in terms of the distribution of germline mutations between patients with and without pouch adenomas (P= 0.21).
Presence and distribution of pouch adenomas
The cumulative incidences of pouch adenomas at 5, 10, and 15 years after IPAA were 15.2%, 29.6%, and 44.1% (95%CI: 7.2%-22.4%, 15.8%-41.1%, and 25.3%-58.2%), respectively (Figure 2). Among the 24patients with pouch adenomas, 13 (54.2%) had fewer than 12 countable lesions, whereas others had numerous polyps within the pouch. All countable adenomas were removed endoscopically regardless of size. Only one patient had to undergo a transanal excision to remove a pouch adenoma 31 mm in diameter. The median value of the maximum diameter was 3 mm (range, 2.0-31.0 mm). Tubular adenomas were detected in 23 (95.9%) patients, and tubule-villous adenomas were detected in two(8.4%) patients. There were no cases of high-grade dysplasia or malignancy in our study sample. During follow-up for the 13 patients who underwent complete removal of all detected adenomas, eight (61.5%)patients had no recurrence, and four (38.5%) developed recurrent adenomas, which were endoscopically resected. The remaining patient in this group was lost to follow-up, and the disease course after adenoma removal was not documented. For the 11 (45.8%) patients with numerous polyps within the pouch, only those larger than 5 mm were removed, and surveillance biopsy specimens were collected.In four (36.4%) patients, the adenomas remained unchanged, while seven (63.6%) patients exhibited pouch adenoma progression (Figure 3).
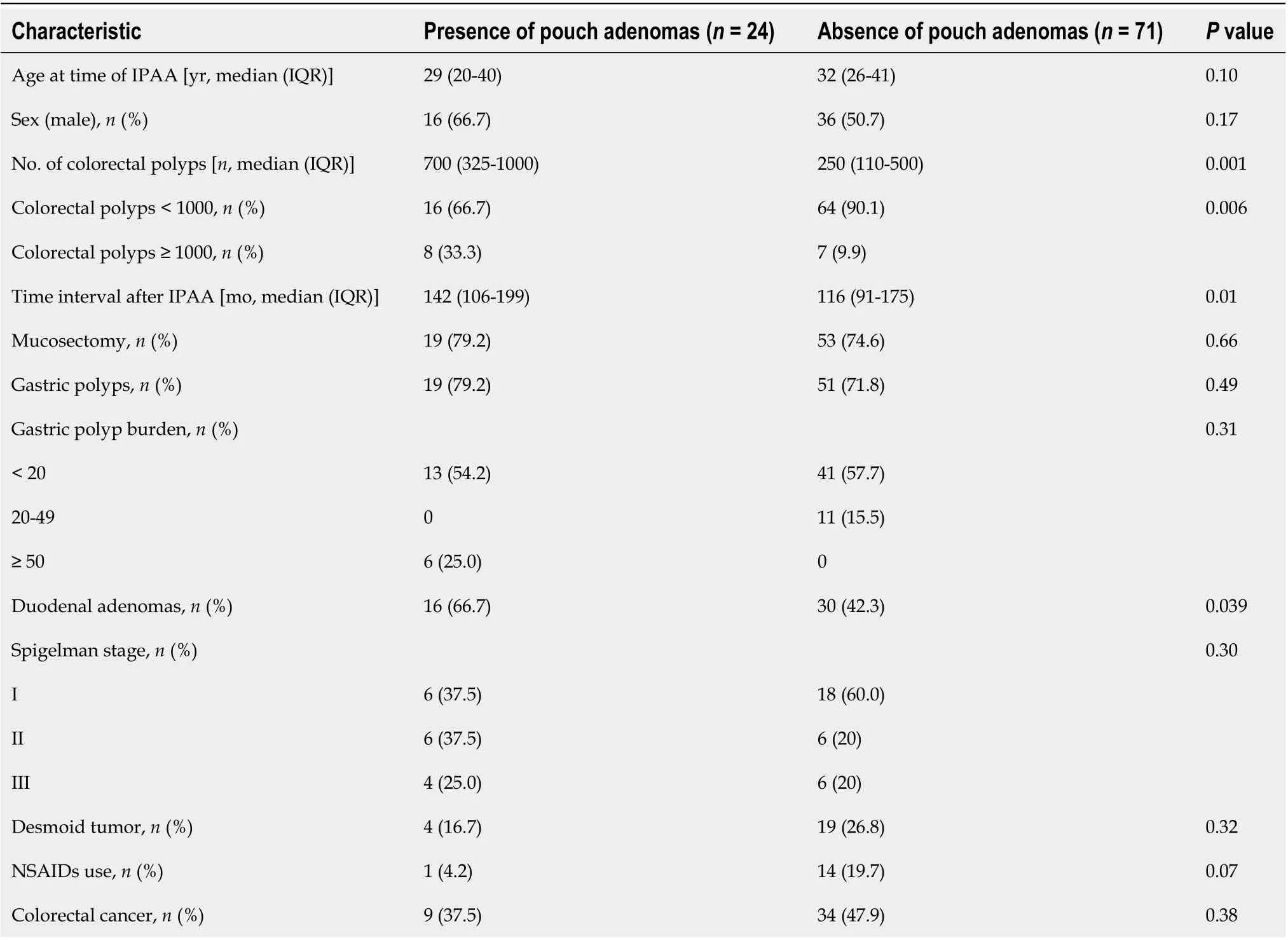
Table 2 Clinical characteristics of study patients according to presence of pouch adenomas
Clinical characteristics of study patients with and without pouch adenomas
Comparisons of the clinical characteristics among the FAP patients according to the presence of pouch adenomas are presented in Table 2. Compared with patients without adenomas, the pouch adenoma group had a significantly higher mean number of colorectal polyps at the time of surgery (700vs250,P= 0.001). Severe polyposis involving more than 1000 colorectal polyps was also significantly more common in the pouch adenoma group (P= 0.006). Additionally, patients with pouch adenomas (relative to those without pouch adenomas) were more likely to have duodenal adenomas (66.7%vs42.3%,P=0.039). There was no significant intergroup difference in the Spigelman adenoma stage distributions (P=0.30) and no differences in the gastric polyp status (absent or present) or gastric polyp burden.Nonsteroidal anti-inflammatory drug (NSAID) treatment for desmoid tumors-including with celecoxib and meloxicam-was more common among patients without pouch adenomas, but this difference was not statistically significant (4.2%vs19.7%,P= 0.07). There were no differences between the clinical characteristics of the study patients when stratified by the presence of colorectal cancer at the time of surgery (P= 0.38).
Associations between different clinical factors and pouch adenoma-free survival
Associations between different patient factors and pouch adenoma-free survival were evaluated(Table 3). Among the clinical factors analyzed, multivariate analysis revealed severe colorectal polyposis(with more than 1000 polyps) to be a significant risk factor for pouch adenoma development (HR, 2.49;95%CI: 1.04-5.96;P= 0.041) (Figure 4). The presence of gastric polyps or a duodenal adenoma had no significant association with pouch adenoma development (P= 0.28 and 0.54, respectively).
DlSCUSSlON
TPC/IPAA is now being implemented as a standard treatment to eliminate the risk of colorectal cancer in patients with FAP. However, the postoperative development of adenomas in the ileal pouch in these individuals has raised new concerns about appropriate postoperative surveillance and management approaches. In this study cohort, the incidence of pouch adenoma was 25.3% at a median follow-up of 88 mo (IQR, 61-141 mo) after IPAA. The cumulative risk of pouch adenoma was 15.2%, 29.6%, and 44.1% at 5, 10, and 15 years after TPC/IPAA, respectively. There were no cases of high-grade dysplasia or carcinoma in our cohort. We found that a higher colorectal polyp burden at the time of surgery was positively associated with the occurrence of pouch adenoma formation (P= 0.001). These results are consistent with the findings reported in prior studies[9,10,16-18].
Several potential risk factors associated with pouch adenoma development have been investigated previously, but they remain controversial. Consistent with the findings of Tonelliet al[10], we found inour present analyses that a high colorectal polyp count at the time of IPAA was positively associated with pouch adenoma development. This result is likely to be assumed to be more aggressive disease.However, other authors have not observed an association between the severity of colonic disease and development of pouch adenoma[5].
Mutations of theAPCgene predispose the carrier to benign polyps and malignancies in the upper gastrointestinal tract. Therefore, the risk of developing small bowel adenomas remains in these individuals even after TPC/IPAA. In this context, gastric or duodenal adenomas may be relevant to development of pouch adenoma. Ganschowet el[9] analyzed these variables previously and found that the presence of a gastric adenoma was a significant risk factor for developing a pouch adenoma (P=0.0019). Several investigator groups have also reported that the presence of a duodenal adenoma is associated with pouch adenoma formation[10,16]. Tonelliet al[10] observed that the severity of duodenal polyposis was also relevant in this regard. As with the findings of other studies, our experience has been that patients who develop pouch adenomas are more likely to have had duodenal adenomas, although this was not observed to be a significant risk factor in our present multivariate analysis.
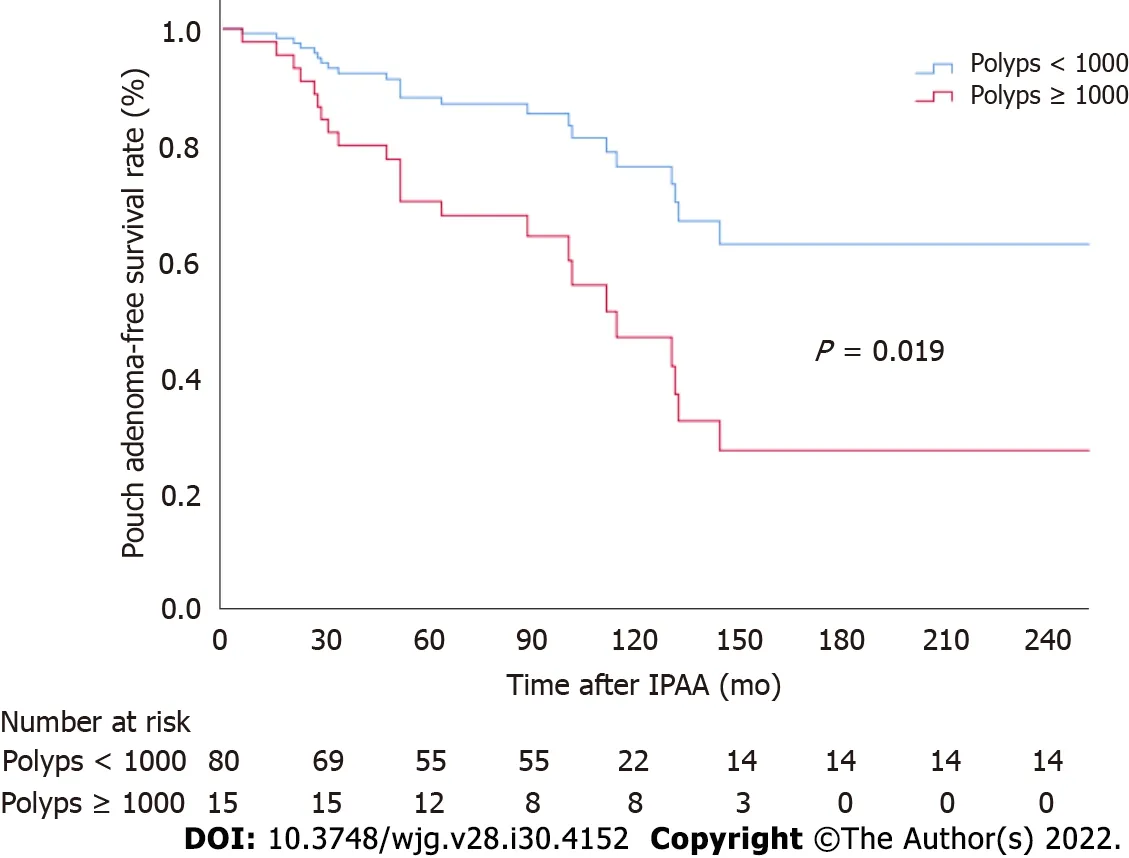
Figure 4 Pouch adenoma-free survival according to colorectal polyp burden at the time of ileal pouch-anal anastomosis. IPAA: Ileal pouchanal anastomosis.
There has been little research conducted on the association between the site of anAPCmutation and the occurrence of pouch adenoma. No such association has been identified in earlier studies[9,10,16],nor was such an association identified in our present analysis. However, in previous reports and in our present series,APCmutation data were not available for all subjects. Moreover, the low number of patients who underwent this mutation analysis in our present series and in prior study cohorts could not yield the statistical power needed to determine whether theAPCmutation site is associated with the tendency to develop pouch adenomas. Additionally, a recently published study of genotype-phenotype associations betweenAPCmutations and pouch adenomas found that patients with either indel/deletion mutations or exon 15 mutations had a higher tendency for pouch adenoma formation (P= 0.002 and 0.019, respectively)[19]. Hence, further larger-scale research is required to investigate the association between underlying germline mutations and pouch adenoma development.
Several authors have implicated colonic metaplasia of the ileal mucosa-an adaptive response of the neorectum-as a predisposing condition to the onset of ileal adenoma development[20]. Advanced adenomas with high-grade dysplasia were observed in about 18% of previous study samples[5,18].However, no case of an advanced adenoma was detected in our present study cohort, possibly because adenomas were aggressively removed from our patients, even if small. If ileal pouch adenomas progress to carcinoma, following the classic adenoma-carcinoma sequence, a higher number and larger size of polyps may be associated with the severity of the dysplasia. Tajikaet al[18] reported that the postoperative time interval was significantly associated with the maximum ileal pouch adenoma size (P=0.0214). Progression of a pouch adenoma to invasive carcinoma appears to be rare, with an incidence of less than 1% in patients that undergo IPAA[8,9,19]. Moreover, the majority of carcinomas observed after IPAA arise in the residual rectal mucosa or anal canal, although several cases of carcinoma inside the ileal pouch have been described in the past few years[18]. Tonelliet al[10] found that the development of malignancy in the terminal ileum can present with a rapid disease course and does not seem to follow the classic adenoma-carcinoma sequence. In some patients, ileal polyps are not detected by endoscopic follow-up until the development of a pouch carcinoma, and the mean interval between pouch construction and the diagnosis of carcinoma can be very short (range, 3-16.4 years).
Clinically, the treatment of pouch adenomas depends on the number, size, shape, and histological features-as for the gastric or duodenal polyps. According to the American Society for Gastrointestinal Endoscopy and British Society of Gastroenterology guidelines, all types of gastric or duodenal polyps detectedviaendoscopy need to be sampled using biopsy forceps for evaluation[21-23]. In the case of adenomatous polyps, these guidelines recommend complete endoscopic removal when it is safe to do so, given the higher probability of malignant transformation[22,23]. Endoscopic follow-up should be repeated at 6 mo for incompletely resected polyps or for those with high-grade dysplasia; it can be conducted again at 12 mo for all other polyps[22]. Although the data are currently limited, 62% of our cohort did not develop adenoma recurrence after adenoma removal, whereas 63% of our patients under observation showed progression. There was no spontaneous diminution or disappearance of any adenoma in our study cohort. Hence, it is important to be aware of the risk of pouch neoplasia when caring for FAP patients after IPAA, and-to enable evaluation and treatment at the same time-we recommend endoscopic resection when the adenoma is detected. If numerous polyps are present,random biopsy sampling is required, and polyps larger than 5 mm should be removed.
Interestingly, our FAP patients who used NSAIDs as a treatment for desmoid tumors rarely developed pouch adenomas. This finding is presumed to be related to the chemopreventive effect of these drugs. Chemoprevention with NSAIDs is a treatment option considered to facilitate the management of the remaining rectum or pouch in selected postoperative patients[13]. In a prior randomized controlled study, patients with FAP and attenuated FAP treated with celecoxib following prophylactic surgery showed reductions in polyp number and diameter[24]. NSAIDs may thus be considered if not all of the numerous polyps within the pouch can be removed, although there are currently no Food and Drug Administration-approved drugs for this indication.
There were some limitations to this study. First, this was a retrospective cohort study with a small sample size, and there may have been unknown confounders. However, as we were investigating a rare disease, there have been few studies to date that have analyzed a substantial number of affected patients. Therefore, in relative terms, our sample size was large, and the patients were followed for a considerable length of time. A second limitation was that whereas all of the patients had a clinical phenotype of 100 or more colorectal polyps and biopsy-confirmed FAP,APCgenetic mutation analysis was only performed for about 50% of the patients. This limited the strength of our findings related to these mutations. Additionally, there was no consistent endoscopic treatment standard in our cohort.When a polyp was countable, it was removed regardless of its size. In patients with multiple polyps,however, the individual judgment of the endoscopist determined whether to perform endoscopic resection or observation. The indications used for polyp removal were, therefore, not clear.
Overall, our study findings provide further evidence for the need for standardized endoscopic surveillance of FAP patients following TPC/IPAA. Pouch endoscopy should be performed yearly for these patients, and standardized biopsy and removal protocols are needed if pouch adenomas are observed. Furthermore, surveillance should be tailored depending on the presence and characteristics of the pouch adenoma. In the future, validation of whether an annual endoscopic interval is appropriate is required, as is an evaluation of the feasibility and effectiveness of endoscopic resection of a pouch adenoma.
CONCLUSlON
In conclusion, pouch adenomas occur at a fairly high rate over time in association with FAP after IPAA.A high colorectal polyp count increases the risk of developing a pouch adenoma in this patient population. In our experience, the progression of pouch adenomas to high-grade dysplasia or carcinoma is rare. However, this risk is not negligible, and the long-term risk of this cannot presently be well quantified. Close surveillance of the pouch should thus be mandatory, and new guidelines for the management of pouch adenomas are essential.
ARTlCLE HlGHLlGHTS
significant risk factor for pouch adenoma development (hazard ratio, 2.49; 95% confidence interval:1.04-5.96;P= 0.041).
Research conclusions
We recommend endoscopic resection when the adenoma is detected. If numerous polyps are present,random biopsy sampling is required, and polyps larger than 5 mm should be removed. Close surveillance of the pouch should be mandatory, and new guidelines for the management of pouch adenomas are required.
Research perspectives
In the future, validation of whether an annual endoscopic interval is appropriate is required, as is an evaluation of the feasibility and effectiveness of endoscopic resection of a pouch adenoma.
FOOTNOTES
Author contributions:Ryu HS designed and performed the research and wrote the paper; Yu CS designed the research and supervised the report; Kim YI, Lee JL, Kim CW, Yoon YS, Park IJ, Lim SB, and Kim JC provided clinical advice and supervised the report.
lnstitutional review board statement:The protocol for this research project has been approved by a suitably constituted ethics committee of the institution (Committee of Asan Medical Center, Approval No. 2021-0309), and it conforms to the provisions of the Declaration of Helsinki.
lnformed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:This study did not receive a specific grant from any funding agency in the public,commercial, or not-for-profit sectors.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:South Korea
ORClD number:Hyo Seon Ryu 0000-0003-2606-9973; Chang Sik Yu 0000-0001-9401-9981; Young Il Kim 0000-0002-0212-9196; Jong Lyul Lee 0000-0002-5878-8000; Chan Wook Kim 0000-0002-2382-0939; Yong Sik Yoon 0000-0002-3196-8423; In Ja Park 0000-0001-5355-3969; Seok-Byung Lim 0000-0001-8824-4808; Jin Cheon Kim 0000-0003-4823-8619.
S-Editor:Yan JP
L-Editor:Wang TQ
P-Editor:Yan JP
 World Journal of Gastroenterology2022年30期
World Journal of Gastroenterology2022年30期
- World Journal of Gastroenterology的其它文章
- Role of one-step nucleic acid amplification in colorectal cancer lymph node metastases detection
- Current perspectives on the role of liver transplantation for Langerhans cell histiocytosis: A narrative review
- Gut microbiota, inflammatory bowel disease and colorectal cancer
- Thrombocytopenia in chronic liver disease: Physiopathology and new therapeutic strategies before invasive procedures
- P2X7 receptor blockade decreases inflammation, apoptosis, and enteric neuron loss during Clostridioides difficile toxin A-induced ileitis in mice
- Serological profiling of Crohn’s disease and ulcerative colitis patients reveals anti-microbial antibody signatures
