Altered gut microbiota patterns in COVID-19: Markers for inflammation and disease severity
Chiranjib Chakraborty,Ashish Ranjan Sharma, Manojit Bhattacharya, Kuldeep Dhama, Sang-Soo Lee
Abstract The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection leads to a severe respiratory illness and alters the gut microbiota, which dynamically interacts with the human immune system. Microbiota alterations include decreased levels of beneficial bacteria and augmentation of opportunistic pathogens. Here, we describe critical factors affecting the microbiota in coronavirus disease 2019 (COVID-19) patients. These include, such as gut microbiota imbalance and gastrointestinal symptoms, the pattern of altered gut microbiota composition in COVID-19 patients, and crosstalk between the microbiome and the gut-lung axis/gut-brain-lung axis. Moreover, we have illustrated the hypoxia state in COVID-19 associated gut microbiota alteration.The role of ACE2 in the digestive system, and control of its expression using the gut microbiota is discussed, highlighting the interactions between the lungs, the gut, and the brain during COVID-19 infection. Similarly, we address the gut microbiota in elderly or co-morbid patients as well as gut microbiota dysbiosis of in severe COVID-19. Several clinical trials to understand the role of probiotics in COVID-19 patients are listed in this review. Augmented inflammation is one of the major driving forces for COVID-19 symptoms and gut microbiome disruption and is associated with disease severity. However, understanding the role of the gut microbiota in immune modulation during SARS-CoV-2 infection may help improve therapeutic strategies for COVID-19 treatment.
Key Words: COVID-19; Inflammation; Gut microbiota; Therapeutic
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic has stimulated research on several medical conditions and on individual patient variations during severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) infection to unfold underlying disease mechanisms. Scientists have determined the inflammatory response and cellular injury mediated by acute SARS-CoV-2 infection. Moreover, several studies have revealed the involvement of the gastrointestinal (GI) tract and its associated gut microbiome during COVID-19, motivating research in this field. Increasing evidence has surfaced confirming the association of the GI tract and COVID-19, including[1,2] a severe state of gut dysbiosis in COVID-19 patients[3,4]. Similarly, GI symptoms such as vomiting, abdominal pain, and diarrhea have been noted in many COVID-19 patients[5-7]. Moreover, high expression of ACE2 receptor was reported in epithelial cells of the GI tract[8]. SARS-CoV-2 RNA has been identified in rectal and anal swabs, as well as stool specimens[7,9,10]. Finally, liver damage, loss of appetite, and irritable inflammatory diseases have been reported as post-COVID-19 illnesses[11]. These all data strongly indicate a correlation between the GI including the gut microbiome, and COVID-19.
The gut microbiota plays an important role in controlling gut health and acts as a health modulator(Figure 1)[12] aidings in different metabolic activities and extensively impacting health and disease[13,14]. Ongoing research aims to better understand the gut microbiota and provide insights into the mechanistic conditions required to implement normal health functions. The gut microbiota controls specific functions in the host, such as drug and xenobiotic metabolism and nutrient metabolism[15].Simultaneously, it helps maintain the structural integrity of the gut mucosal barrier, protects against pathogens, and regulates immunomodulation, as well as health and disease conditions[16,17]. Several other studies suggest a possible link between COVID-19 and gut microbiota composition[18,19].Additionally, an association has been shown between altered gut microbial composition and increased risk factors in COVID-19 patients (Figure 1)[20,21].
Inflammation is a major risk factor in COVID-19 patients[22-24]. During uncontrolled inflammation,abnormal levels of cytokines such as interleukin-1 beta (IL-1β), IL-6, IL-8, IL-10, IL-12, granulocytemacrophage colony-stimulating factor (GM-CSF), tumor necrosis factor-alpha (TNF-α), and interferongamma (IFN-γ) are found in the patients[23,25-27]. Certain abnormal levels of cytokines are substantial related to the severity of COVID-19 and are probably responsible for the “cytokine storm” syndrome manifested during the disease[28-30]. Research has correlated the inflammation during COVID-19 with GI and hepatic manifestations of the disease[31].
Interactions between the gut microbiota and the lungs, known as the gut-lung axis, have sparked interest for gastroenterology studies focusing on COVID-19 as these interactions affect disease severity.Changes in the gut microbiome certainly affect homeostasis and may lead to increased infections[32,33].Similarly, in addition to the gut, COVID-19 can also have a detrimental effect on the central nervous system (CNS) and the blood-brain barrier (BBB) and disrupt the gut-brain-lung axis. Studies have explored therapeutic options (nicotinic cholinergic agonists and vagus nerve stimulation) to minimize the damage caused to this axis[34].
Research is necessary to understand how the gut microbiome is altered during COVID-19 infection and the factors that influence the microbiome during mild to moderate and severe disease. Studies have been conducted to understand the GI symptoms during COVID-19 and to detect viral shedding using the fecal matter of SARS-CoV-2 patients. The gut microbiota of COVID-19 patients has been mapped to obtain evidence regarding inflammation, disease severity, and therapeutic development.

Figure 1 The schematic diagram shows normal healthy gut and the incidence in gut microbiota and gut virome in coronavirus disease 2019 patients. COVID-19: Coronavirus disease 2019.
Using these studies, we explore the following critical factors: (1) The gut microbiota imbalance and GI symptoms in COVID-19 patients; (2) fecal viral shedding in COVID-19 patients and restoration of the gut microbiota; (3) the pattern of altered gut microbiota composition in COVID-19 patients; (4)alterations in gut biosynthesis during COVID-19 infection; (5) the role of ACE2 in the digestive system and the gut microbiome; (6) crosstalk between the microbiome and the gut-lung axis during COVID-19 infection; (7) crosstalk between the microbiome and the gut-brain-lung axis during COVID-19 infection;and (8) hypoxia during COVID-19 associated with altered gut microbiota. We also discuss how immune responses and inflammation due to COVID-19 drive the changes in the microbial ecosystem and summarize therapeutic options currently in development.
GI SYMPTOMS IN COVID-19 PATIENTS
Along with respiratory symptoms and fever, GI symptoms have also been observed in COVID-19 patients (Table 1). A study by Reddet al[35] reported abdominal pain (14.5%), nausea (26.4%), diarrhea(33.7%), and vomiting (15.4%) in patients from the United States. Three hundred and eighteen hospitalized COVID-19 patients were evaluated to understand their symptoms. In another study with 204 COVID-19 patients, 50.5% (103 patients) exhibited GI symptoms. Among these 103 patients, 78.6%showed a lack of appetite, 34% had diarrhea, 3.9% vomited, and 1.9% complained of abdominal pain.The authors correlated patients describing GI symptoms with other measurements such as prothrombin time, monocyte count, and liver enzyme levels. Patients with GI symptoms had elevated mean liver enzyme levels, extended prothrombin times, and lower monocyte counts[36]. In a much larger cohort study involving 1099 COVID-19 patients from 552 different hospitals spread to over 30 provinces, only 3.8% of patients experienced diarrhea. The authors concluded that fever and cough are common symptoms, unlike diarrhea, among the COVID-19 patient population[37].
These findings suggest that the virus might be present for a period in the GI tract, which may cause a GI infection (Figure 2). Importantly, fecal viral shedding was noted after clearing SARS-CoV-2 from the respiratory tract, suggesting that the virus can persist for a long time in the GI tract, especially in patients who manifest GI symptoms. During COVID-19 infection, gut microbiota composition is altered,possibly explaining the GI imbalance and manifestations of the different GI symptoms such as abdominal pain, nausea, vomiting, and diarrhea, as described above. This change in the gut microbiota includes reduced levels of commensals microbes and is observed in patient samples even after 30 d of disease remission[38-40]. Additional studies addressed the imbalance of the gut microbiota and its association with different GI-related aspects of COVID-19[41]. The gut microbiota population in COVID-19 patients with low to moderate GI symptoms should also be analyzed. Evaluating these diverse patient populations will enable a thorough description of this phenomenon.

Table 1 Different gastrointestinal symptoms in coronavirus disease 2019 patients
FECAL VIRAL SHEDDING IN COVID-19 PATIENTS
Table 2 lists various cohort studies reporting fecal viral shedding by COVID-19 patients and detecting SARS-CoV-2 RNA in the fecal matter[42,43]. SARS-CoV-2 RNA-positive fecal matter was detected in 66.67% of COVID-19 patients (42 patients) in China[43]. Researchers attempted to evaluate the viral shedding period in stool samples, and noted viral shedding in asymptomatic patients. For example,SARS-CoV-2 RNA was detected from a stool sample of an asymptomatic child 17 d after viral exposure[9].
Certain studies have reported that virus separation from stool samples is difficult. For example,Wölfelet al[44] detected viral RNA in stool samples but attempts to isolate the virus were unsuccessful,most likely due to the mild nature of the infection. A viral load below 106copies per milliliter often hampers viral isolation[36]. The viral load also varies widely from one sample to another, including stool, serum, and respiratory samples[44-46]. However, understanding the correlation between the altered gut microbiota and the viral load in patient samples is essential for advancing therapeutic strategies centered around restoring the microbiota.
Additionally, efforts should focus on determining the possible correlation between fecal viral shedding and altered gut microbiota composition at different stages the infection,i.e., mild to moderateor severe COVID-19.
ALTERED GUT MICROBIOTA COMPOSITION IN COVID-19 PATIENTS
SARS-CoV-2 infections have led to changes in the ecology of the gut microbiota in patients (compared to that seen in controls). These changes are influenced by the immune responses elicited during COVID-19(Table 3). Different studies have revealed the growth of unusual microorganisms and depletion of common gut microbes (bacterial, viral, and fungal populations) in COVID-19 patients (Figure 3).
To understand the severity of disease in COVID-19 patients, the gut microbiota composition of 100 COVID-19 patients was analyzed in two hospital cohorts. Stool samples were collected from 27 of the 100 patients. The gut microbiome compositions were characterized using total DNA extracted from stool samples. The authors demonstrated that the number of gut commensals and Bifidobacteria was low and correlated with several factors of disease severity, such as high concentrations of inflammatory cytokines and C-reactive protein (CRP). These data suggests that the composition of the microbiota is associated with disease severity[38]. Another study carried out RNA and DNA profiling by sequencing of the virome using fecal matter from COVID-19 patients. The fecal matter of 98 COVID-19 patients was analyzed to understand COVID-19 severity and its association with the gut virome. The study showed that COVID-19 severity is inversely correlated with gut viruses, and older patients are more prone to severe COVID-19 outcomes[47]. Alterations in fungal microbiomes during COVID-19 have also been investigated. Analysis of the fecal mycobiome using the deep shotgun method showed heterogeneous microbial profiles, with enrichment of fungal genera such as Aspergillus and Candida. Two species ofAspergillus(Aspergillus flavusandAspergillus niger) were identified in fecal samples after clearance of SARS-CoV-2 from nasopharyngeal samples[48]. Additionally, there is evidence of abundant symbionts among COVID-19 patients includingClostridium ramosum, Coprobacillus,andClostridium hathewayi,which directly correlated with disease severity. Conversely,Faecalibacterium prausnitzii,which was also abundant among the patients, was inversely correlated with disease severity[49].

Table 3 Analysis of gut microbiota in coronavirus disease 2019 patients in different cohorts
Similarly, in a study by Yeohet al[38], stool samples from 27 patients were correlated with blood markers and inflammatory cytokines. The study concluded that the scale of COVID-19 severity might be associated with the gut microbiome and linked it to COVID-19 inflammation[46]. In another study containing a greater number of African Americans, enriched genera (Campylobacter, Corynebacterium,andPeptoniphilus)were mapped in the COVID-19 patient population, the gut microbial composition was markedly different between positive and negative samples. However, the study did not identify any considerable association between COVID-19 severity and microbiome composition[50].
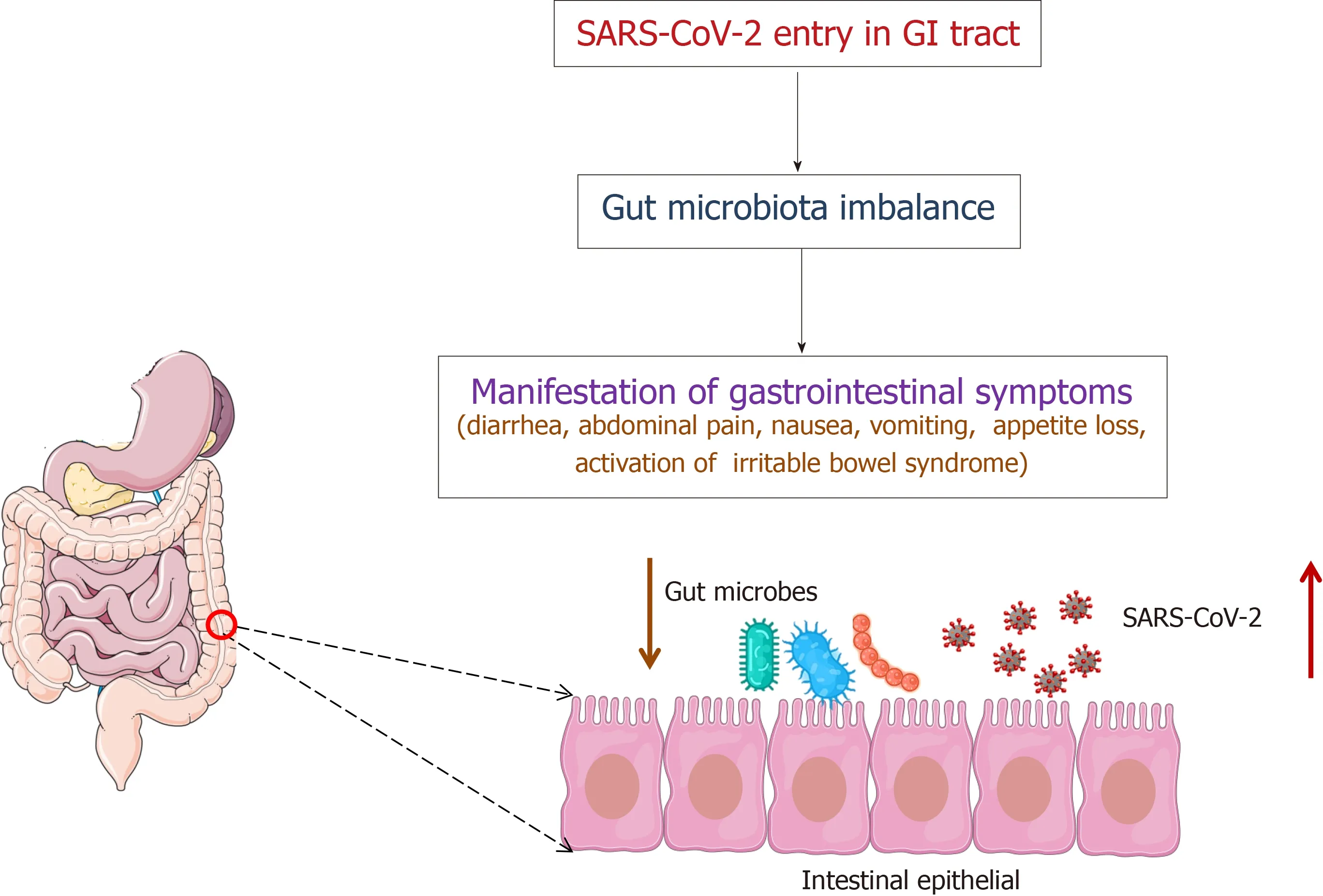
Figure 2 The schematic diagram illustrates the severe acute respiratory syndrome coronavirus 2 entry in the body, causes of gut microbiota imbalance which assists in manifesting the gastrointestinal symptoms in coronavirus disease 2019 patients. GI: Gastrointestinal;SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2.
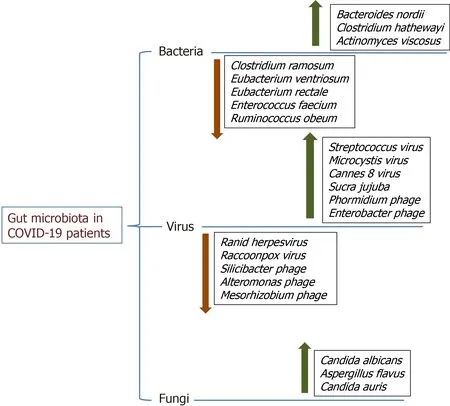
Figure 3 The diagram illustrates increased or decreased gut microbiota in coronavirus disease 2019 patients, including bacterial, viral,and fungal populations. COVID-19: Coronavirus disease 2019.
Certain studies even noted a reduction in fiber-utilizing bacteria such asPrevotella,Bacteroides plebius,andFaecalibacterium prausnitzii(F. prausnitzii), and a low Firmicute/Bacteroidetes ratio[51]. Poor outcomes were noted in special populations, such as hypertensive, diabetic, and elderly patients[52,53].Research is still underway to ascertain the different types of gut microbial populations (pro-inflammatory, opportunistic, beneficial, or anti-inflammatory) present depending on COVID-19 severity(Figure 4).

Figure 4 The diagram illustrates different types of mapped gut microbiota in coronavirus disease 2019 patients. Pro-inflammatory microbiota,opportunistic microbiota, the microbiome in severe coronavirus disease 2019 (COVID-19) patients, and the microbiome in low to moderate COVID-19 patients, antiinflammatory microbiota, and beneficial microbiota. COVID-19: Coronavirus disease 2019.
These studies help us understand how gut microbiota composition affects patients with moderate to severe COVID-19 and how gut microbiota diversity might alter immunity in COVID-19 patients.
ALTERATIONS IN THE BIOSYNTHESIS OF BIOLOGICAL COMPOUNDS IN THE GUT DURING COVID-19 INFECTION
Other than compositional changes in gut microbiota, functional changes during SARS-CoV-2 infection were observed in some patients. The gut microbiota aids in different biosynthetic pathways, such as amino acid biosynthesis, carbohydrate metabolism, nucleotide de novo biosynthesis, and glycolysis.This might be due to the abundance of bacterial components such asCollinsella tanakaei, Streptococcus infantis, Morganella morganii,andCollinsella aerofaciens,etc.Apart from these microbes, many short-chain fatty acid (SCFA) synthesis bacteria, such asLachnospiraceae bacteria,Bacteroides stercoris,Alistipes onderdonkii,andParabacteroides merdaewere present in COVID-19 samples with mild symptoms and in non-COVID-19 samples[54]. In a study using non-human primate models, β diversity analysis and 16S rRNA gene profiling were carried out to understand the gut microbiota composition during SARS-CoV-2 infection. The study revealed substantial changes in the gut microbiota composition and metabolism and a reduction in the concentration of SCFAs as well as a difference in the concentrations of bile acids.The study also found alterations in tryptophan metabolites during SARS-CoV-2 infection in the animal models[55].
Shotgun metagenomic sequencing using fecal samples has also been performed to profile the gut microbiome in SARS-CoV-2 infected patients. Researchers observed prolonged impairment of Lisoleucine biosynthesis and SCFAs due to alterations in the gut microbiome of patients with COVID-19[56].
ROLE OF ACE2 IN THE DIGESTIVE SYSTEM AND THE GUT MICROBIOME
The ACE2 (angiotensin-converting enzyme 2) receptor acts as a binding site by which SARS-CoV-2 enters host cells[57,58]. A higher expression of ACE2 in the cell favors SARS-CoV-2 infection. Despite this, ACE2 deficiency can play a vital role in SARS-CoV-2 infection[59]. Increased ACE2 expression is found in the epithelial cells of the respiratory tract (nasal mucosa, nasopharynx, and lungs), in different parts of the intestine, and in different types of epithelial cells, including nasal, corneal, and intestinal epithelial cells in humans[60]. In addition, this protein is expressed in different parts of the digestive system, such as the small intestine, stomach, colon, and liver[61]. However, ACE2 expression is controlled by distinct microbial communities in several body tissues. Mouse model studies suggest an association between certain microbial communities and overexpression of ACE2. This overexpression may prevent detrimental changes in hypoxia-induced gut pathophysiology and pulmonary pathophysiology[62]. ACE2 expression is controlled in the GI and respiratory tract[63]. Additionally, it can also be controlled by some bacterial species from important phyla. Downregulation of ACE2 expression was associated with the Bacteroidetes phylum. Among all species of this phylum,Bacteroides doreihas been shown to inhibit ACE2 expression in the colon, whereas the Firmicutes phylum plays a variable role in its modulation[20,49,64]. These findings are supported by other studies describing the modulation of ACE2 expression in the gut by the microbiota[65,66].
GUT-LUNG AXIS CROSSTALK DURING COVID-19 INFECTION
Several reports indicate that manipulation of the gut microbiota may be used to treat pulmonary diseases[67]. Therefore, the gut-lung axis crosstalk can help to elucidate these respiratory and digestive system interactions (Figure 5). Dysbiosis occurs when there are detrimental changes in the microbial composition of the gut or respiratory tract. It often leads to altered immune responses and the development of diseases, such as COVID-19. Nonetheless, of gut dysbiosis can be manipulated for treatment purposes[32,67-69]. Studies suggest that SARS-CoV-2 from the lungs travels to the gutviathe lymphatic system leading to disrupted gut permeability[70,71]. Furthermore, the extent of dysbiosis is associated with COVID-19 severity[4,72]. Therefore, understanding the crosstalk between the microbiome and the gut-lung axis during COVID-19 infection may provide therapeutic approaches.
GUT-BRAIN-LUNG AXIS CROSSTALK DURING COVID-19 INFECTION
Like the gut-lung axis, crosstalk between the microbiome and the gut-brain axis has been recognized and remains the topic[73-75]. Several studies have illustrated the role of the microbiome-gut-brain axis in different neurological disorders[76,77].
The interaction between the brain and the gut (also called the gut-brain axis) is bidirectional, with several pathways involved, including bacterial metabolites, neuroanatomical communications,neurotransmitters, and hormones[78]. The vagus nerve is primarily involved in such communication,and these molecules (neurotransmitters/hormones) are produced in the GI tract. During communication between neurotransmitters and hormones, they might interact with the receptors on the vagus nerve, relaying information to the brain[78-81]. Many hormones can cross the BBB and affect the CNS directly. Additionally, neuroendocrine pathways which operateviathe hypothalamic-pituitary-adrenal(HPA) axis associated with stress also affect the BBB. The stress-HPA axis is associated with the release of glucocorticoids such as cortisol from the adrenal cortex. Cortisol, is associated with augmented intestinal permeability and GI motility, affecting the gut microbiota[78,82-84]. The stress-HPA axis may also lead to inflammation and bacteria-derived impaired metabolite production, especially SCFAs[78,84]. Therefore, a thorough understanding of the gut-brain axis can help the development of therapeutic approachesviamodulation of the gut microbial composition.
The gut microbiota might play a distinct role in controlling the host immune system, and research is underway to uncover more in this field[85,86]. The involvement of the lungs (gut-brain-lung axis)occurs when inflammation and neurodegeneration in the brain stem due to COVID-19 prevent cranial nerve signaling, disrupting anti-inflammatory pathways and normal respiratory and GI functions.Recently, the lungs have been associated in the crosstalk among the microbiota-gut-brain axis components, and this axis was also noted during COVID-19 (Figure 6)[34,78]. Moreover, in COVID-19 patients, alterations in the gut microbiota have been shown to reduce live microbes (Bifidobacterium and Lactobacillus) during intestinal microbial dysbiosis[87].
The microbial translocation to the gut and its subsequent damage may play a vital role in inferior clinical outcomes for the disease. The gut-brain-lung axis during COVID-19 infection can also offer clues indicate viable directions for therapeutic development[34].
HYPOXIA IN COVID-19 AND GUT MICROBIOTA
Abnormal cytokine release (cytokine storms) and inflammatory responses may be associated with hypoxia during severe COVID-19. Viral replication in the lungs leads to a cytokine storm, destroying normal lung function and causing hypoxemia,i.e., low oxygen levels in the blood. Hypoxia-inducible factor-1α (HIF-1α) is a transcription factor that regulates cellular functions such as cell proliferation and angiogenesis. In hypoxic conditions, HIF-1α binds to the hypoxemic response element and induces the production of cytokines such as IL-6 and TNF-α, leading to hypoxia[88]. There are other collective causes of hypoxia, including pulmonary infiltration and thrombosis. The COVID-19 virus induces pneumonia that causes atelectasis (collapsing of air sacs), leading to low oxygen levels in the body[89].Additionally, COVID-19 leads to mitochondrial damage, production of reactive oxygen species, and subsequently HIF-1α, further promoting viral infections and inflammation[90].

Figure 5 The diagram points out the normal gut and its microbial association. The figure also illustrates the crosstalk between the microbiome and gut-lung axis. SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2.

Figure 6 The diagram describes the normal gut and its microbial association. The figure also illustrates the crosstalk between the microbiome and gut-brain-lung axis. BDNF: Brain-derived neurotrophic factor; HPA: Hypothalamic-pituitary-adrenal; SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2.
As part of its normal metabolic functions, the gut microbiota produces neurotropic metabolites,neurotransmitters, peptides, and SCFA, whose levels are disrupted due to COVID-19. SCFA such as butyrate confer neuroprotection. Modulation of gut microbes (responsible for such metabolite production) by SARS-CoV-2 alters hypoxia-sensing, negatively impacting the CNS[91]. Therefore, an association between gut microbiota and hypoxia in COVID-19 patients can be speculated, and may be linked to the CNS (Figure 7).
ALTERATION OF GUT MICROBIOTA IN COVID-19: EVIDENCE FOR INFLAMMATION OR DIEASE, SEVERITY?
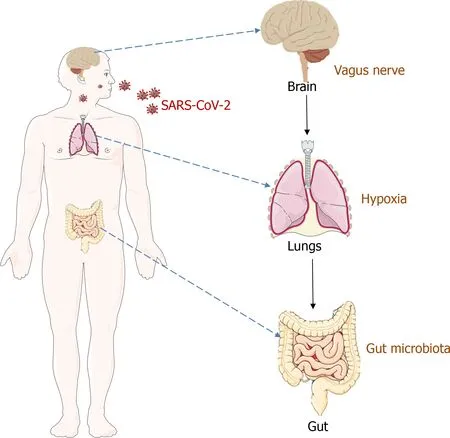
Figure 7 The figure illustrates an association between gut microbiota and hypoxia in coronavirus disease 2019 patients, and it is connected with central nervous system. SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2.
Under normal conditions, colonization of the normal microbiota in the gut causes resistance to pathogen[92,93]. Much of the normal gut microbiota belongs to Clostridia., which produces butyric acid. This SCFA is produced during dietary fiber fermentation along with acetic acid and propionic acid, which play a critical role in gut health (Figure 8A)[94,95]. Butyric acid helps in maintain the integrity of the gut barrier by providing a vital energy resource for colonocytes. This SCFA also hinders histone deacetylase activity and inhibits the activation of the nuclear factor (NF)-κB signaling pathway activation. This phenomenon may activate the G protein-coupled receptor pair (GPR41 /GPR43). These events help exert an anti-inflammatory response in normal gut health and stimulate regulatory T cells (Treg cells)[96-100]. Treg cells play a central role in suppressing inflammatory responses[97,101]. However, in COVID-19 patients, typical microbiota dysbiosis causes an imbalance in all these events.
There is a distinct connection between dysbiosis of the gut microbiota and hyper-inflammatory responses, especially cytokine release, in some COVID-19 patients[102] (Figure 8). Researchers noted that gut microbiota composition is related to the COVID-19 severity of and observed an association between altered cytokine levels and gut microbiota composition[38]. Cytokines/inflammatory factors,such as IL-1β, IL-6, and TNF-α, are usually associated with inflammation during disease[103]. In the case of severe COVID-19, the levels of certain cytokines, such as IL-6, IL-10, TNF-α, and IFN-are raised abnormally, and in some cases, cytokine storms are observed (Figure 8B)[23]. In pilot study, the quality of gut microbial composition was associated with the severity COVID-19 in 15 patients at the time of hospitalization in Hong Kong. The study showed an abundance of microbes such asClostridium hathewayi,Clostridium ramosum, andCoprobacillusin COVID-19 patients. Moreover, an anti-inflammatory bacteria,Faecalibacterium prausnitzii, was be inversely correlated with disease severity[49].
Nonetheless, more detailed studies are needed to understand the impaired gut health during COVID-19, especially in extreme forms of the disease. Another study confirmed microbiota dysbiosis in COVID-19 patients. This study found differential bacterial populations with a decrease inF. prausnitziiandClostridiumspp and an association of IL-21 in mild to severe COVID-19 patients[51].
A gut microbiota richness analysis in COVID-19 patients was conducted over through a six-month evaluation using 16S rDNA sequencing. This study showed that, patients with decreased postconvalescence richness in bacterial microbiota had high disease severity with increased CRP.Additionally, the authors observed increased incidence of intensive care unit admissions with worse pulmonary functions in these patients[104]. The study suggested an association between the hyperinflammatory response in COVID-19 and gut dysbiosis. However, a greater number of studies testing patients well after recovery are required to fully illustrate gut dysbiosis, associated factors, and the hyper-inflammatory response during COVID-19.
GUT MICROBIOTA IN ELDERLY OR CO-MORBID COVID-19 PATIENTS
Researchers have attempted to understand the role of the gut microbiota in elderly or co-morbid COVID-19 patients. A recent study evaluated the association of the gut microbiota and its modulation in COVID-19 patients. In this study, the cohort comprised approximately 200 severe COVID-19 patients hospitalized with pneumonia. Researchers considered elderly patients (age 62 years to 64 years) and their comorbidity. Patients in this study received two types of treatments: one group was treated with only the best available therapy (BAT), and the other group was treated with oral bacteriotherapy and BAT. Researchers found a decline in mortality and decreased progress in severe disease. Finally,researchers concluded that oral bacteriotherapy might be helpful in the management of hospitalized COVID-19 patients[105]. Similarly, Raoet al[106] noted that people with the comorbidities are more prone to COVID-19-related complications. In this case, immune system deregulation and deaths were also noted. However, researchers used-glucan to enhance the immune system in COVID-19 patients.This glucan was used to augment the activity of macrophages, natural killer cells, and IL-8, implicating that it might enhance the defense mechanisms to combat the virus[106].
Recently, Liuet al[1] evaluated the role of the gut microbiota composition and its association with the post-acute COVID-19 syndrome (PACS). In this study, researchers considered the comorbidities and dietary patterns during patient selection compare gut microbiota compositions. However, no considerable differences were observed in age, comorbidities, gender, antibiotics, or antiviral drug use between patients with PACS or without PACS[1].
Therefore, in cases of elderly or co-morbid COVID-19 patients, the gut microbiota might play an important role in immune system deregulation, although further studies are required to validate the findings.
GUT MICROBIOTA BASED ON ANTIBIOTIC USAGE IN COVID-19 PATIENTS
In COVID-19 patients, the use of antibiotics is relatively common. The frequently used antibiotics in COVID-19 patients are Azithromycin, Amoxicillin Clavulanate, Cephalosporin, Tetracycline[49,107],etc.The composition of the gut microbiota is hampered in COVID-19 patients due to the usage of antibiotics, occasionally causing antibiotic-associated diarrhea (AAD)[108]. Antibiotics usages in COVID-19 patients were increased the number of opportunistic pathogens compared with that detected in an untreated control group. Zuoet al[49] reported that the gut of COVID-19 patients, using antibiotics contains opportunistic bacterial pathogens such asBacteroides nordii,Actinomyces viscosus, andClostridium hathewayi. Additional studies also reported this phenomenon[22,109]. An increase of opportunistic bacterial pathogens causes dysbiosis of the gut. Rafiqul Islamet al[110] also noted that the abundance of opportunistic pathogens in COVID-19 patients in Bangladesh could cause dysbiosis, with 46 genera of opportunistic bacteria being identified patient GI samples. However, a study demonstrated that particular strains of probiotics may be useful for AAD[111]. Scientists have shown that the administration of oral probiotics can recover gut health and have antiviral effects[112,53]. For probiotic strain identification, Maket al[113] highlight the need for effective research to easily recognize the probiotic strains of therapeutic use. In this case, the probiotics should be specific for COVID-19, and help reduce the susceptibility to COVID-19 preventing severe COVID-19 disease.
GUT MICROBIOTA DYSBIOSIS DURING COVID-19 AND USE OF PROBIOTICS
Scientists identified an association between the gut microbiota dysbiosis and the severity of COVID-19.Magalhãeset al[52] noted that gut microbiota dysbiosis causes poor outcomes in elderly COVID-19 patients with hypertension and diabetes. Additionally, co-morbid elderly COVID-19 patients were prone to increased inflammatory situations due to the dysbiosis. The elevated amount of bacterial products in the gut might translocate into the blood due to the increased permeability across the intestinal epithelium. Bacterial toxin products, such as lipopolysaccharides (LPS), may accumulate in blood, aggravating TLR4 and subsequent downstream signaling. This could contribute to the “cytokine storm”, and result in complications in elderly COVID-19 patients[54]. Researchers also found a different route of activation of toll-like receptor (TLR4/TLR5) in COVID-19 patients[114-116]. Hunget al[53] also reported that gut microbiota dysbiosis increases COVID-19 severity in the elderly. However, the use of probiotics is a novel way to reduce COVID-19 severity in elderly populations.
THERAPEUTIC IMPLICATIONS AND CLINICAL TRIALS TO UNDERSTAND THE ROLE OF THE GUT MICROBIOTA DURING COVID-19
A careful analysis of the microbiome-gut-lung axis during COVID-19 infection can direct research towards therapeutic options for restoring gut health. As an altered gut microbiota is strongly associated with COVID-19 and its severity, supplementation of bacterial metabolites or commensals and prebiotics to enrich the microbial ecosystem is a path toward effective therapeutic options.
However, very few studies have explored this. A randomized clinical trial with 300 registered participants assessed the effectiveness of combination therapy usingLactobacillus plantarum(L. plantarum) CECT 7484,L. plantarumCECT 30292,Pediococcus acidilactici(P. acidilactici) CECT 7483, andL. plantarumCECT 7485, in adult COVID-19 patients (ClinicalTrials.gov; Clinical trial no. NCT04517422).Nonetheless, a deficiency of well-established data calls for more studies of this nature[41]. An openlabel, randomized clinical trial with 350 participants conducted by Kaleido Biosciences sought to determine the effectiveness of a novel glycan molecule (KB109) in patients with mild to moderate COVID-19 (ClinicalTrials.gov; Clinical trial no. NCT04414124)[117]. The synthetic glycan molecule reduced the number of acute care visits by COVID-19 patients. Additionally, disease resolution in patients with comorbidities was improved, compared to that in patients relying solely on supportive self-care.
A similar study attempted to evaluate the glycan molecule’s effectiveness (KB109) associated with gut microbiota function in COVID-19 patients. The same organization conducted the clinical study, an openlabel, randomized clinical trial in 49 participants in the United States (ClinicalTrials.gov; Clinical trial no. NCT04486482)[118]. There were no conclusive results; however, more studies are likely to be conducted in this sense. A complete list of the clinical trials initiated to understand the role of the gut microbiota in COVID-19 and its therapeutic implications are shown in Table 4.

Table 4 List of clinical trials initiated to understand the role of gut microbiota in coronavirus disease 2019 and its therapeutic implications
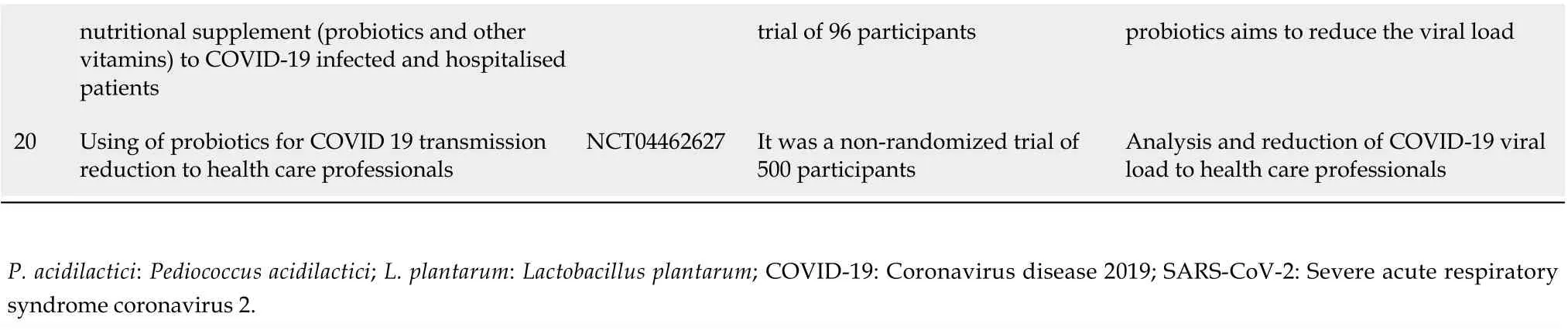
nutritional supplement (probiotics and other vitamins) to COVID-19 infected and hospitalised patients trial of 96 participants probiotics aims to reduce the viral load 20 Using of probiotics for COVID 19 transmission reduction to health care professionals NCT04462627 It was a non-randomized trial of 500 participants Analysis and reduction of COVID-19 viral load to health care professionals P. acidilactici: Pediococcus acidilactici; L. plantarum: Lactobacillus plantarum; COVID-19: Coronavirus disease 2019; SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2.
As the pandemic persists, it is critical to assess the effect of next-generation probiotics, prebiotics,synbiotics, and increased fiber intake on changes in gut microbiota composition in patients with mild to moderate and severe COVID-19.
FUTURE PERSPECTIVE
In several cases, complex pathophysiological and immunological responses are reported in the host due to SARS-CoV-2 infection. However, very little is known regarding the changes in gut virome in the COVID-19 patients, and this should be explored in future studies should explore it further. Moreover,the possible role of the gut microbiota in COVID-19 should be explored in future research. Likewise,population-based cohorts should be generated to illustrate the function of the altered gut microbiota during COVID-19 in different populations. This will enable the design of diagnostics and therapeutics for COVID-19 in different population types. Simultaneously, population-specific changes need to be described as this can help resolve severe conditions in COVID-19 patients. In the future, researchers should attempt to understand population-specific gut microbiota alteration during COVID-19 to design therapeutic interventions as required. Moreover, research could focus on the population specific changes in the immune response generated against the two altered gut microbiota during COVID-19.
CONCLUSION
Presently, abundant research has described the marked changes in the gut microbiomes of COVID-19 patients. Therefore, an apparent association exsists between the overall health of the gut microbiome and the progression of COVID-19[119]. Furthermore, the altered gut microbiota has been shown to persist in patients even after several days of recovery from COVID-19.
However, poor outcome were observed in elderly or co-morbid patients[97,120]. Recently, several studies discussed the factors associated with the modified gut microbiota in COVID-19 patients manifesting GI symptoms. According to some reports, increased inflammation may lead to a leaky gut,which enables the translocation of bacterial metabolites and toxins into the systemic circulation[97,120].This might cause further complications to the severe COVID-19 patients.
In this review, we have illustrated various GI aspects of COVID-19 patients including the gut microbiota imbalance and GI symptoms, the patterns of altered gut microbiota composition, the crosstalk between the microbiome and the gut-lung axis, the crosstalk between the microbiome and the gut-brain-lung axis, as well as hypoxia associated with altered gut microbiota. We also highlighted the association between the gut microbiota and elderly or co-morbid COVID-19 patients, as well as that of gut microbiota dysbiosis and COVID-19 severity. Additionally, we explored the correlation between,probiotics usage and the gut microbiota based on antibiotic usage in COVID-19 patients. Therefore, our review will provide a distinct outline for researchers working in the field. Also, it will provide valuable insight into the role of gut microbiomes in COVID-19 patients.
Currently, therapeutics are in development to combat COVID-19. In addition to antiviral therapeutics, probiotics might be effective for improving gut health through the gut-lung axis. Recently,several clinical trials have been initiated to understand the role of probiotics in COVID-19 patients. The ongoing clinical trials will elucidate the role of probiotic therapeutics or for COVID-19 patients, and offer new alternatives in COVID-19 treatment.
FOOTNOTES
Author contributions:Chakraborty C, Sharma AR, and Bhattacharya M contributed equally, Chakraborty C designed the research study and wrote the main manuscript draft; Sharma AR reviewed and edited the manuscript;Bhattacharya M developed the figures and tables; Dhama KD performed the English editing and validation; Lee SS did the funding acquisition; all authors have read and approved the final manuscript.
Supported bythe Hallym University Research Fund and the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2020R1C1C1008694 & NRF-2020R1I1A3074575).
Conflict-of-interest statement:There are no conflicts of interest to report.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:India
ORCID number:Chiranjib Chakraborty 0000-0002-3958-239X; Ashish Ranjan Sharma 0000-0003-3973-6755; Manojit Bhattacharya 0000-0001-9669-1835; Kuldeep Dhama 0000-0001-7469-4752.; Sang-Soo Lee 0000-0001-5074-7581.
S-Editor:Chen YL
L-Editor:A
P-Editor:Wu RR
 World Journal of Gastroenterology2022年25期
World Journal of Gastroenterology2022年25期
- World Journal of Gastroenterology的其它文章
- Correction to “Gut microbiota dysbiosis in Chinese children with type 1 diabetes mellitus: An observational study”
- Acupuncture and moxibustion for treatment of Crohn’s disease: A brief review
- Correlation of molecular alterations with pathological features in hepatocellular carcinoma: Literature review and experience of an Italian center
- Mapping the global research landscape on nutrition and the gut microbiota: Visualization and bibliometric analysis
- Upregulated adenosine 2A receptor accelerates post-infectious irritable bowel syndrome by promoting CD4+ T cells’ T helper 17 polarization
- Fecal gene detection based on next generation sequencing for colorectal cancer diagnosis
