Clinical observation on moxibustion at Baihui (GV20)plus Tuina for children with postnasal drip syndrome
YE Kang (叶康), DAI Qibin (戴奇斌)
Nanjing Integrated Traditional Chinese and Western Medicine Hospital Affiliated to Nanjing University of Chinese Medicine,Nanjing 210014, China
Abstract
Keywords: Moxibustion Therapy; Thermal Box Moxibustion; Tuina; Massage; Point, Baihui (GV20); Postnasal Drip Syndrome;Cough; Child, Preschool
Postnasal drip syndrome (PNDS) in children refers to that the mucosae of the posterior nose and throat are stimulated by the backflow of nasal secretions. The condition mainly presents with cough, and the associated symptoms include stuffy and runny nose as well as sneezing[1]. The duration of the cough is long and the efficacy of antitussive is not clear.
Western medicine mostly adopts symptomatic treatment to relieve the symptoms of this condition,such as glucocorticoid nasal spray[2], normal saline nasal irrigation, oral administration of leukotriene receptor modulator, and antihistamine[3]. Despite the relatively satisfactory efficacy they have achieved, the condition may relapse after stopping these medications.Moreover, long-term adoption is prone to various adverse reactions and can damage children’s immunity[4], which is unacceptable to their parents.
Traditional Chinese medicine (TCM) boasts many methods for this condition, such as nasal cavity irrigation with herbal medicine extract[5]and acupoint application[6]. In addition, pediatric Tuina (Chinese therapeutic massage) and moxibustion are easily accepted by children and their parents since they have no side effects.
In this study, we observed the clinical efficacy of moxibustion at Baihui (GV20) plus Tuina at the head and face for PNDS in children. The details are as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria for PNDS in children referred to theOtorhinolaryngology of Integrated Traditional Chinese and Western Medicine[7]and theChinese National Guideline on Diagnosis and Management of Cough(2015)[8]released by the Asthma Group of Chinese Thoracic Society.
Children with PNDS mostly experience persistent paroxysmal cough aggravated when they get up in the morning or change their body postures; backward flow of nasal secretions is noticed, and foreign body sensation may exist in the pharynx, and mucinous attachment and pebble-like view can be observed on the posterior pharyngeal wall; most patients have a history of chronic pharyngitis, rhinitis, sinusitis, nasal polyps, etc.
1.2 Inclusion criteria
Those who met the above diagnostic criteria; mainly presented with cough for more than four weeks,accompanied by symptoms including runny and stuffy nose as well as sneezing; with normal results of chest X-ray or CT examination; whose guardians voluntarily participated in the study and signed informed consent.
1.3 Exclusion criteria
Those who had foreign bodies or congenital dysplasia in the nasopharynx; those who had a history of drug allergy; those who were not able to take the medicine as required during the course.
1.4 Elimination and dropout criteria
Those who were unable to cooperate with the treatment during the course.
1.5 Statistical methods
The SPSS version 19.0 statistical software was adopted for data analysis. The counting data were expressed in cases and percentages, and Chi-square test was used. All measurement data conformed to normal distribution. They were expressed as mean ± standard deviation (±s) and analyzed witht-test.P<0.05 indicated a statistical significance.
1.6 General data
Patients from the Pediatric and Tuina Outpatients of Nanjing Integrated Traditional Chinese and Western Medicine Hospital Affiliated to Nanjing University of Chinese Medicine between January 2018 and December 2020 were recruited for the study. A total of 60 cases were divided into an observation group and a control group according to the random number table method, with 30 cases in each group. The minimum age of the observation group was 2 years and the maximum age was 6 years; the minimum age of the control group was 2 years and the maximum age was 6 years. There were no statistical differences between the two groups in the general data, including gender, age, and disease duration (P>0.05), indicating that the two groups were comparable (Table 1).
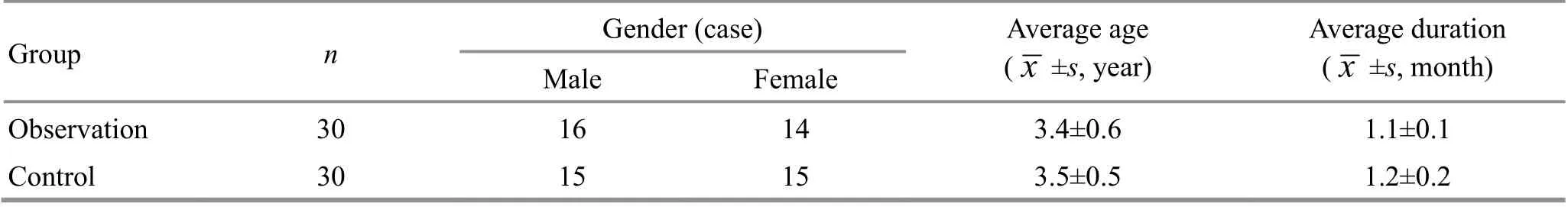
Group n Gender (case) Average age(Male Female images/BZ_7_1311_2835_1350_2881.png±s, year)Average duration(images/BZ_7_1311_2835_1350_2881.png±s, month)Observation 30 16 14 3.4±0.6 1.1±0.1 Control 30 15 15 3.5±0.5 1.2±0.2
2 Treatment Methods
2.1 Control group
Mometasone furoate nasal spray was adopted, once in the morning and once in the evening, with two sprays per nostril each time; 0.9% normal saline was used to wash both nostrils, once in the morning and once in the evening, for four consecutive weeks.
2.2 Observation group
In addition to the same hormone nasal spray and normal saline nasal irrigation as the control group,moxibustion at Baihui (GV20) and Tuina at the head and face were added for the observation group. Patients were firstly treated with moxibustion and then Tuina therapy.
2.2.1 Moxibustion therapy
Ignited a moxa stick of about 20 cm in length and 1.8 cm in diameter. Inserted the ignited end down into the moxibustion box till about 3 cm away from the protective net of the box. Then covered the box tightly.Asked the child to sit in a chair, with the upper body upright. Then aligned the moxibustion box right above Baihui (GV20) and attached the box to the head with a bandage to conduct moxibustion therapy (Figure 1).Asked the child to keep still, without shaking, lowering,or raising up the head. Parents cooperated with the treatment and held the moxibustion box. The medical staff was informed whenever the child was uncomfortable.
This treatment lasted 30 min each time, once a day,with 5-day treatments constituting one treatment course. The interval between two courses was 2 d. This treatment lasted for four courses.
2.2.2 Tuina therapy
Points: Baihui (GV20), Tianmen, Kangong, Shangen,Taiyang (EX-HN5), Yingxiang (LI20), Zhuntou; Fengchi(GB20), Fengfu (GV16), Jianjing (GB21), and Feishu(BL13)[9].
Baihui (GV20) is located at the intersection of the line between the two apexes of the ears and the sagittal line of the head. The operator An-Pressed and Rou-Kneaded it with his thumb 200 times (Figure 2a).
Tianmen is a vertical line from the middle of the two eyebrows to the anterior hairline. The operator used two thumbs to Tui-Push it from bottom to top alternately 50 times (Figure 2b).
Kangong is a horizontal line from the glabella to the tip of the eyebrow. The operator used two thumbs to Tui-Push from the glabella to the eyebrow tips on both sides 50 times (Figure 2c).
Shangen is located at the middle of two inner canthi and the depression on the bridge of the nose. The operator An-Pressed and Rou-Kneaded it 200 times(Figure 2d).
Taiyang (EX-HN5) is located in the depression on the outer side of the eyebrow. The operator An-Pressed and Rou-Kneaded it with his thumbs 200 times (Figure 2e).
Yingxiang (LI20) is located in the nasolabial fold and 0.5 Cun beside the wing of the nose. The operator An-Pressed and Rou-Kneaded it with his two thumbs 200 times (Figure 2f).
Zhuntou is located at the tip of the nose. The operator Rou-Kneaded it 200 times (Figure 2g).
Fengchi (GB20) is located in the depression between the sternocleidomastoid and the upper end of the trapezius, aligned with Fengfu (GV16). The operator An-Pressed and Rou-Kneaded it with his two thumbs 300 times (Figure 3a).
Fengfu (GV16) is located in the depression between the trapezius on both sides under the occipital tuberosity, 1 Cun above the middle of the posterior hairline. The operator An-Pressed and Rou-Kneaded it with his two thumbs 300 times (Figure 3b).
Jianjing (GB21) is located at the midpoint between Dazhui (GV14) and the acromion. The operator An-Pressed and Rou-Kneaded it with his two thumbs 300 times (Figure 3c).
Feishu (BL13) is located under the spinous process of the third thoracic vertebra, 1.5 Cun beside the Governor Vessel. The operator An-Pressed and Rou-Kneaded it with his two thumbs 300 times (Figure 3d).
The operator needs to pay more attention to An-Pressing and Rou-Kneading Yingxiang (LI20), Fengchi(GB20), and Fengfu (GV16). He should gradually exert force within the tolerance of the child and examine whether there are subcutaneous nodules on the head,face, and both wings of the nose or not, and whether there are cords in the neck or not. After confirming the existence of these pathogenic tissues, the operator should try to break the subcutaneous nodules and cords by Rou-Kneading and Bo-Plucking manipulations.
This treatment lasted about 20 min each time, once a day, with 5 d as a course. The interval between two courses was 2 d. This treatment lasted for four courses.
The clinical efficacy was evaluated after four weeks of consecutive treatments.

Figure 1. Moxibustion at Baihui (GV20)
3 Observation of Clinical Efficacy
3.1 Observation items
The TCM symptoms score was in accordance with the report of WANG C Y,et al[10]. Check Table 2 for details.
3.2 Efficacy evaluation criteria
The efficacy evaluation criteria were in accordance with theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[11]and theGuiding Principles for Clinical Study of New Chinese Medicines[12].
Cured: Symptoms like coughing, sneezing, runny nose,and nasal congestion all disappeared; the secretion almost disappeared or decreased significantly from the posterior pharyngeal wall.
Markedly effective: Symptoms like coughing,sneezing, runny nose, and nasal congestion were relieved; the secretion of the posterior pharyngeal wall decreased.
Invalid: Symptoms like coughing, sneezing, runny nose, and nasal congestion were not relieved or even worse; the secretion of the posterior pharyngeal wall did not decrease or even aggravated.
3.3 Results
3.3.1 Comparison of the clinical efficacy
After four weeks of treatment, the total effective rate of the observation group was 93.3% while that of the control group was 70.0%. There was statistical significance in comparing the total effective rate between the two groups (P<0.05), indicating that the clinical efficacy of the observation group is better than that of the control group (Table 3).
3.3.2 Comparison of the TCM symptoms score
Before treatment, there was no statistical significance in comparing the TCM symptoms score between the two groups (P>0.05). After four weeks of treatment,there was a significant intra-group difference in comparing the TCM symptoms score in both groups(P<0.01), suggesting that treatments for both groups are effective. After treatment, the TCM symptoms score of the observation group was lower than that of the control group (P<0.05), indicating that the symptoms in the observation group were relieved more significantly than those in the control group (Table 4).

Symptom None Mild Moderate Severe Coughing 0 2 4 6 Sneezing, runny, and stuffy nose 0 1 2 3 Secretion of the posterior pharyngeal wall 0 1 2 3
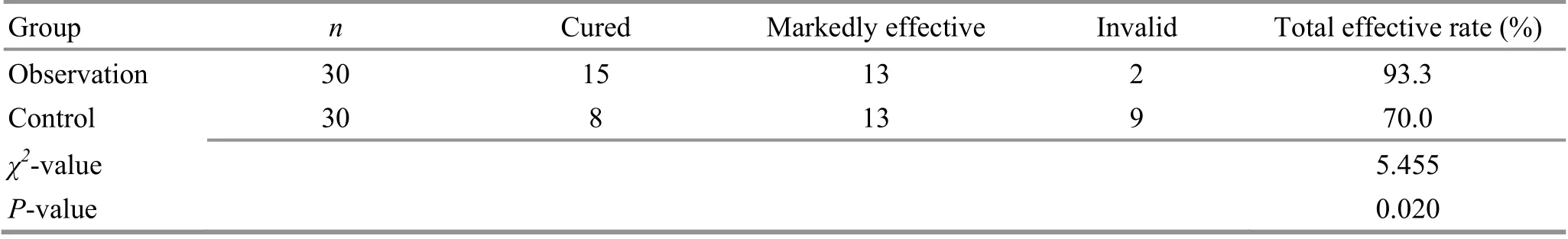
Group n Cured Markedly effective Invalid Total effective rate (%)Observation 30 15 13 2 93.3 Control 30 8 13 9 70.0 χ2-value 5.455 P-value 0.020
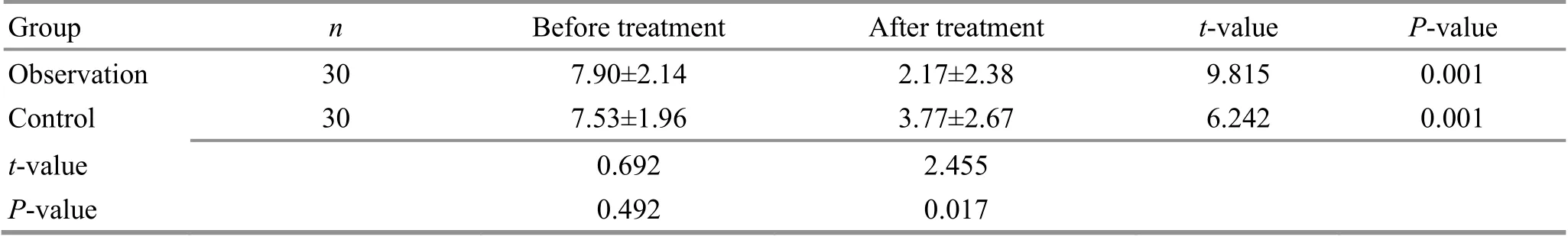
Group n Before treatment After treatment t-value P-value Observation 30 7.90±2.14 2.17±2.38 9.815 0.001 Control 30 7.53±1.96 3.77±2.67 6.242 0.001 t-value 0.692 2.455 P-value 0.492 0.017
4 Discussion
PNDS is one of the main causes of chronic coughing in children. The causative factors of this condition are complex. Most children suffering from this condition also experience allergic rhinitis, sinusitis, and pharyngitis. The nasopharynx of children with PNDS is stimulated by inflammatory secretions for a long time,which may lead to chronic coughing or secondary inflammatory reactions[13]. Chronic conditions may cause tissue infection of certain organs, and subsequently influence the growth of children[14].
PNDS in children is a disease that spans pediatrics and otorhinolaryngology with a high missed diagnosis rate[15]. Western medicine often adopts such methods as anti-infection drugs, nasal congestion improvement,drainage promotion, and inflammation relief. Since PNDS usually presents with no significant symptoms of infection, the efficacy of routine antibiotics and antitussives is not clear or even may damage tracheal and bronchial mucosa[16]. Moreover, long-term use of antibiotics may cause damage to the liver and kidney,metabolic disorders, and immune response inhibition,which may prolong the disease duration and affect the physical and mental health, as well as the growth of children[17].
Mometasone furoate is a glucocorticoid that can prevent local inflammation by spraying the nasal cavity.It is direct and effective, with fewer adverse reactions compared with systemic medication[18]. Washing the nasal cavity with 0.9% normal saline can remove pathogenic bacteria and harmful substances in it,correct the pH value, repair the nasal mucosa, restore the ciliary movement, improve its autoimmune function,and thus relieve the local symptoms.
PNDS in children falls under the categories of “Jiu Ke”(chronic coughing) and “Bi Yuan” (profuse nasal discharge) in TCM. In TCM theory, the lung opens into the nose, and the nose is located at the center of the face and is the confluence of clear Yang. Pathogenic factors can easily invade the lung through the nose[19].Deficiency of lung Qi and Wei-Defensive Qi may cause invasion of pathogenic factors, and the lung will fail in diffusing, subsequently leading to PNDS[20]. Therefore,the treatment principles are to diffuse lung Qi, and warm and tonify the lung, spleen, and kidney.
Baihui (GV20) is located at the top of the head and connects all the meridians. It has the functions of eliminating wind, dissipating cold, warming Yang,preventing collapse, and tranquilizing the mind.Moxibustion at Baihui (GV20) can stimulate meridian Qi,adjust the permeability of capillaries, and promote local blood circulation, thus warming meridians, dissipating cold, reinforcing Yang, preventing collapse, eliminating blood stasis, preserving health, and clearing heat.
By stimulating specific points or regions, pediatric Tuina can improve children’s immunity, stimulate Yang Qi, and subsequently unblock the meridians and regulate Zang-Fu organs. PNDS in children is often caused by the contraction of pathogenic wind and cold.The lung governs the skin and body hair and opens into the nose. Pathogenic cold invading the lung mainly manifests as nasal symptoms. In this regard, points around the nose and on the head and face were selected for the Tuina therapy. The stimulation of points around the nose and occipital bone via Tuina manipulations can promote local blood circulation and absorption of inflammatory exudate, and effectively relieve symptoms like coughing, sneezing, and stuffy and runny nose. Pediatric Tuina enjoys better acceptance by children compared with other therapies.
In this study, apart from routine mometasone furoate nasal spray and 0.9% saline nasal irrigation, patients received additional moxibustion at Baihui (GV20) and Tuina at the head and face, and the efficacy was clear.Without adverse reactions, this method is convenient and easy to accept, thus worthy of clinical promotion.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
There was no project fund support for this study.
Statement of Informed Consent
Informed consent was obtained from the guardians of the recruited children in this study.
Received: 5 March 2021/Accepted: 28 July 2021
 Journal of Acupuncture and Tuina Science2022年3期
Journal of Acupuncture and Tuina Science2022年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Meta-analysis of acupuncture intervening exercise-induced fatigue
- Clinical efficacy of electroacupuncture in controlling myopia in children and its influence on retinal blood flow
- Clinical study on warm needling moxibustion plus isokinetic muscle strength training in treating knee osteoarthritis
- Clinical efficacy of Tuina manipulations for lumbar disc herniation and its influence on posture-associated indicators
- Clinical study of warm needling moxibustion plus intra-articular injection of sodium hyaluronate for hip involvement in ankylosing spondylitis
- Clinical study of warm needling moxibustion combined with entecavir in the treatment of compensated cirrhosis due to chronic hepatitis B
