Double tracheal stents reduce side effects of progression of malignant tracheoesophageal fistula treated with immunotherapy:A case report
lNTRODUCTlON
Malignant tracheoesophageal fistula (MTEF) is a devastating complication of esophageal cancer and tracheocarcinoma, which leads to a shorter life-span and decreased quality of life. MTEF develops in approximately 5%-15% of patients with an esophageal malignancy, with less than 1% of those having bronchogenic carcinoma[1,2]. Airway stent insertion provides an effective approach to improve symptoms and quality of life[3]. Toripalimab, a selective monoclonal antibody to the immunecheckpoint protein programmed cell death protein-1 (PD-1), is used for patients with advanced or metastatic esophageal squamous cell carcinoma[4].
The day of gift-giving finally came. We oohed and aahed over our handiwork as the presents were exchanged. Through it all, she sat quietly watching. I had made a special pouch for her, red and green with white lace. I wanted very much to see her smile. She opened the package so slowly and carefully. I waited but she turned away. I had not penetrated9 the wall of isolation10 she had built around herself.
My son, go and lift your father s arm up on the bench, said the queen to one of the princes, for she easily knew the king again, although she was afraid to make herself known to him
In this report, we described the progression of MTEF in a patient caused by advanced esophagus squamous cell carcinoma invading the trachea, who was treated with toripalimab after tracheal stent placement.
CASE PRESENTATlON
Chief complaints
A 58-year-old male presented with an 18-d history of choking after drinking and eating. He was hospitalized in Dongzhimen Hospital in Beijing on April 28, 2020.
History of present illness
The patient had previously been diagnosed with advanced esophageal squamous cell carcinoma (c-T4bN0M1, stage 4B). The patient received radiation as the first-line therapy, without surgery or chemotherapy. He was then treated with afatinib for 4 d as a trial treatment. Subsequently, he began choking after drinking and eating, and developed dysphagia 18 d before admission. After anti-infective and nutritional support treatments, the patient's symptoms were not significantly relieved.
History of past illness
His daughter reflected for a moment, and then said: Dear father, I wish for eleven girls as nearly as possible of the same height, age, and appearance as myself
Personal and family history
The patient reported a personal history of smoking and drinking for more than 30 years. The patient reported his familial history did not include any tumors.
Physical examination
The patient’s physical examination was unremarkable.
Laboratory examinations
Tests of peripheral blood tumor markers showed that pro-gastrin-releasing peptide (commonly known as pro-GRP) was 93.58 pg/mL and carcinoembryonic antigen (commonly known as CEA) was 5.6 ng/mL, both of which were higher than the normal range. All other markers tested were within normal range. White blood cell count was 3.8 × 10/L, hemoglobin was 125 g/L, and C-reactive protein was 4.69 mg/L.
Imaging examinations
Insertion of a tracheal or esophageal stent, to cover the fistula, is also effective, as was the case with our patient. The stent placement relieved dyspnea for our patient, avoided chemical lung infections, and improved the quality of life, which enabled the patient to continue immunotherapy. Together, these factors likely contributed to the increased survival time for our patient, which was greater than the reported median survival time for MTEF (from stent insertion to death) of 163 d[3]. Although, it is important to note that the expanded stent may readily erode and enlarge the size of the fistula[5].
FlNAL DlAGNOSlS
Malignant tracheoesophageal fistula
Why didn t you call me up and tell me about your dream? he asked. They say that the more you talk about bad dreams, the sooner you ll stop having them.
The patient had no remarkable disease history.
TREATMENT
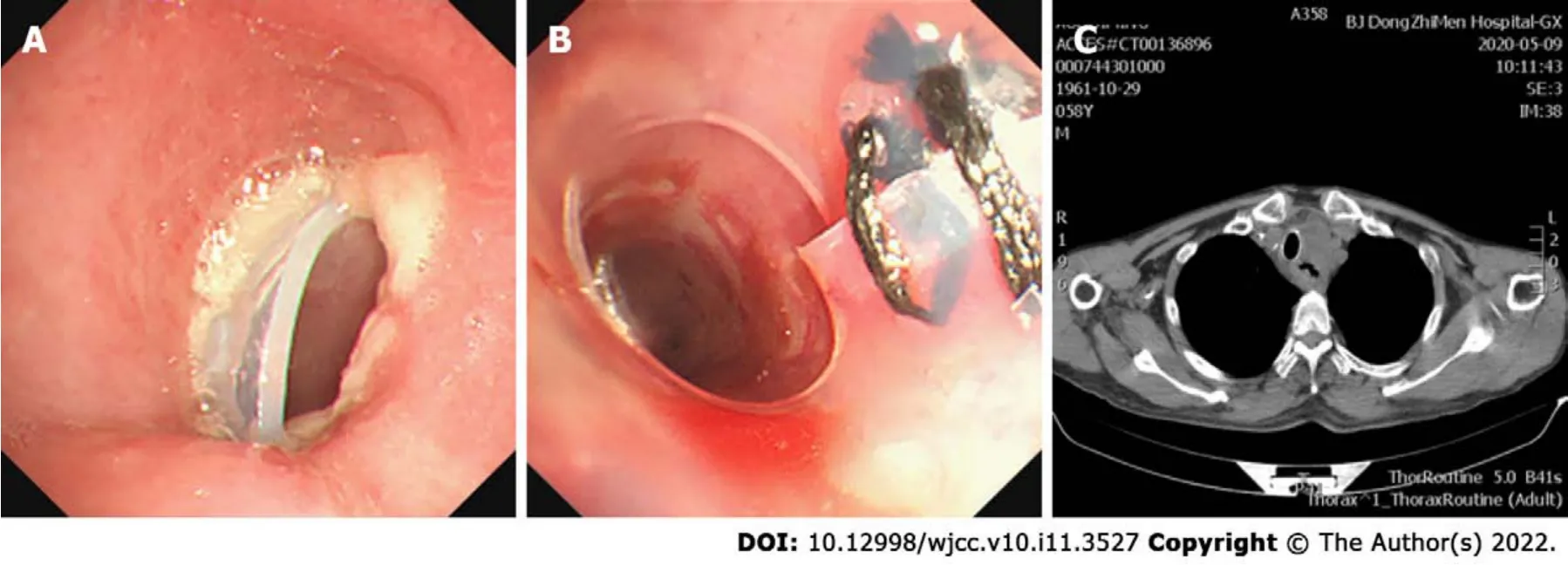
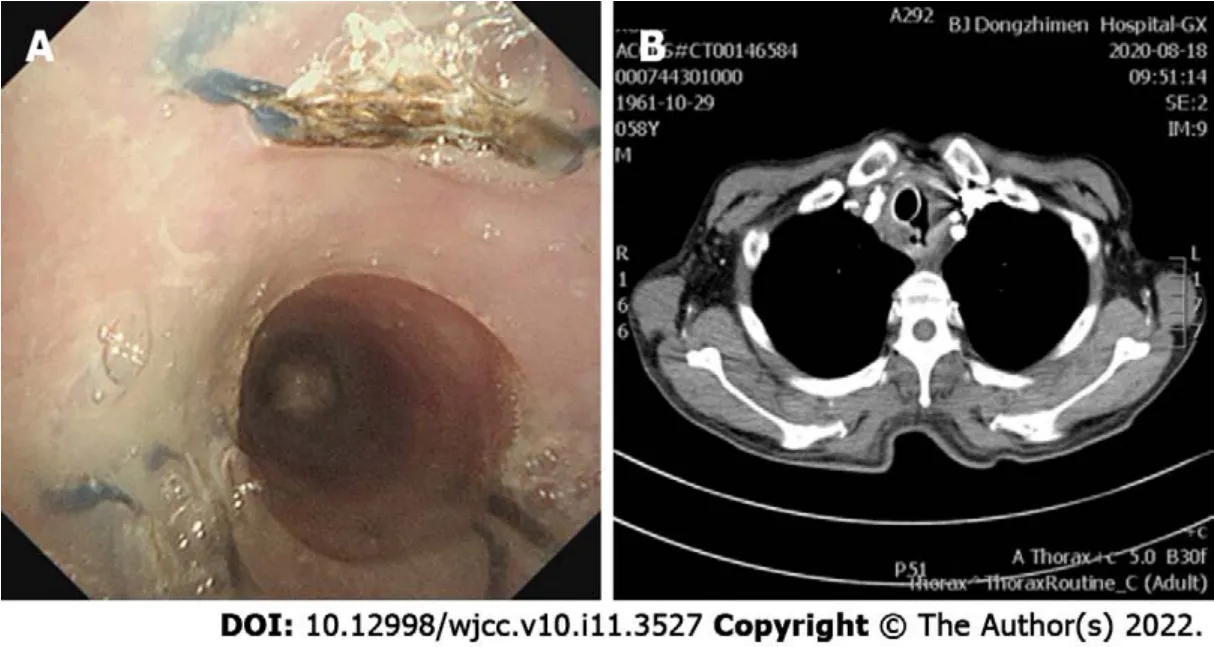
Given that the airway was significantly obstructed by the tumor, and performance status and Eastern Cooperative Oncology Group (commonly known as ECOG) classification had worsened from 1 to 3-4,mechanical debulking was performed on the tumor arising from the membranous trachea. Initially, a Yshaped silicone stent of 16 mm × 13 mm × 13 mm in diameter and 80 mm × 30 mm × 15 mm in length(TracheobronxaneDumonTD; Novatech SA, La Ciotat, France) was placed in the main trachea, with projections into both the left and right main bronchus by rigid bronchoscopy. However, the upper edge of the stent blocked the airway wall, so that the trachea was significantly narrowed. To open the trachea,a straight silicone stent 16 mm in diameter and 30-mm length, partially incised along the long axis, was sutured to reduce the lumen diameter and inserted into the Y-type Dumon stent in the form of a telescope (Figure 2). After placement of the stent, the fistula was completely enclosed, without significant stenosis of the trachea. One month after stenting, the patient received the first dose of toripalimab (240 mg, intravenous drip, every 3 wk). After the fourth dose of toripalimab, the patient presented with hemoptysis. Chest computed tomography and bronchoscopy revealed that the original malignant tracheoesophageal fistula between the upper trachea and esophagus had progressed rapidly in size, measuring 20-30 mm (Figure 3). However, the fistula was still completely covered by the silicone stents.
OUTCOME AND FOLLOW-UP
Despite the increased survival time, the patient in the present report experienced rapid progression of MTEF after tracheal stent placement and treatment with toripalimab. Although several clinical studies have reported promising efficacies and manageable safety profiles of immune checkpoint inhibitors(ICIs) on advanced or metastatic esophageal squamous cell carcinoma[8,9], response rates to different anti-PD-1 antibodies in patients with previously treated advanced or metastatic esophageal squamous cell carcinoma were reported to be 14.3%-33.3%[10,11]. However, there have been no reports of immunotherapy and/or stenting increasing the size of the original fistula. Based on our case report,however, there is a potential risk of treating MTEF with immunotherapy and stenting. It is possible that immunotherapy may have hastened the development of a fistula by lysing the tumor. Although the fistula progressed rapidly after immunotherapy, the enlarged fistula remained completely covered,owing to the appropriate size of the stents; in addition, due to the dilation of the trachea by the stents,the airway remained open and protected against lung infections from either the cancer or the esophagobronchial fistula.
DlSCUSSlON
MTEF develops in approximately 5%-15% of patients with an esophageal malignancy, with less than 1%of those having bronchogenic carcinoma[1,2]. MTEF is a negative predictor of long-term survival, and those patients generally have a very poor prognosis and quality of life. Severe cough, frequent aspiration pneumonia, malnutrition, and life-threatening hemoptysis can lead to rapid deterioration of the patient, and most patients die within 3-4 mo.
MTEF is mostly caused by tumoral invasion or as a complication of cancer therapies. Esophageal cancer invades the trachea directly through its membranous wall or indirectly through metastases from the mediastinal lymph nodes. This leads to tumor necrosis, thus paving the path for MTEF formation[5].
Immediate management of MTEF involves nasogastric tube placement or gastrostomy, to minimize regurgitation. However, this palliative treatment does not improve the patient's quality of life, due its preclusion of oral eating. Radical resection of the MTEF has been reported but with minimal survival advantage[6] because of the advanced stage of the cancer and the consequent and ongoing nutritional depletion. Mesenchymal stem cell transplantation therapy for MTEF is most useful for smaller bronchopleural and distal fistulas, but the further research is required to gain an accurate understanding of the treatment’s efficacy and safety profiles[7].
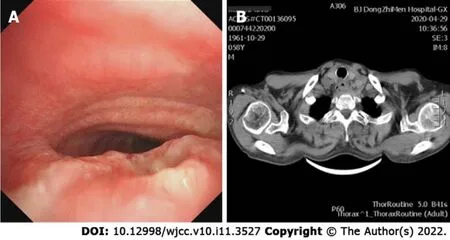
Bronchoscopy and computer tomography imaging found a 5 mm malignant tracheoesophageal fistula in the main airway, located between the upper trachea and esophagus (Figure 1).
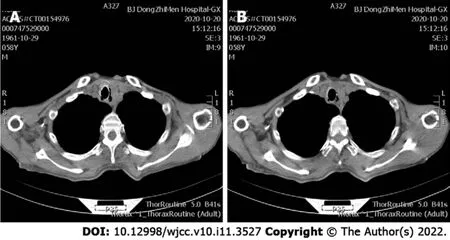
After palliative treatment for infection (piperacillin sodium and sulbactam sodium for injection, 3.75 g,intravenous drip, q8h) and hemostasis (haemocoagulase, 1 U, intravenous injection, q12h), the condition of the patient was stable. Immunotherapy was continued. During a 4-mo follow-up, no complications related to the stent placement were observed (Figure 4). However, after 7 mo total of toripalimab treatment, the patient died of esophageal cancer on February 16, 2021 (Figure 4B).
21.Offered meat and drink:If the king is fasting as a form of penance to take the offered food would be a break of that fast. Because he refused, he shows his piety like his wife does when she prays.Return to place in story.
However, Lin Guirui, a professor of psychology9 at Capital Normal University, encourages students to face up to their poverty. It s not a shame to be poor, Lin said.
CONCLUSlON
This rare case highlights the possibility that toripalimab might exacerbate the progress of a fistula in patients with MTEF. However, using an appropriately sized tracheal stent combined with ICIs therapy may improve the survival of patients with MTEF.
National Natural Science Foundation of China, No. 81973784.
Li CA, Ban CJ, and Wang HW designed the report; Yu WX, Wang LY, and Zou H collected the patient’s clinical data; Li CA and Ban CJ wrote the paper.
Helena sat down on the rocks which had been pointed9 out to her as the site of the castle, feeling very depressed10, but at the same time with the lurking11 hope that the kind Fairy would come once more to her aid
She cast one more lingering, half-fainting glance at the prince, and then threw herself from the ship into the sea, and thought her body was dissolving into foam
Written informed consent was obtained from the patient and his family for publication of this case report and any accompanying images.
The authors declare no conflicts of interest.
The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See:https://creativecommons.org/Licenses/by-nc/4.0/
China
Chang-An Li 0000-0001-9698-5585; Wei-Xia Yu 0000-0002-2749-6953; Lin-Yang Wang 0000-0003-2551-9506; Hang Zou 0000-0002-2570-7569; Cheng-Jun Ban 0000-0002-8468-3755; Hong-Wu Wang 0000-0003-1939-8795.
Ma YJ
A
Ma YJ
 World Journal of Clinical Cases2022年11期
World Journal of Clinical Cases2022年11期
- World Journal of Clinical Cases的其它文章
- Pleomorphic adenoma of the left lacrimal gland recurred and transformed into myoepithelial carcinoma after multiple operations:A case report
- Thyrotoxicosis after a massive levothyroxine ingestion:A case report
- Contrast-enhanced ultrasound manifestations of synchronous combined hepatocellular-cholangiocarcinoma and hepatocellular carcinoma:A case report
- Papillary thyroid microcarcinoma with contralateral lymphatic skip metastasis and breast cancer:A case report
- Del(5q) and inv(3) in myelodysplastic syndrome:A rare case report
- Ultrasound-guided local ethanol injection for fertility-preserving cervical pregnancy accompanied by fetal heartbeat:Two case reports
