Need for oxygen therapy and ventilatory support in premature infants in a hospital in Southern Brazil
Amanda Meier, Kelser de Souza Kock
Amanda Meier, Kelser de Souza Kock, Department of Physiotherapy, University of South of Santa Catarina, Tubarão 88704-001, SC, Brazil
Abstract BACKGROUND Prematurity in newborns is a condition that is associated with worse hospital outcomes when compared to birth to term. A preterm infant (PI) is classified when gestational age (GA) < 37 wk.AIM To analyze prognostic indicators related to the use of oxygen therapy, noninvasive ventilation (continuous positive airway pressure) and mechanical ventilation (MV) in PI.METHODS This is a retrospective cohort. The sample was composed of PIs from a private hospital in southern Brazil. We included neonates with GA < 37 wk of gestation in the period of January 1, 2018 to December 31, 2018. For data collection, electronic records were used in the Tasy PhilipsTM system, identifying the variables: maternal age, type of birth, prenatal information, GA, Apgar score, birth weight, neonatal morbidities, vital signs in the 1st hour at birth, need for oxygen therapy, continuous positive airway pressure and MV, hospitalization in the neonatal intensive care unit, length of stay and discharge or death.RESULTS In total, 90 PI records were analyzed. The median (p25-p75) of GA was 34.0 (31.9-35.4) wk, and there were 45 (50%) males. The most common morbidity among PIs was the acute respiratory discomfort syndrome, requiring hospitalization in the neonatal intensive care unit in 76 (84.4%) cases. The utilization rate of oxygen therapy, continuous positive airway pressure and MV was 12 (13.3%), 37 (41.1%) and 13 (14.4%), respectively. The median (p25-p75) length of stay was 12.0 (5.0-22.2) d, with 10 (11.1%) deaths. A statistical association was observed with the use of MV and GA < 28 wk, lower maternal age, low birth weight, Apgar < 8 and neonatal deaths.CONCLUSION The identification of factors related to the need for MV in prematurity may help in the indication of a qualified team and technologies to promptly meet the unforeseen events that may occur after birth.
Key Words: Premature; Continuous positive airway pressure; Artificial respiration; Non-invasive ventilation
INTRODUCTION
Prematurity in newborns is a condition that is associated with worse hospital outcomes when compared to birth to term. However, in recent years there has been an increase in survival rates due to the improvement in neonatal intensive care, supported by technological evolution and the qualification of professionals in the field[1]. Even with all these progressions, prematurity rates at the present time remain high, reaching 10.94% of live births in 2018 in Brazil[2].
The determining gestational age of a preterm birth (PTB) is less than 37 wk, related to some resultants that generate the anticipation of childbirth[3]. Obstetric complications can interfere with the natural process of pregnancy, causing premature delivery, some of which are infections, hypertensive diseases, diabetes and hemorrhages that are more common[4]. According to DATASUS in Brazil in 2018 (its last census), the duration of pregnancy between 22 wk and 36 wk was 322234 live births, among them single, double, and triple births; in the South region there were 43313 live births[2].
Among the factors related to the clinical evolution of the PTB are gestational age (GA), Apgar score, weight at birth, congenital malformations/morbidities and vital signs. The Apgar scale is a tool for systematic assessment of the newborn, created by Virginia Apgar in 1953, for this reason the name Apgar. It uses a numerical score from 0 to 10, which has five variables, heart rate, respiratory effort, color, muscle tone and reflex irritability. It is used as an indicator of fetal distress if less than 5 on the scale is determined. Oxygen therapy (O2) is offered to reduce respiratory difficulty and collaborate in hemodynamic stabilization[5]. Newborns under 2500 kg have an increased risk of death in the 1styear of life and of developing infectious diseases, respiratory diseases, growth retardation and development[6]. Constant monitoring and early initiation of appropriate therapy prevent possible complications of disease and prematurity[7].
In Brazil, 24061 live births and 268 neonatal deaths were named, with a neonatal mortality rate of 11.1 deaths per thousand live births. Causes of neonatal death prevailed in the prematurity group, accounting for about one-third of the cases, followed by congenital malformation (22.8%), infections (18.5%), maternal factors (10.4%) and asphyxia/hypoxia (7%)[8].
At-risk birth, as in PTB, a physiological and/or hemodynamic imbalance occurs, where the extrauterine environment generates numerous adaptations involving morphophysiological and biochemical maturation of the lung parenchyma[9]. The inability to achieve effective breathing, lack of a powerful respiratory drive, reduced muscle strength, lack of surfactant and high compliance of the chest wall are contributing factors to respiratory failure[10]. As a result of these factors, premature babies need respiratory assistance to perform and/or adapt gas exchange and establish consistent functional residual capacity[10].
Several methods are used to provide respiratory support to premature infants, including intubation, prophylactic surfactant, oxygen therapy and non-invasive ventilation. Intubation requires all airway control, reducing support according to tolerance, with as little intubation time as possible, avoiding related morbidities. Surfactant administration is prophylactic, preventing lung damage and respiratory implications[11].
Due to the importance in early recognition of PTBs that will need ventilatory support, this work sought to analyze prognostic indicators related to the need for invasive mechanical ventilation in PTB[8,12]. The use of maternal and newborn epidemiological parameters as well as physiological signs of the premature infant in the first 24 h can be used as indicators for respiratory failure. In this sense, the general objective of this study was to analyze factors related to the need for ventilatory support in PTB in 2018 in a hospital in southern Brazil.
MATERIALS AND METHODS
This is a retrospective cohort type study. The sample was composed of premature infants in a private hospital in the city of Tubarão, Santa Catarina, Brazil. It has 8 beds in the neonatal intensive care unit, 10 adult beds in the intensive care unit, 50 adult inpatient beds and 21 adult and pediatric beds as required.
The following criteria were adopted for inclusion: newborns of both sexes and preterm born with less than 37 wk of gestation in the period from January 1, 2018 to December 31, 2018. The exclusion criteria were incomplete medical records and newborns transferred to another hospital. Electronic records were used in the Tasy PhilipsTMsystem for data collection.
This research project was approved by the Ethics Committee in Human Beings of UNISUL under the number of the opinion 3.529.438, CAAE: 17573519.2.0000.5369.
The following variables were extracted from the electronic records: gestational age, Apgar score, birth weight, congenital malformations/morbidities, vital signs at the first hour of birth, maternal age, type of delivery, previous adequate prenatal, mother's morbidity, number of gestations, use of O2, non-invasive ventilation [continuous positive airway pressure (CPAP)] and mechanical ventilation (MV), need for admission to the neonatal intensive care unit, length of stay and discharge or death.
The data were stored in a database created with the Excel® software and later exported to the SPSS 20.0® software. They were presented through absolute numbers and percentages, measures of central tendency and dispersion. A logistic regression analysis was performed to obtain the odds ratio in comparison to the use of mechanical ventilation. Considering the 95% confidence interval, a 5% statistical significance level was used.
RESULTS
We analyzed 90 PTB records and their maternal antecedents. Of these, 81 were cesarean deliveries and 45 (50%) were boys. The median (p25-p75) age of the mother was 31.0 (28.0-35.0) years, the most common comorbidity was premature rupture of membranes, and other comorbidities included fetal malformations and inadequate fluid in the amniotic sac. The highest frequency of prenatal visits was 4 to 7, which 64 women performed.
The median gestational age was 34.0 (31.9-35.4) wk, where the most common morbidity among the PTB was respiratory distress syndrome. The Apgar in the first and fifth minute were higher than 8 in the majority, where 37 needed CPAP and 13 needed orotracheal intubation. The need of admission to the neonatal intensive care unit occurred for 76 patients, where the median length of hospital stay was 12.0 (5.0-22.2) d, of which 10 deaths occurred, totaling 11.1% of the PTB. Tables 1 and 2 summarize the information from maternal data and PTB.
In the present study, lower maternal age, lower gestational age, lower birth weight, Apgar < 8 and death were statistically significant and were associated with patients who required MV compared to those who did not require oxygen support (Table 3).
DISCUSSION
Prematurity all over the world is an evident problem in perinatal health, and in Brazil it is one of the major causes of infant mortality. Preterm infants (PIs) are at an increased risk of adapting to life in the extrauterine environment, mainly due to the immaturity of the physiological and anatomical system[9,13].
The main findings of the study showed that the need for MV is associated with extreme prematurity with gestational age < 32 wk, a lower maternal age, low birth weight, Apgar < 8 in the first and fifth minutes of life and neonatal deaths compared to PIs who did not use oxygen therapy. More than half of the studied PIs required some form of oxygen support, whether helmet or incubator O2, CPAP or MV.
Premature rupture of membranes is determined by the loss of amniotic fluid before birth. According to the Hackenhaaret al[14] study, that rupture may be associated with a pregnant woman’s age above 29 years. The study explained that it may be related to endogenous changes in the fetus and its annexes. In the present study we noticed that one-third of the pregnant women had premature rupture of membranes as a comorbidity and that a little more than half of the women were older than 30 years.
Prenatal care should be initiated in the first trimester of pregnancy; a total of at least six consultations should be performed. During the consultations, physical examinations should be performed, and if necessary, specific tests should be performed. The early initiation of prenatal care provides access to diagnostic and therapeutic methods to prevent possible pregnancy complications[14]. More than half of the pregnant women had 4 to 7 consultations, showing that consultations do not prevent prematurity but that a more thorough follow-up can prevent maternal and child complications.
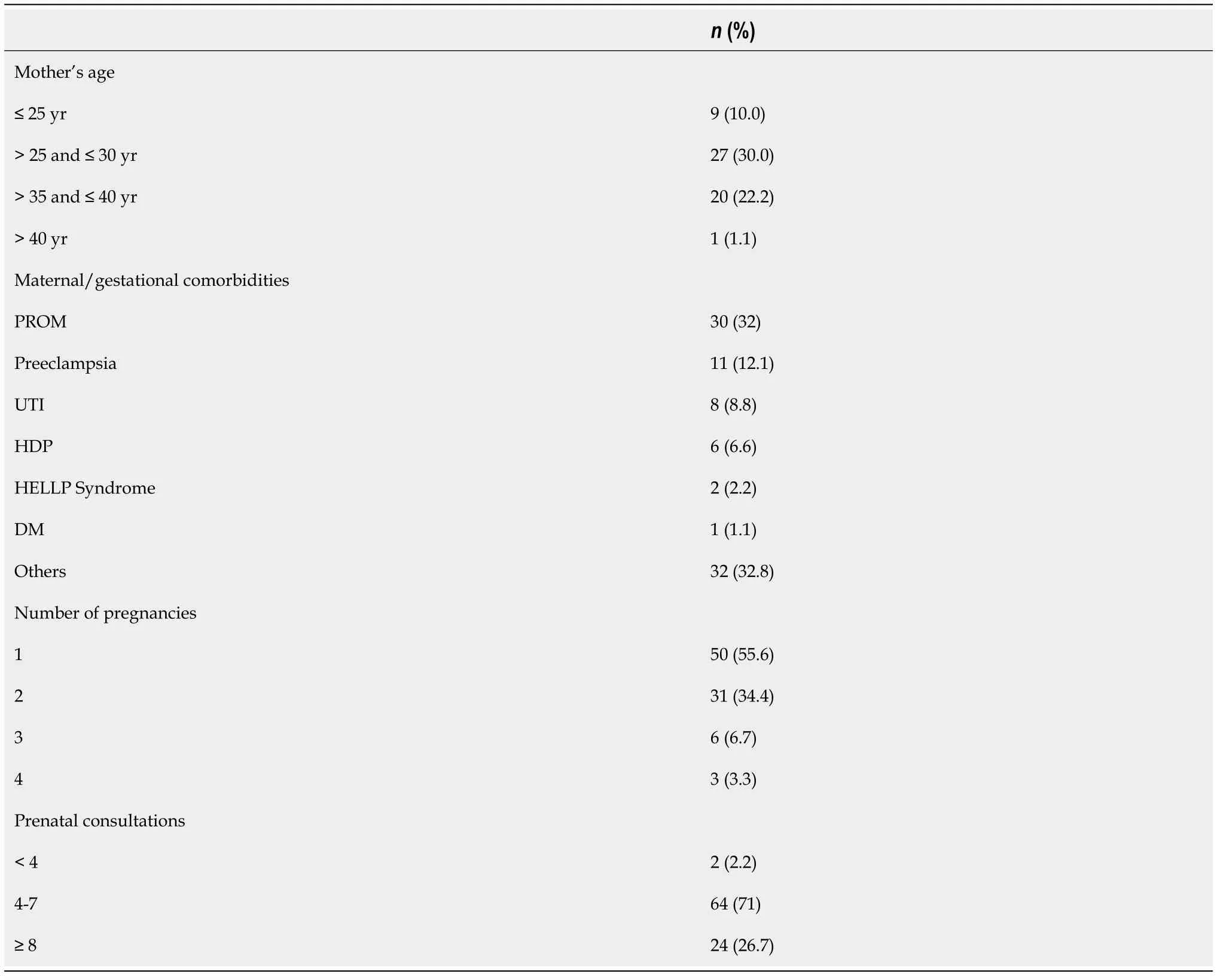
Table 1 Maternal data
Cesarean delivery was predominant in more than 85% of PIs, and most pregnancies were uniparous, according to the Miranda-Flores study[15]. Cesarean section is indicated in pregnancies from 26 wk to 31 wk + 6 d, and vaginal delivery in pregnancies under 26 and over 31, depending on maternal and fetal conditions, in which the cesarean section represents a higher percentage[15].
The median gestational age found was similar to the study by Galletaet al[16]. It is during this period that the formation of surfactant takes place by the type II pneumocytes, which are responsible for preventing the alveoli from collapsing when in contact with air. Newborn respiratory distress syndrome (NRDS) remains one of the most frequent complications in infants weighing 1500g or less.
The data in relation to neonatal death in this study are similar to the works of Lanskyet al[8] and Andegiorgishet al[17]. In the study by Myrhauget al[18], in infants born alive, the survival rate increased from 74.0% for infants born at 25 wk GA to 90.1% for those born at 27 wk GA. The study by Glasset al[19] reported the morbidity and mortality of 1765 PIs (birth weight 500-1500 g) in the period after implementation of neonatal intensive care units and mechanical respiratory support. In a metaanalysis evaluating the outcome in PIs, survival improved significantly with each week of GA and for each 100-g increase in birth weight. Specifically, survival in the 500-600 g group was only 20% compared to 56% in the 700-800 g birth weight group. It can be observed that in the studies there was a higher survival rate in infants with lower GA who had support in the neonatal intensive care unit where more and more medical and technological advances are showing a better prognosis regarding the prediction of ventilatory support[18]. In this study, it was observed that lower GA and low birth weight were associated with the use of MV, and this in turn was related to death.
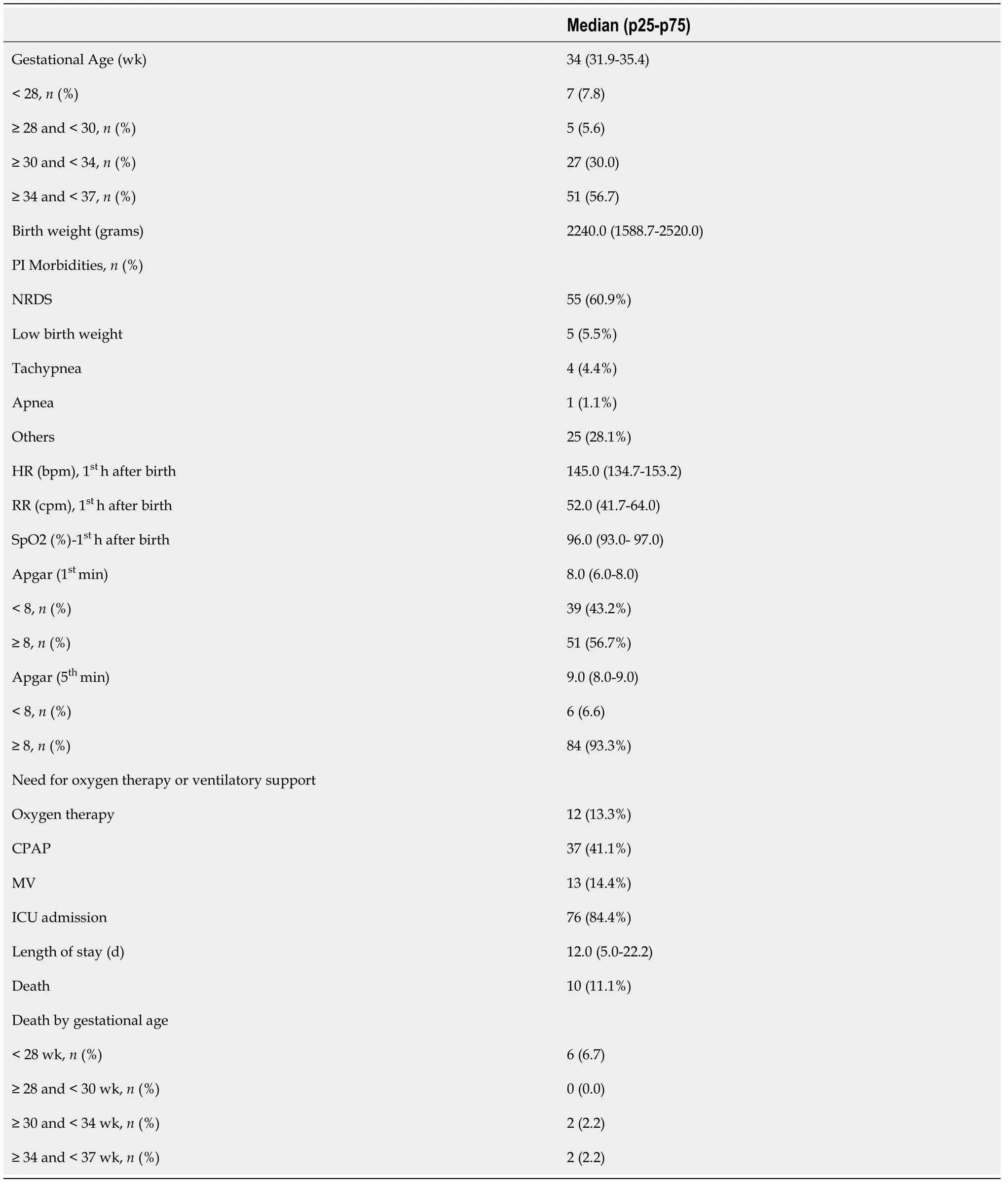
Table 2 Preterm infant data
The main morbidity found in PIs was NRDS. According to Sweetet al[20], NRDS is a significant problem for premature infants, and they sought to maximize survival with the creation of guidelines for better management of these patients. CPAP should be initiated from birth in all infants at risk of respiratory distress, such as those at < 30 wk GA who do not require intubation for stabilization. After stabilization, MV should be used in infants with respiratory distress when other methods of respiratory support fail. The duration of MV should be minimized whenever possible. To achieve the best outcomes for PIs with respiratory distress, optimal supportive care with monitoring of physiological variables is important. In the neonatal intensive care unit, there should be access to continuous pulse oximetry, electrocardiogram monitoring and monitoring of PaCO2 levels.
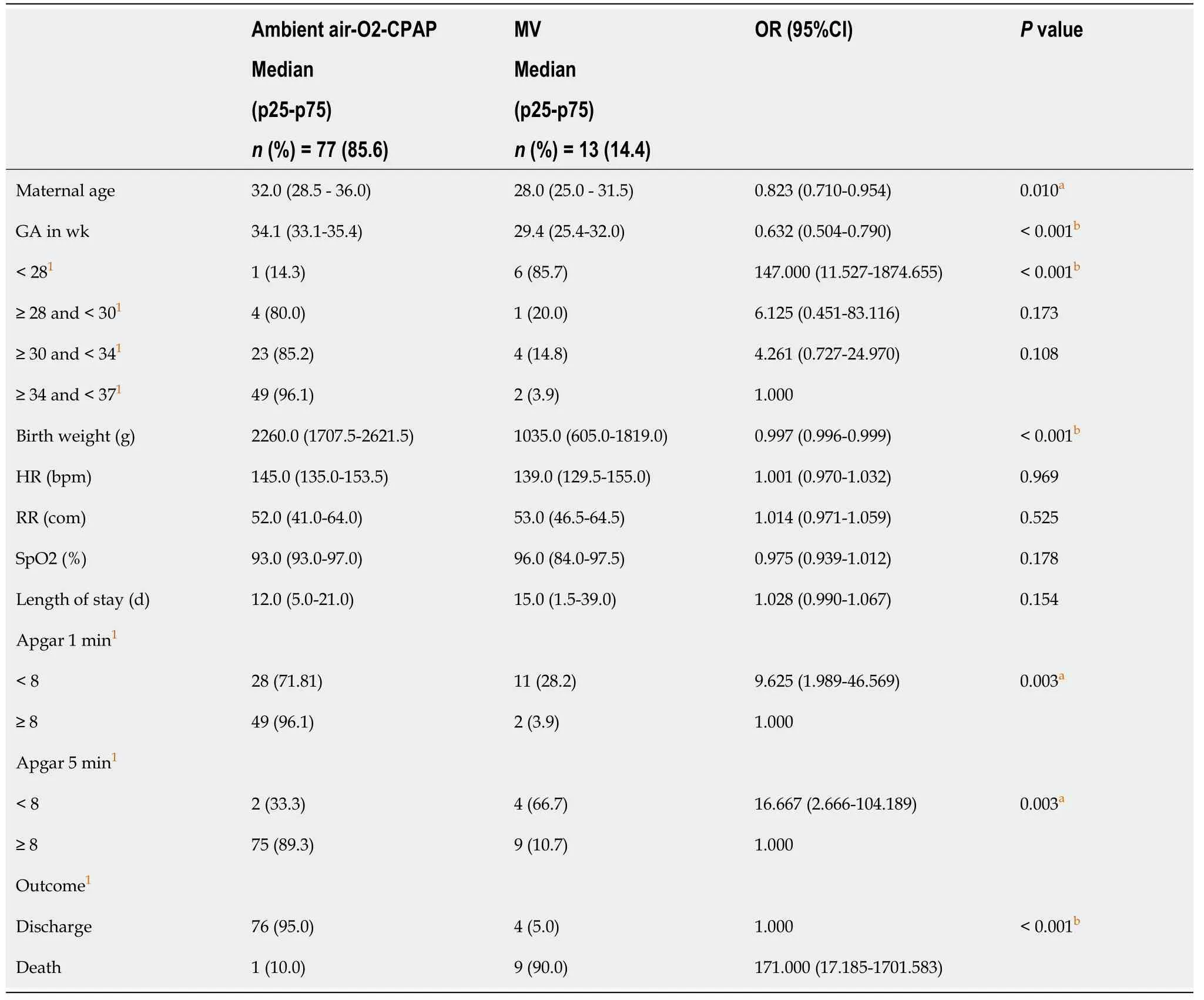
Table 3 Comparison of data according to the need for mechanical ventilation
Regarding vital signs in the first hour, no association was observed with the need for ventilatory support. According to the study by Kumaret al[21], where clinical assessment and nursing observation are very important, some vital sign data are not used and the update in the medical records can still be improved. Vital sign monitoring is constantly monitored on monitors at the incubator bedside. Short and long-term monitoring can predict sepsis risks and neurological and respiratory problems, as slowing heart rate may be indicative of some pathologies. Lower peripheral oxygen saturation (85%-89%) has a higher incidence of intermittent hypoxemia compared to higher peripheral oxygen saturation (91%-95%) during the first 3 d of life. Respiratory rate monitoring is important for detection of apnea associated with decreased heart rate and peripheral oxygen saturation. Perhaps, dynamic monitoring of vital signs could provide more prognostic information than those assessed only at the first hour.
The comparison of data from PIs with low Apgar scores at the fifth minute and birth weight less than 1500g are closely linked to the need for MV and neonatal mortality, corroborating the study by Daliliet al[22]. The study by Oliveiraet al[23] states that mortality increased for those with Apgar scores 4-7 in relation to PIs weighing between 1500 g and 2999 g, which shows that the lower the birth weight, the higher the mortality. The Apgar score was the best known and oldest form of measurement of neonatal asphyxia. New knowledge, such as the determination of fetal blood pH, among others, has changed this concept, and the score of 6 or less at the fifth minute has become the most important reference in the diagnosis and prognosis of asphyxia, along with the proposal not to wait for the first minute score to start resuscitation maneuvers. Despite this, the first minute score still seems to have importance in the prognosis of mortality[21,22].
Limitations found in this study were the small sample size, research conducted in a hospital that provides health care only to health insurance companies/private entities, and not being able to generalize the findings to other hospitals.
CONCLUSION
We conclude that the need for mechanical ventilation is associated with extreme prematurity with GA < 28 wk, lower maternal age, low birth weight, Apgar < 8 at the first and fifth minutes of life and neonatal deaths. NRDS is the most frequent morbidity in premature infants, where more than half of those studied required some form of oxygen support, whether O2, CPAP or MV. The identification of factors related to the need for MV in prematurity may help in the indication of a qualified team and technologies to promptly meet the unforeseen events that may occur after birth.
ARTICLE HIGHLIGHTS
Research background
Prematurity may be associated with some degree of respiratory failure.
Research motivation
Clinical recognition of premature infants at risk is important for appropriate management of ventilatory support.
Research objectives
To assess maternal and newborn factors related to the need for ventilatory support.
Research methods
A retrospective cohort conducted in a private hospital in southern Brazil consisted of preterm infants with gestational age < 37 wk.
Research results
We evaluated 90 premature infants with median (p25-p75) gestational age of 34.0 (31.9-35.4) wk. The utilization rate of oxygen therapy, continuous positive airway pressure and mechanical ventilation was 12 (13.3%), 37 (41.1%) and 13 (14.4%), respectively. The median (p25-p75) length of stay was 12.0 (5.0-22.2) d, with 10 (11.1%) deaths. A statistical association was observed with the use of mechanical ventilation and gestational age < 28 wk, lower maternal age, low birth weight, Apgar < 8 and neonatal deaths.
Research conclusions
The need for mechanical ventilation in premature infants was related to low birth weight, extreme prematurity and low Apgar.
Research perspectives
Other clinical indicators for predicting ventilatory support in premature infants can be used, such as monitoring vital signs and their variability measures.
FOOTNOTES
Author contributions:Meier A performed the data collection and wrote the manuscript; Kock KS performed the statistical analysis and revision and editing of the manuscript.
Institutional review board statement:This research project was approved by the Ethics Committee in Human Beings of (University of Southern Santa Catarina, Brazil) UNISUL under the number of the opinion 3.529.438, CAAE: 17573519.2.0000.5369.
Informed consent statement:All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement:The informed consent form was waived because only information from the electronic records was collected and the patients were not hospitalized during the study period.
Data sharing statement:No additional data are available.
STROBE statement:The authors have read the STROBE Statement-checklist of items, and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Brazil
ORCID number:Amanda Meier 0000-0002-9856-5215; Kelser de Souza Kock 0000-0002-0117-6142.
S-Editor:Wang LL
L-Editor:Filipodia
P-Editor:Wang LL
 World Journal of Critical Care Medicine2022年3期
World Journal of Critical Care Medicine2022年3期
- World Journal of Critical Care Medicine的其它文章
- Cough as a neurological sign: What a clinician should know
- Presentation and outcome of myocardial infarction with nonobstructive coronary arteries in coronavirus disease 2019
- Plasma D-dimer level in early and late-onset neonatal sepsis
- Stress cardiomyopathy in critical care: A case series of 109 patients
- Critical care practices in the world: Results of the global intensive care unit need assessment survey 2020
- Diuretic combinations in critically ill patients with respiratory failure:A systematic review and meta-analysis
