Point-of-care ultrasound for critically-ill patients: A mini-review of key diagnostic features and protocols
Yie Hui Lau,Kay Choong See
Yie Hui Lau,Department of Anaesthesiology,Intensive Care and Pain Medicine,Tan Tock Seng Hospital,Singapore 308433,Singapore
Kay Choong See,Division of Respiratory &Critical Care Medicine,National University Hospital,Singapore 119074,Singapore
Abstract Point-of-care ultrasonography(POCUS)for managing critically ill patients is increasingly performed by intensivists or emergency physicians.Results of needs surveys among intensivists reveal emphasis on basic cardiac,lung and abdominal ultrasound,which are the commonest POCUS modalities in the intensive care unit.We therefore aim to describe the key diagnostic features of basic cardiac,lung and abdominal ultrasound as practised by intensivists or emergency physicians in terms of accuracy(sensitivity,specificity),clinical utility and limitations.We also aim to explore POCUS protocols that integrate basic cardiac,lung and abdominal ultrasound,and highlight areas for future research.
Key Words: Critical care;Echocardiography;Point-of-care testing;Sensitivity and specificity;Ultrasonography
lNTRODUCTlON
Diagnostic errors in medicine and intensive care are prevalent,with autopsy studies showing substantial misdiagnoses[1].Point-of-care ultrasonography(POCUS)fills a void to reduce diagnostic uncertainty and some features may also guide prognosis and management.However,image acquisition and interpretation needs to be done with skill and caution to avoid inadvertent over-or underdiagnosis of abnormalities.POCUS misdiagnoses due to inexperience may lead to errors in the treatment that may worsen patients’ outcomes or even be fatal[2].Each POCUS practitioner must be mindful of this,and follow up or evaluate with alternatives where applicable.It is still important that any form of POCUS should be preceded by clinical examination,which provides complementary information for diagnosis and treatment.
There is an increase in the application of POCUS for managing critically ill patients,performed by intensivists or emergency physicians,who are neither radiologists nor sonographers.POCUS is inexpensive,non-invasive and can be readily available at the bedside.It is thus an important skill-set for anyone who takes care of critically ill patients.
POCUS may be too brief to have in depth interrogation of any pathology found and more detailed scanning is not practical in a busy intensive care unit(ICU)or emergency department.Excessive time taken for image acquisition and measurements may delay other clinical assessment or treatment.If abnormalities are found or if a comprehensive evaluation is required,a formal transthoracic echocardiogram or follow up computed tomography(CT)imaging can then be arranged at a more opportune time.
Results of needs surveys among intensivists reveal emphasis on basic cardiac,lung and abdominal ultrasound[3],which are the commonest POCUS modalities in the ICU.We thus aim to describe the key diagnostic features of basic cardiac,lung and abdominal ultrasound as practised by intensivists or emergency physicians in terms of accuracy(sensitivity,specificity),clinical utility and limitations.We also aim to explore POCUS-based protocols that integrate these ultrasound features.
BASlC CRlTlCAL CARE ECHOCARDlOGRAPHY
Basic critical care echocardiography(CCE)typically involves obtaining 4 echocardiography views(parasternal long axis,parasternal short axis,apical four-chamber,subcostal views)to answer urgent questions at the bedside,regarding myocardial contractility,left ventricular filling,right ventricular dilatation,or the presence of other obvious abnormalities(e.g.large pericardial effusion).Myocardial contractility is usually described in terms of regional wall motion abnormalities such as hypokinesia,dyskinesia or akinesia.Image acquisition and interpretation requiring all 4 of these views require skill and competency in order to complete the assessment in a timely manner.CCE is most often used to evaluate causes of shock,cardiac arrest or acute cardiopulmonary failure.Some key features of basic CCE are summarised in Table 1;examples in Figure 1.
BASlC LUNG ULTRASOUND
Lung ultrasound has also gained popularity because of its relative portability.The added benefit compared to chest radiographs and CT imaging,is that the patient’s clinical course can be conveniently followed up over time with no radiation risk.Lung ultrasound has been shown to reduce the use of chest radiographs and CT scans in critically ill patients by 26% and 47% respectively[4].The diagnostic accuracy rates of lung ultrasound for cardiogenic pulmonary edema(94%vs65%,P= 0.03)and for pneumonia(83%vs66%P= 0.016)are better if paired with CCE,than compared to lung ultrasound alone[5].Some of the key features and the clinical utility of these features are described in Table 2,with examples in Figure 2.
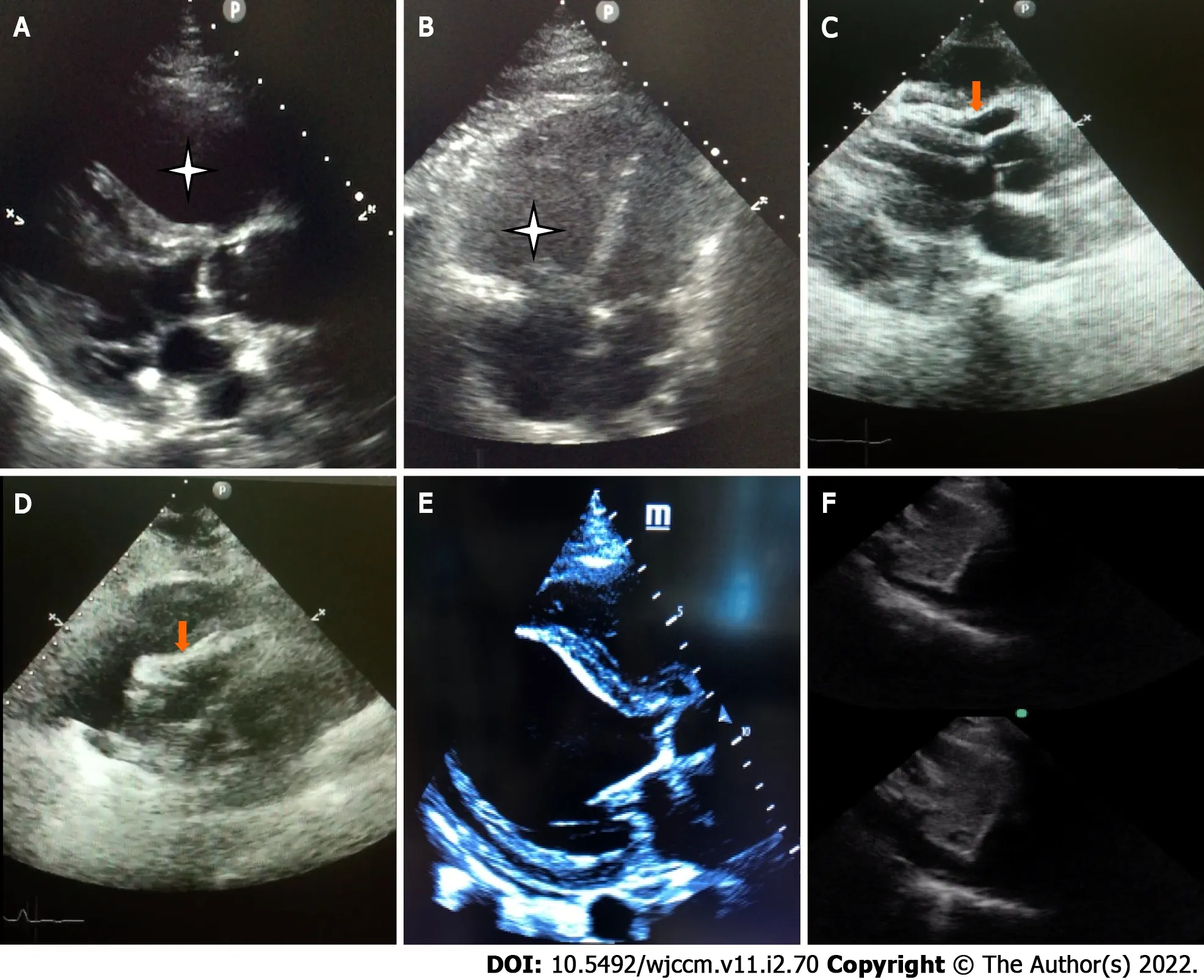
Figure 1 Key features in basic critical care echocardiography.A: Dilated right ventricle[Parasternal long axis(PLAX)];B: Dilated right ventricle(Apical 4 chamber view);C: Pericardial tamponade-Pericardial effusion with diastolic collapse of right ventricle(PLAX view);D: Pericardial tamponade-Pericardial effusion with systolic collapse of right atrium[subcostal long axis(SLAX)view];E: Left ventricular dysfunction-minimal thickening and contraction of basal anteroseptal and inferolateral wall with severe hypokinesia(PLAX view);F: Inferior vena cava variation of > 50% with foreceful spontaneous respiration-“sniff test”(SLAX view).
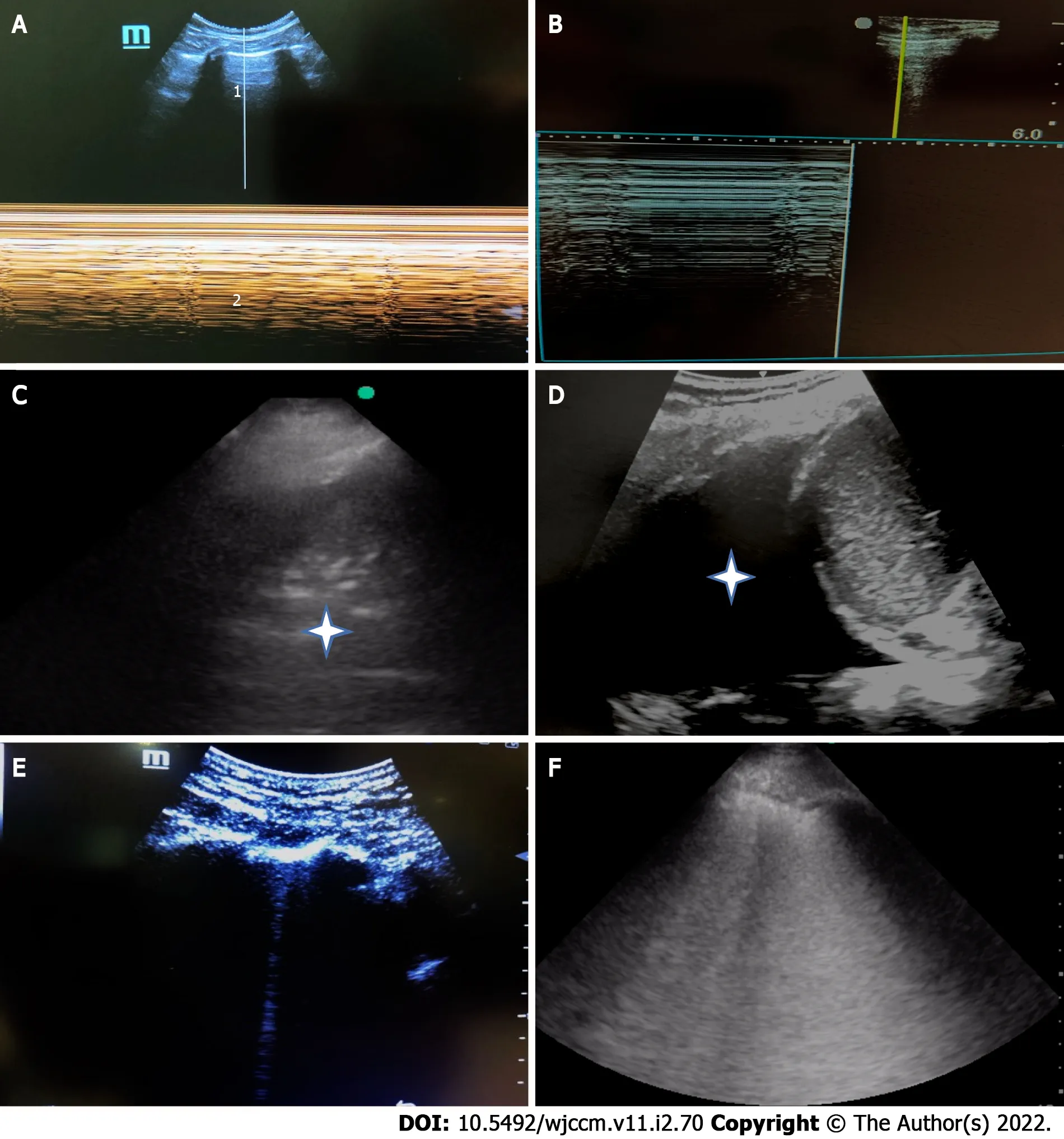
Figure 2 Key features in basic lung ultrasound.A: M-mode lung ultrasound-normal a lines(1),and seashore sign(2);B: M-mode lung ultrasoundpneumothorax Bar code/stratosphere sign;C: Consolidation with air bronchograms(Asterisk);D: Pleural effusion(large);E: 1 single B line-normal;F: B profile,> 3 B lines(confluent)-pathological.
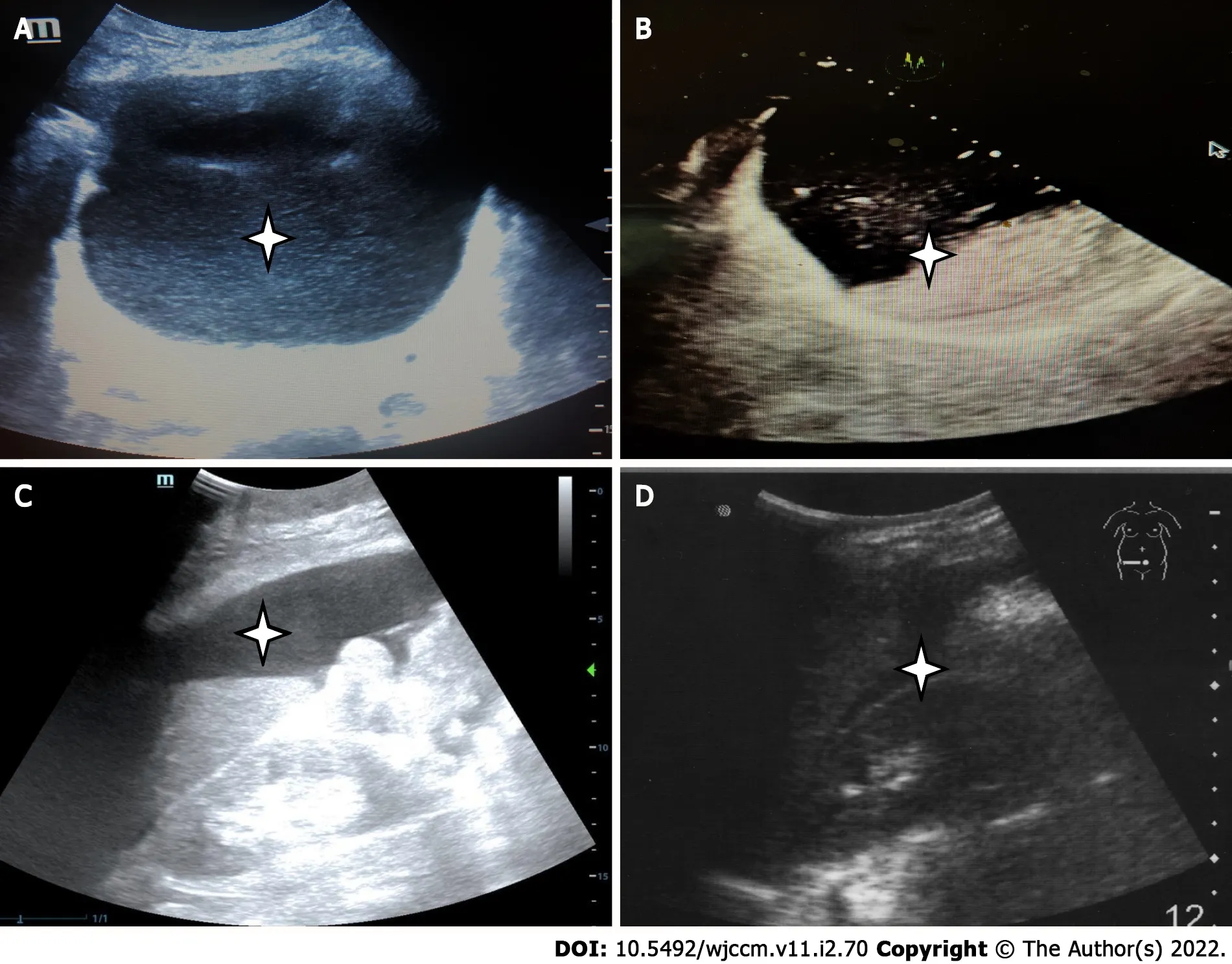
Figure 3 Key features in abdominal ultrasound.A: Bladder overdistension due to acute retention of urine(Asterisk);B: Incomplete gastric emptying(presence of semi-digested food in the stomach,Asterisk),which will indicate need for rapid sequence induction for intubation;C: Ascites(Asterisk);D: Free fluid in the hepato-renal pouch.In cases with abdominal trauma,this indicates intra-peritoneal bleeding(Asterisk).
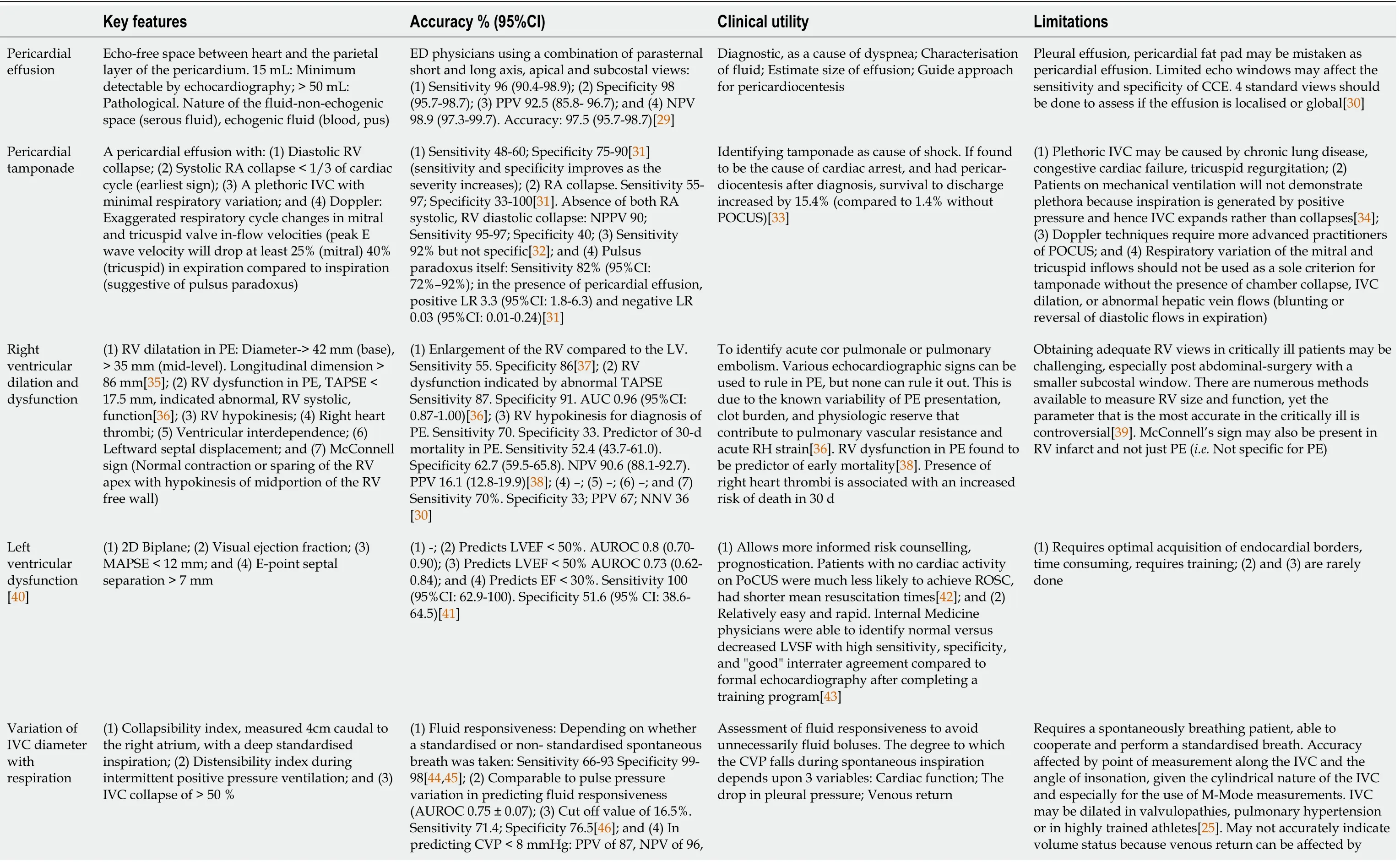
Table 1 Characteristics of basic critical care echocardiography
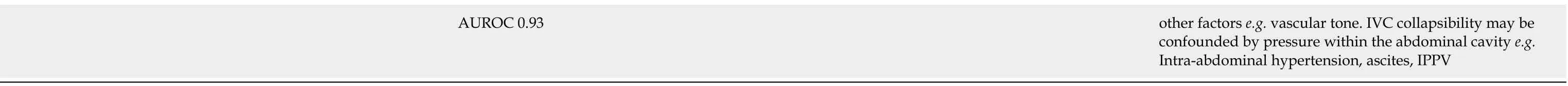
AUROC: Area under receiver operating characteristic;CVP: Central venous pressure;ED: Emergency department;IPPV: Intermittent positive pressure ventilation;IVC: Inferior vena cava(plethoric IVC defined as diameter > 2.1 cm and < 50% inspiratory reduction);LR: Likelihood ratio;LV: Left ventricle;LVEF: Left ventricular ejection fraction;LVSF: Left ventricular systolic function;MAPSE: Mitral annular plane systolic excursion;NPV: Negative predictive value;PE: Pulmonary embolism;PPV: Positive predictive value;RA: Right atrial;ROSC: Return of spontaneous circulation;RV: Right ventricle;TAPSE: Tricuspid annular plane systolic excursion.
General limitations to lung ultrasound include a large body habitus,presence of subcutaneous emphysema and thoracic dressings;these limit obtaining adequate windows[6].Lack of access to training and ultrasound machines also limit more widespread application of lung ultrasound.However,compared to CCE,competency in lung ultrasound can be achieved more quickly with a minimum of 10 scans[7].
ABDOMlNAL ULTRASOUND
While basic cardiac and lung ultrasound features have generally been well-characterized individually,abdominal ultrasound features have instead been studied in the context of integrated protocols.The Focused Assessment with Sonography for Trauma(FAST)incorporates scanning the abdomen,heart,pericardial and pleural spaces in a trauma patient.This subsequently incorporated basic thoracic injuryassessment in form of extended FAST(E-FAST).In FAST,abdominal sonography focuses on detecting free fluid in the abdominal cavity which indicates hemoperitoneum associated with significant abdominal injuries.The 4 sonographic views in the FAST exam are the 4 Ps: Pericardial,perihepatic,perisplenic,pelvic regions.The limitations of FAST are that it has low accuracy in the very early postinjury phase,and does not detect retroperitoneal bleeding well.It does not detect early solid organ injuries not accompanied by significant bleeding.It does not replace traditional imaging modalities if there are penetrating injuries[8].Extended FAST further incorporates basic lung ultrasound to detect pneumothoraces or hemothorax,which has a sensitivity of 78.6%-95.3%(68.1%-99.2%)and specificity of 98.2%-99.8%(97.0%-99.9%)compared to traditional clinical examination and radiological imaging with chest X-ray or CT[8].Other than FAST,abdominal POCUS in the critical care setting also includes assessing the bladder(to detect retention of urine),kidneys(for hydronephrosisetc.),gallbladder(for cFhigoulercey 3s.titisetc.),and abdominal aorta(for abdominal aortic aneurysms).Some examples are shown in
POCUS PROTOCOLS
Since 2001,intensivists and emergency physicians have come up with protocols that integrate the key features of basic cardiac,lung and abdominal ultrasound.These protocols are used to confirm or eliminate certain diagnoses in a stepwise manner.Clinicians perform POCUS as an extension of the physical examination in a problem-oriented approach,and scans are often repeated post intervention.
As with all ultrasound procedures,POCUS is operator dependent.Some of the protocols described also require advanced CCE competencies.The more recent protocols tend to integrate multiple POCUS modalities,and have stepwise diagnostic questions to be answered depending on the clinical context.For lung ultrasound,different protocols have different number of points to assess,which is based on the clinical experience of the authors.Some other examples,which are used to explore causes of shock and cardiac arrest,are listed in Table 3.We also included some protocols which only involved one POCUS modality due to its integration in other protocols(BLUE protocol)[9],or the unique pathophysiological question it tries to answer(VeXUS)[10].The clinical benefits of the protocols described below are still pending further study.
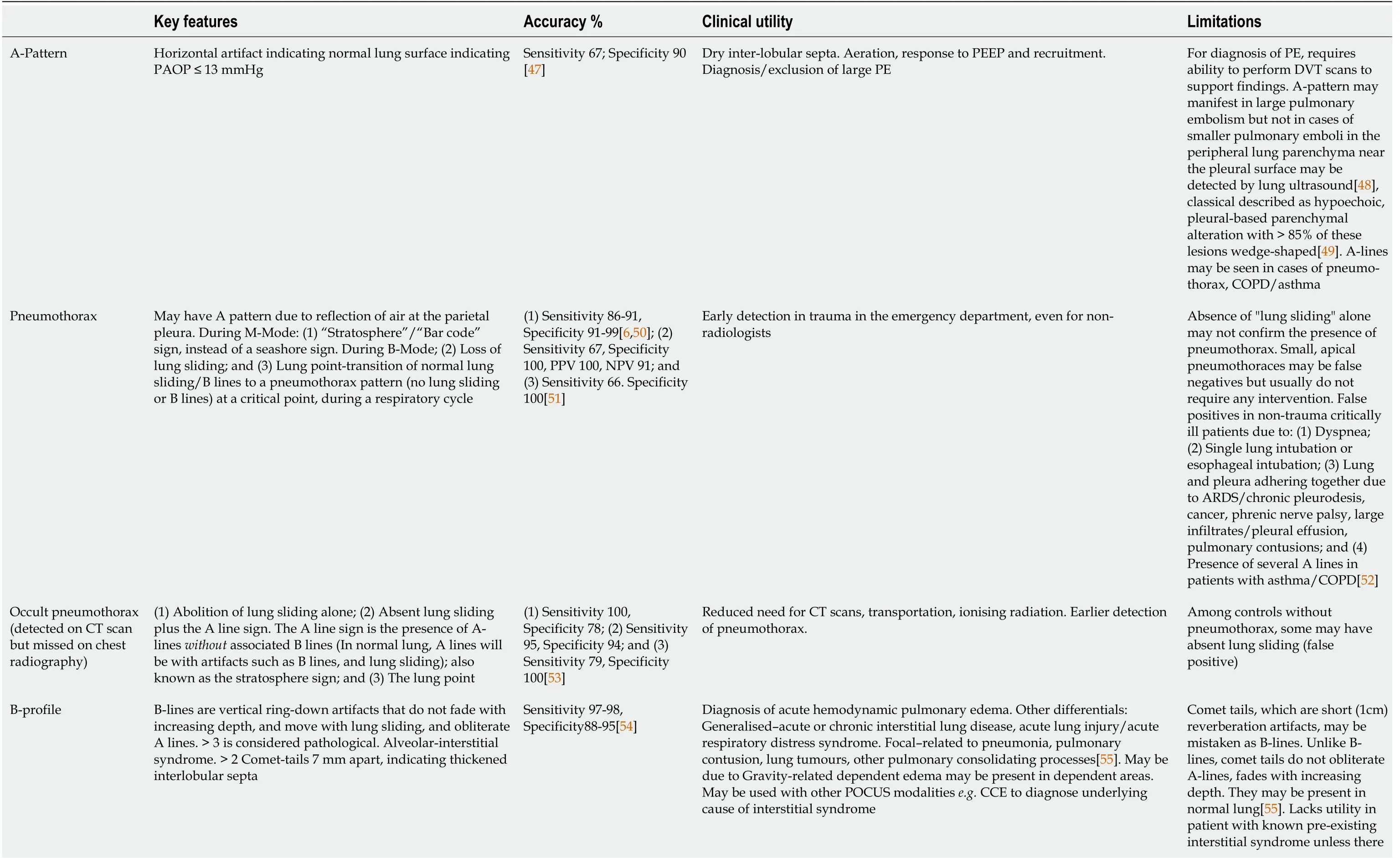
Table 2 Characteristics of basic lung ultrasound
ARDS: Acute respiratory distress syndrome;COPD: Chronic obstructive pulmonary disease;CT: Computed tomography;DVT: Deep vein thrombosis PAOP: Pulmonary artery occlusion pressure;PE: Pulmonary embolism;PEEP: Positive end expiratory pressure;PLAPS: Posterolateral alveolar and/or pleural syndrome,a posterior continuation of the lower BLUE point.
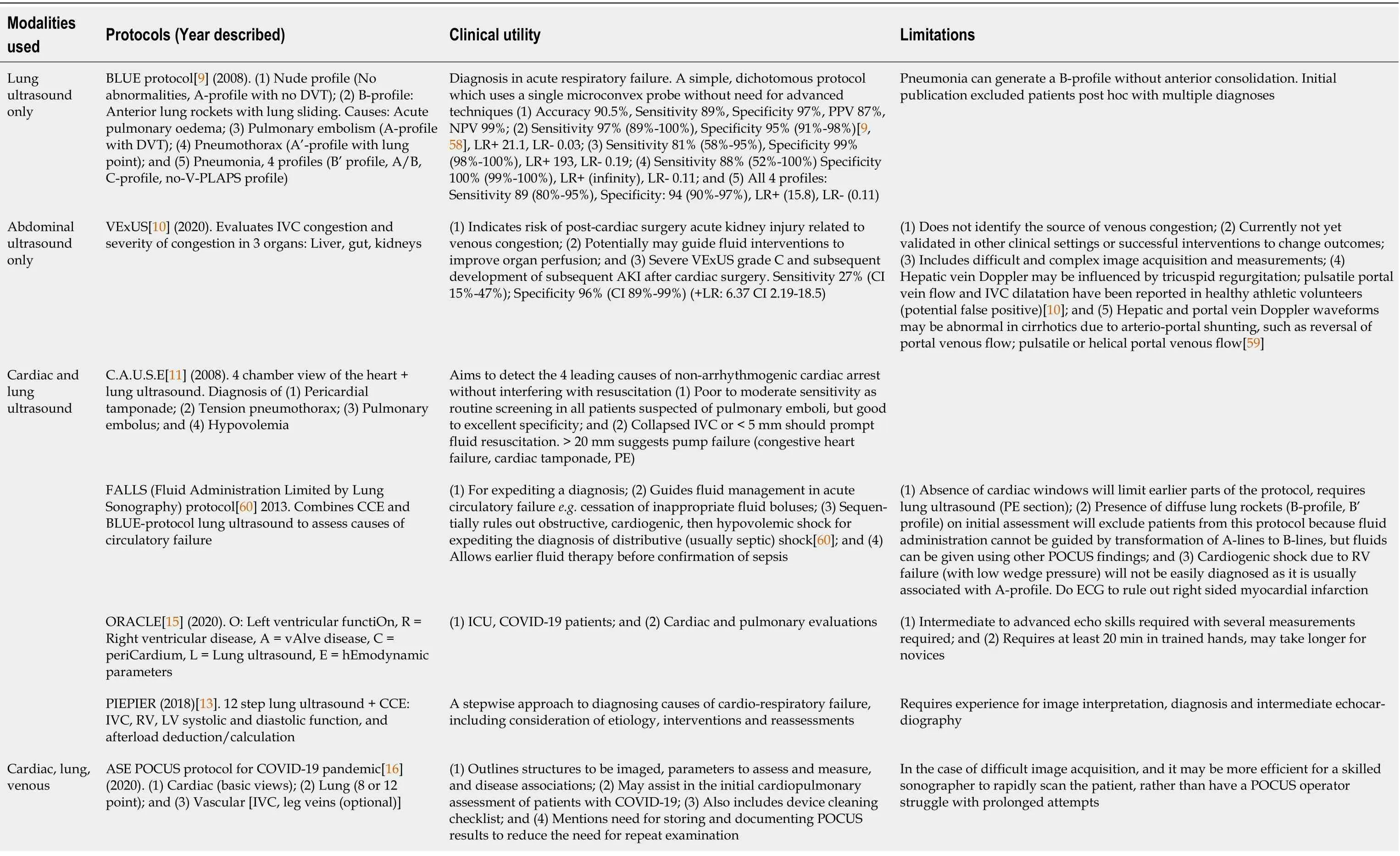
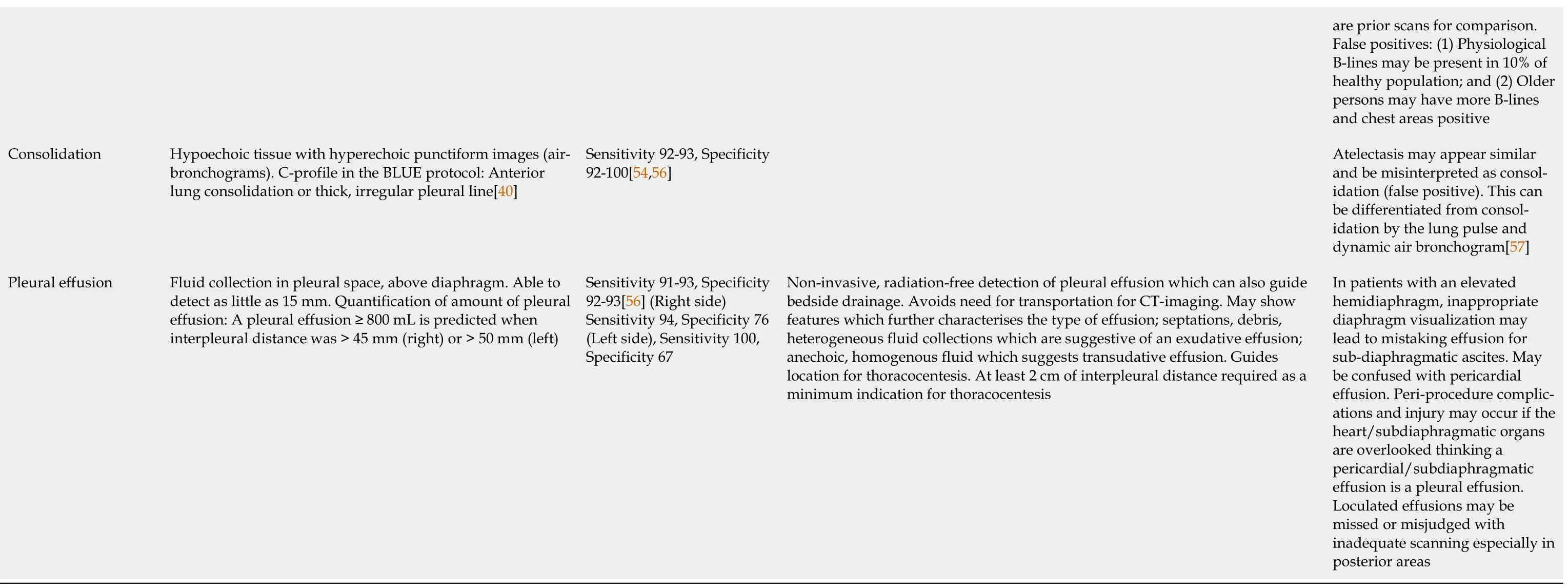
Table 3 Point-of-care ultrasonography protocols in intensive care unit and emergency departments
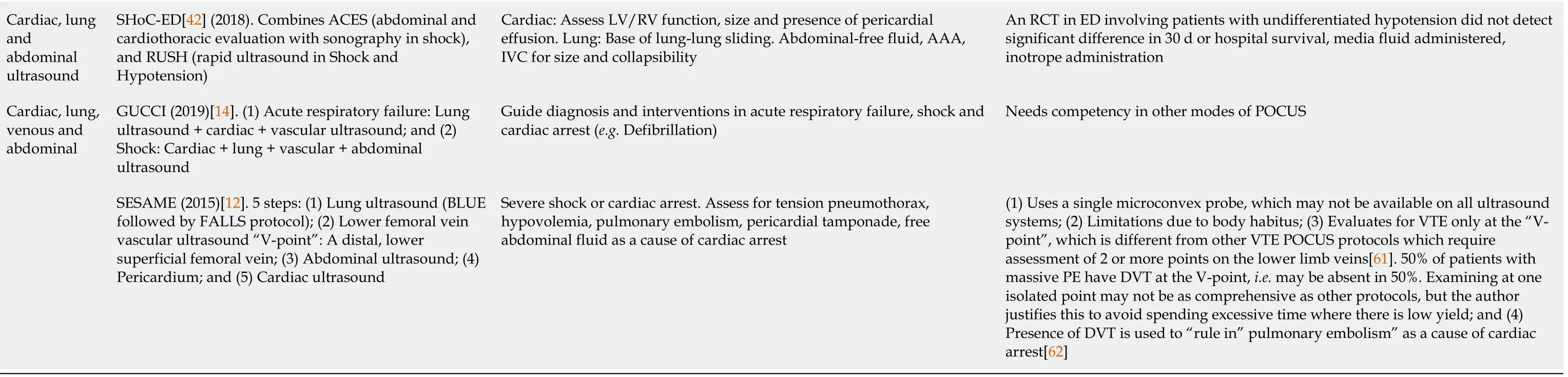
AAA: Abdominal aortic aneurysm;AKI: Acute kidney injury;A4C: Apical 4 chamber;CCE: Critical care echocardiography;DVT: Deep vein thrombosis;ED: Emergency department;FAST: Focused assessment with sonography for trauma;IVC: Inferior vena cava;LR+: Positive likelihood ratio;LR-: Negative likelihood ratio;LV: Left ventricle;PE: Pulmonary embolism;PLAPS: Posterolateral alveolar and/or pleural syndrome;PLax: Parasternal long axis;POCUS: Point-of-care-ultrasound;RCT: Randomised controlled trial;RUSH: Rapid Ultrasound in Shock and Hypotension;RV: Right ventricle;VEXus: Venous Excess Ultrasonography Score;VTE: Venous thromboembolism;ICU: Intensive care unit.
The C.A.U.S.E.protocol[11]aims to detect the common diagnoses that may explain a cardiac arrest,such as cardiac tamponade,severe hypovolemia,pulmonary embolism and pneumothorax.It involves 2 sonographic perspectives of the thorax: The 4 chamber view(the subcostal view is recommended),and the anteromedial views of the lung and pleura at the second intercostal space,at the midclavicular line.
The SESAME protocol[12]was initially described for shock or cardiac arrest,aiming to identify the commonest causes,or easiest causes to diagnose or manage.It uses a single microconvex probe which is available on most ultrasound systems.The steps are as follows:(1)Lung ultrasound(BLUE followed by FALLS protocol),because of convenience and it quickly indicates if a fluid challenge is appropriate;(2)Lower femoral vein vascular ultrasound or abdominal ultrasound to detect deep vein thrombosis or free fluid in the abdomen respectively;and(3)This is followed by pericardial and cardiac ultrasound.The benefit of this protocol is that it uses a single “universal” probe which saves time in a crisis.
The PIEPEAR[13]protocol is a 7-step protocol used in the setting of acute clinical deterioration of a critically ill patient.It describes a thought process,and incorporates POCUS assessments:(1)Identifying deranged physiological systems;(2)Screening for causes;(3)Focused ultrasound exam;(4)Making a presumptive diagnosis;(5)Exploring an etiology,including other investigations;(6)Initiating treatment;and(7)Repeating the focused ultrasound to assess the response to treatment,and titrating the treatment accordingly.It includes a 12-step lung and cardiac ultrasound sequence involving inferior vena cava(IVC),right ventricle(RV),left ventricle(LV)systolic and diastolic function,and afterloaddeduction/calculation.
Another protocol is the Global Ultrasound Check for the Critically Ill(GUCCI)protocol,which integrates multiple protocols[14]and is organised based on 3 syndromes(acute respiratory failure,shock,cardiac arrest)and includes ultrasound-guided procedures.Compared to PIEPEAR,it has specific diagnostic questions to be answered,and has direct,specific management implications.
The ORACLE[15]protocol was designed for ICU patients with coronavirus disease 2019(COVID-19)infections(O: Left ventricular functiOn,R: Right ventricular disease,A: vAlve disease,C: PeriCardium,L: Lung ultrasound,E: hEmodynamic parameters).It was designed such that POCUS is performed in a structured way while reducing additional staff(e.g.sonographers)exposure to infection.Images were acquired during ward rounds and offline measurements were done outside patient rooms.
FUTURE DlRECTlONS AND RESEARCH
POCUS has proven to be essential in triaging cases in the current COVID-19 pandemic,due to availability of relatively portable devices which are easy to disinfect.It reduces the logistical challenge of transporting patients to radiology suites or echocardiography units.The American Society of Echocardiographers(ASE)protocol combines cardiac,lung and vascular ultrasound and is an option for COVID-19 patients where cardiopulmonary disease requires evaluation.An added advantage of intensivists using POCUS is reducing exposure to other personnel and locations,permitting conservation of personal protective equipment[16].
Recently,POCUS has started to appear in the secondary survey of adult cardiac life support(ACLS)algorithm,and can be considered especially if it does not interfere with algorithm.This is to identify potentially reversible causes for cardiac arrest[17]or to detect return of spontaneous circulation(ROSC).Depending on the type of shock or history preceding cardiac arrest,targeted CCE may identify clues to the underlying cause such as a plethoric IVC and absence of lung sliding associated with tension pneumothorax,or small/normal ventricles and collapsed IVC due to hypovolemic shock.CCE may also identify tamponade,thrombus-in-transit,myocardial infarction as a cause of cardiac arrest[18].However,the International Liaison Committee on Resuscitation(ILCOR)task force recommends that the individual performing POCUS is trained to minimise interruptions to chest compressions.With regards to prognostication,ILCOR currently suggestsagainstthe use of POCUS for prognostication during cardiopulmonary resuscitation due to weak evidence for any CCE findings in predicting outcomes.Although a single small randomized controlled trial(RCT)found no improvement in outcomes with use of cardiac ultrasound during cardiopulmonary resuscitation,this result is not definitive and more research is required[19].
There are other modalities of POCUS,although less commonly performed,that can be useful in the ICU.These include airway ultrasound,screening for deep vein thrombosis(DVT),diaphragm ultrasound and ultrasound to assess the optic nerve sheath diameter.Pre-procedural airway ultrasound improves safety prior to a percutaneous tracheostomy[20].Diaphragm ultrasound can be used to detect diaphragm dysfunction with great accuracy[21].Optic nerve sheath diameter ultrasound allows detection of raised intracranial pressure at the bedside and can be used for prognostication post cardiac arrest[22].Evidence for utility of these POCUS modalities in changing patient-centred outcomes is still lacking.Additionally,the training requirements and learning trajectory remain areas for further development and research.
Currently,there has also been increasing interest in the use of artificial intelligence that provides realtime guidance for probe placement,aids acquisition of optimal images[23],and helps to reduce exposure of healthcare workers to highly infectious cases[24].Such technology has also been used to help users identify anatomy and do measurements of cardiac function[23].Whether these algorithms are able to replace a trained sonographer,improve scan durations and accuracy,and improve healthcare delivery or patient outcomes remain uncertain.Robot-assisted ultrasonography,with scans conducted by operators remotely,has also been described.These devices are 5G-powered with robotic arms manipulated by an operator in another room using a simulated robotic hand[25].
There are currently few studies evaluating if CCE or multi-organ POCUS has any effect on mortality,which might be confounded by many other factors.One retrospective study found that POCUS done on ED patients prior to interventions such as fluid boluses are associated with care delays and increased inhospital mortality compared to critically ill patients with no POCUS[26].Also,being a diagnostic and monitoring tool,the therapies given are variable depending on the clinician so it will be hard to link POCUS’s utility directly with mortality.More studies are nonetheless needed to explore the effect of POCUS on patient-centred outcomes.
Given the multitude of POCUS protocols described,there will unlikely be head-to-head studies or standardization of included devices.Each medical unit needs to adopt POCUS protocols that are relevant to its clinical practice.This process must involve multi-disciplinary stakeholders and trainers so that it remains relevant during different parts of a patient’s hospitalisation.This then leads to standardised curricula so that there can be quality assurance and reduction of inter-operator differences.More importantly,the systemic adoption of POCUS protocols can allow patient-centric outcomes to be studied.Needless to say,access to a point-of-care ultrasound machine is critical in adoption of POCUS on a regular basis.Given how each patient’s critical illness,response to treatment and subsequent trajectory lie on a continuum,it would be useful if the unit has a picture archiving and communication system(PACS)to allow different healthcare providers involved in the care of the patient at different stages of the hospitalisation to compare the images.This system also can be used for POCUS education or competency assessment of POCUS learners by their supervisors.Even without a PACS system,this also can be achieved on ultrasound systems which allow storage of video or still clips.Such documentation may be increasingly important for oversight of POCUS practice,which is one of the concerns raised by the Joint Commission in naming POCUS as one of the top 10 health technologyhazardsin 2020[27].
Hand-held POCUS as an extension of physical exam(i.e.stethoscope)is becoming more popular.If POCUS is integrated with structured assessments such as ACLS(Advanced cardiac life support),advanced trauma life support(ATLS),CERTAIN(Checklist for Early Recognition and Treatment of Acute Illness and iNjury),and teams are equipped with ultrasound devices,it can provide additional information at the bedside which may change management.This includes right-siting of patients to the relevant medical disciplines(e.g.a dissecting aortic aneurysm sent to a hospital with cardiac surgery facilities),or pericardiocentesis in a patient who has shock due to tamponade.Pitfalls of incorporating POCUS to routine assessments include inappropriate use of this tool,misdiagnoses by inexperienced operators,excessive time taken,and distraction from clinical assessment and critical resuscitation tasks.POCUS was associated with longer pauses during cardio-pulmonary resuscitation especially comparing between ultrasound-fellowship trainedvsnon-fellowship trained operators[28].If it becomes integrated in such structured assessments,teams must be mindful of the caveats and ultrasound operators should be adequately trained,with safety mechanisms inbuilt(e.g.strict timekeeping for pulse-checks and interruptions in cardiopulmonary resuscitation).Such training may also need to focus on POCUS views which are more easily accessed during a resuscitation situation such as anterior lung,and subcostal echocardiography windows.
The quality of handheld devices is still lacking compared to traditional point-of-care-ultrasound systems,which may lead to poorer image quality or artefacts and misinterpretation.This is an area that is rapidly expanding with newer devices that are smaller coming out in the market,including probes that can be connected to smart devices,and recently artificial intelligence-integrated handheld devices.
CONCLUSlON
Cardiac,lung and abdominal ultrasound should be part of the skillset of doctors managing critically ill patients.Being operator dependent,the accuracy of POCUS in detecting or excluding abnormalities may be influenced by the operator’s experience.The influence of POCUS findings on treatment also depends on clinician experience.Several protocols combining different POCUS modalities have been described but the validity of these protocols in different settings still needs to be studied.There is a growing body of evidence describing the accuracy of POCUS applications,and with growing experience and competency one hopes that the accuracy will improve.POCUS should be considered a tool to confirm a diagnosis,as an extension of physical examination.More evidence is needed to recommend it as standard of care.
FOOTNOTES
Author contributions:Lau YH wrote the manuscript;See KC provided supervision and revised the manuscript.
Conflict-of-interest statement:See KC has received honoraria from GE Healthcare and Medtronic,and has no other conflicts of interest to disclose;Lau YH has no conflict of interest to disclose.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Singapore
ORClD number:Yie Hui Lau 0000-0003-1754-7515;Kay Choong See 0000-0003-2528-7282.
S-Editor:Fan JR
L-Editor:A
P-Editor:Fan JR
 World Journal of Critical Care Medicine2022年2期
World Journal of Critical Care Medicine2022年2期
- World Journal of Critical Care Medicine的其它文章
- Potential role of vitamin D in patients with diabetes,dyslipidaemia,and COVlD-19
- Association of latitude and altitude with adverse outcomes in patients with COVlD-19: The VlRUS registry
- Retrospective analysis of aspirin's role in the severity of COVlD-19 pneumonia
- Treatment with neurohormonal inhibitors and prognostic outcome in pulmonary arterial hypertension with risk factors for left heart disease
