Direct anterior approach hip arthroplasty: How to reduce complications - A 10-years single center experience and literature review
lNTRODUCTlON
The direct anterior approach (DAA) was first described by Heuter in 1881 but popularized by Judet starting in 1947[1]. However, it has only recently become popular. In particular, this happened in 2005 following publications by Matta[2,3]. The increase in popularity of DDA is due to the advantages such as less surgical trauma, minimal dissection of soft tissues, shorter rehabilitation times, faster return to daily activities, lower incidence of dislocation. However, the literature reports a higher rate of perioperative DAA complications than other approaches[4-8] like periprosthetic fracture, prosthesis loosening and nerve injury, but the reported complication rates vary widely in the published literature both in the incidence rate and in the type of complication[9-13]. There is not yet consensus concerning the best approach for total hip arthroplasty (THA) and debates are ongoing[14]. The interest on DAA complications is growing in the recent literature, also compared with those of other hip approaches[15-17]. The aim of our study is to analyze the complication incidence rate in a study group with a maximum follow up of 10 years and compare the results with the literature. Furthermore, from the analysis of our learning curve, we can derive the technical and organizational measures that we have taken to reduce the incidence of complications with the use of DAA for THA.
MATERlALS AND METHODS
All DAA-THA patients with one year minimum follow up who were operated at a single high-volume centre (> 450 arthroplasties/year), between January 2010 and December 2019 were included in this study. The exclusion criteria for the use of DAA in our practice were: age more than 80 years, arthroplasties in hip fractures or in osteolytic lesions, patients with body mass index > 35. Clinical data (gender, age, weight and height) and comorbidities (cardiovascular, respiratory, gastrointestinal, nutritional, endocrine, genitourinary) were collected retrospectively from medical records and outpatient control cards. Radiographic data was taken from the hospital database (Picture archiving and communication system).
My mommy says that you lost your daughter and you re very, very sad with a broken heart. Susie held her hand out shyly. In it was a Band-Aid. This is for your broken heart. Mrs. Smith gasped5, choking back her tears. She knelt down and hugged Susie. Through her tears she said, Thank you, darling girl, this will help a lot.
All surgeries were performed using cementless short stems and press fit cup by three surgeons experienced in DAA. Two cementless design of the stem were used. Minimax stem and Versafit press-fit cup (Medacta International, Castel San Pietro, Switzerland) and Fitmore stem and Continuum press-fit cup (Zimmer Biomet, Warsaw, IN, USA). Minimax is anatomically designed, collarless, and made of titanium-niobium alloy (Ti-6Al-7Nb) stem. The neck has a 127 degrees neck-shaft angle with an anteversion of 9 degrees. Minimax stem can be classified as type 6 according to Khanuja[18] because it is curved, anatomic stems that match the proximal femoral endosteal geometry. Fitmore is a straight designed, tapered, collarless and made of titanium stem which is coated proximally with Ti-VPS (Titanium Vacuum Plasma Spray) and rough-blasted distally. The neck has a neck-shaft angle of 127°, 129°, 137° or 140° without anteversion. Fitmore stem can be classified as type 2 according to Khanuja[18] because it is a tapered, wedged and proximal porous coated stem that achieves fixation proximally. According to short stem classification[19], Fitmore stem can be classified as type 4, shortened conventional wedged design.
Final decision whether to use DAA was made by the orthopaedic surgeon, in compliance with the exclusion criteria, operating based on age, fragility, bone morphology, and level of activity of the patient. In a same way, decision whether implant straight or anatomical stem was made by orthopaedic surgeon in compliance with proximal femoral anatomy after pre-operative planning[20,21]. Ceramic on ceramic coupling was chosen and 32 mm or 36 mm head diameter were used in all cases.
The authors collected 394 patients underwent DDA-THA from January 2010 and December 2019, for a total of 412 hips; twelve patients lost to follow-up and one patient who died from causes not related to surgery were excluded from the study. Mean follow-up time was 64.8 mo (range 12-120 mo). Seven stems were revised. One cortical perforation, one trochanteric and lateral cortical wall intraoperative fracture, one diaphyseal fracture, three clinically symptomatic early subsidence and one late aseptic loosening. We also observed 3 periprosthetic fractures B1 according to the Vancouver Classification.Other minor complications not requiring stem revision were 5 undisplaced fractures of the calcar region treated with preventive cerclage, one early infection, one case of late posterior dislocation, 18 case of asymptomatic stem subsidence, 6 cases of lateral cutaneous femoral nerve dysesthesia.
Primary outcomes were stem revision for aseptic loosening and all-cause stem revision. Second outcome was intra-operative and post-operative complications identification. Patient follow-up was performed at 6 wk, 3 mo and then annually post-surgery.
During preoperative and postoperative radiographic controls, anteroposterior and axial hip radiographs were taken with the foot in a neutral rotational position. Femoral geometries were categorized according to the Door classification system[22] using preoperative anteroposterior radiographs of the hip. The calcar-to-canal ratio was calculated by dividing the canal width, measured at 10 cm below the lesser trochanter, by the calcar width, measured at the middle level of the lesser trochanter. Femurs with a ratio of 0-0.5 were considered type A, 0.5-0.75 as type B, and 0.75-1 as type C[23,24].
Alignment of the stem was considered neutral when the vertical axis of the stem was between 0 and 2° with respect to the femoral shaft axis. A varus-valgus alignment was classified as mild in case of misalignment between 2° and 5° and severe when the misalignment of the stem was greater than 5°. The most recent radiographs were compared to the first postoperative clinic radiographs to evaluate bony remodeling and changes in implant positioning. Stem subsidence was diagnosed in the presence of a stem sinking greater than 3 mm, measured on a perpendicular line drawn from the greater trochanter to the lateral edge of the implant. Implant loosening was diagnosed in the presence of subsidence and/or axial deviation in varus/valgus. We judged early subsidence or axis deviation within 6 mo of surgery, late when observed after 6 mo post-operative.
On a Sunday when I went to church alone, Betty handed me a small piece of paper and asked me to read it when I had time. On the slip of paper she had written, “Here are some phrases to think about over an egg enjoyed from an egg cup.”
Sometimes she would go overboard with her enthusiasm. If it was cold, I had on too many sweaters and never could be without my earmuffs. If it was hot, and our apartment was always hot, she would flee to the beaches and hurry me into the ocean. She was a worrying mother, and when a famous family lost their child in a kidnapping, my mother put bottles of coins on the window ledge6 so that, if they fell, she would be warned there was an intruder in the house. And if anyone threatened me at school with a schoolyard confrontation7, my mother would square off with them if she found out. She was my protector, supporter, and the first person who ever made me feel as if I were special, as nowhere else in life.
RESULTS
Acetabular cup anteversion and inclination are a key point for the long-term success of THA and seen as a challenge in DAA-THA. There are some studies suggesting alternative solutions on this issue; Hu[29] described satisfactory clinical and radiographic outcomes achieved by DAA-THA performed in the lateral position. Fluoroscopic guidance is reported to be used to improve component positioning during anterior approach THA, but with still debated results; for example, Rathod[30] depicted a reduction of variability of acetabular cup anteversion using fluoroscopy with the patient in the supine position during direct anterior THA, while Kobayashi[31] revealed potential excessive cup anteversion and flexion implantation of the stem obtained from fluoroscopic assistance by surgeons in their early experience with DAA. In our practice, we do use intraoperative imaging, but especially to check stem size and alignment in order to mitigate the tendency to undersize the femoral implant associated to DAA-THA, as described in our previous work[32].

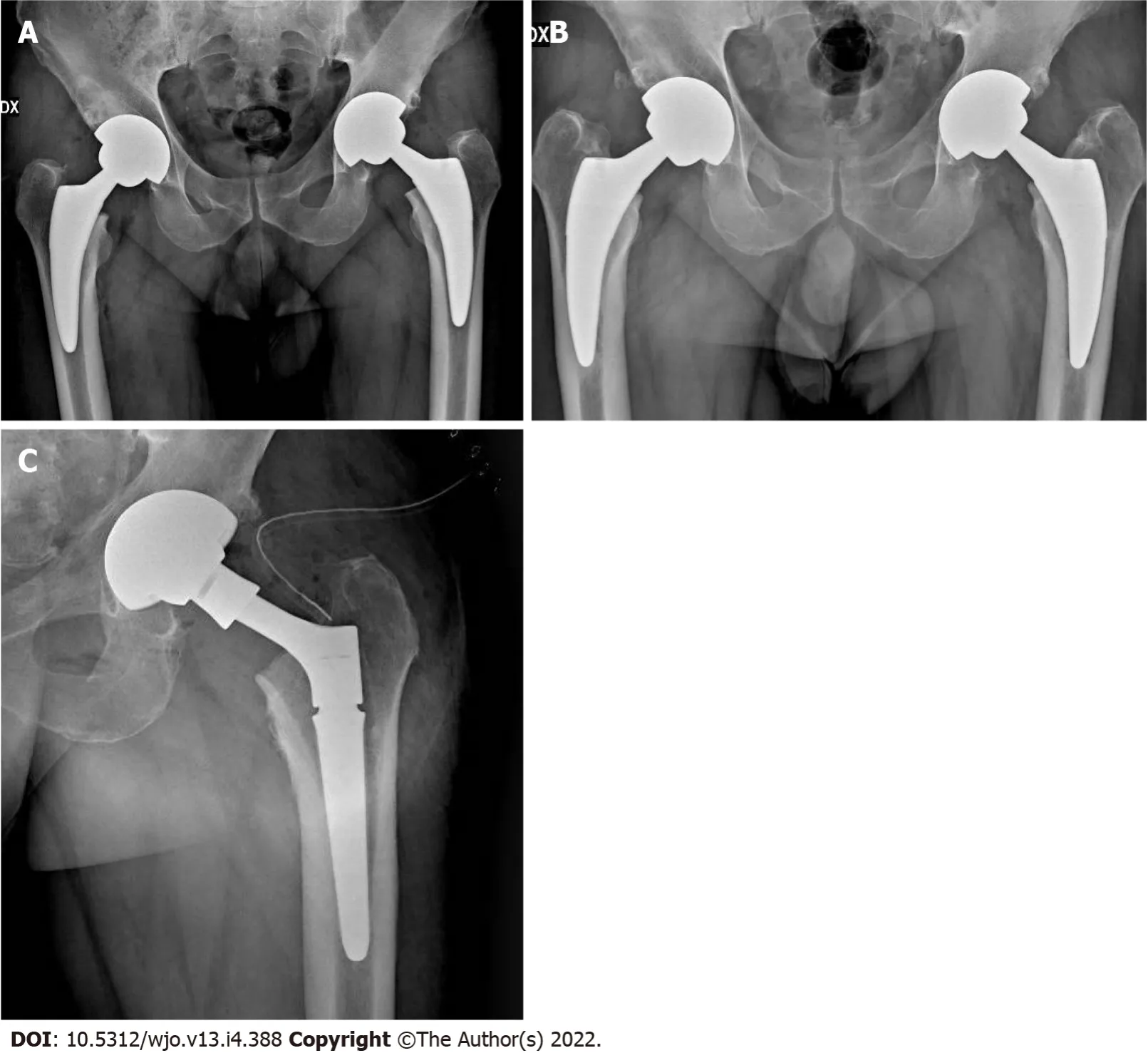
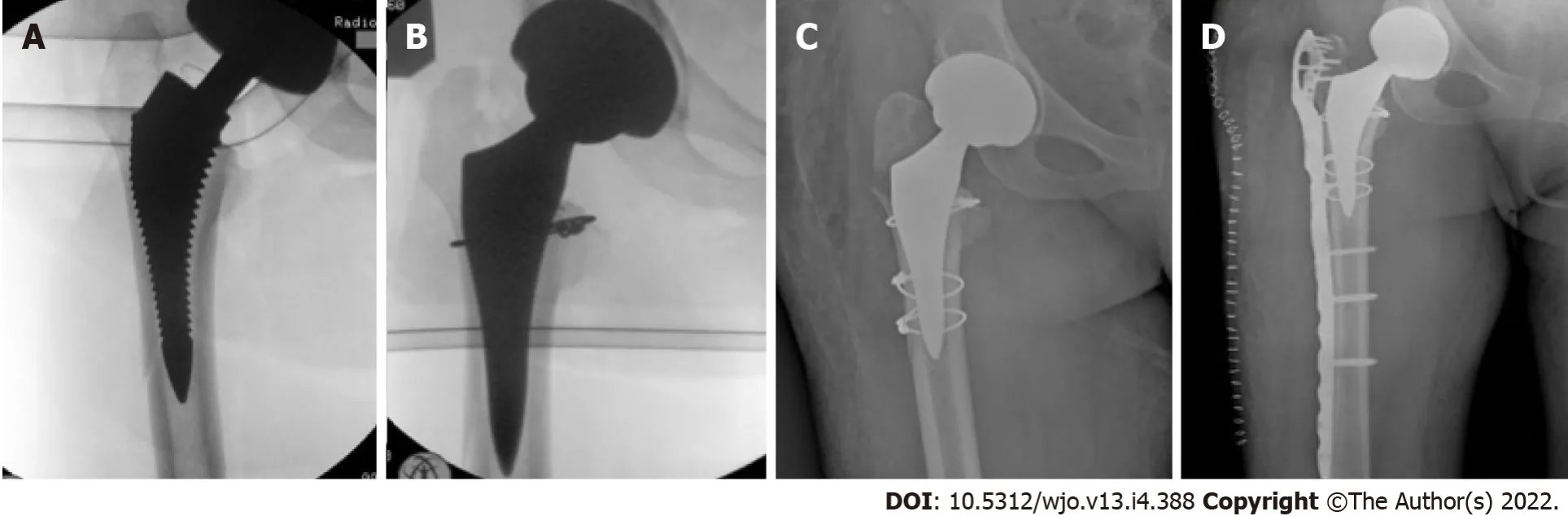
Seven stems were revised. One cortical perforation was observed on postoperative radiographic control and then revised. One trochanteric and lateral cortical wall fracture was intraoperative observed and fixed with cerclage and stem revision. One diaphyseal fracture was treated by plate fixation. Three clinically symptomatic early subsidence revised respectively 5, 6 and 7 mo after surgery. One aseptic loosening 4 years after surgery (Figure 1). We also observed 3 periprosthetic fractures B1 according to the Vancouver Classification. The intra operative complications observed, in addition to the cortical perforation, the diaphyseal fracture and the trochanteric fracture, were 5 un-displaced fractures of the calcar region treated with preventive cerclage (Figure 2). One early infection was treated with surgical washing and head and liner revision followed by antibiotic therapy. One posterior dislocation was observed one year after surgery (Figure 3). Patient referred dislocation during a squat on the ground with the loss of balance. Dislocation was reduced without anesthesia, no further dislocations were observed one year after reduction. Six patients referred numbness or paresthesias within the cutaneous distribution of the anterolateral thigh at follow-up.
According to Dorr classification[17], 168 hips (42%) were graded as Dorr A, 192 hips (48%) as Door B and 39 hips (10%) as Dorr C. In our experience pre-operative planning showed more suitable Fitmore stem for a femoral geometry type A (84/168), according to the Door classification system. This is due to the tapering of the tip adaptable to a narrow femoral canal. Minimax stem is instead more suitable for a femoral geometry type C due to more filling metaphyseal portion (37/39). For this reason, the two groups of patients treated with Fitmore stem and Minimax stem appear not homogeneous and their incidence of complications is not comparable.
In 307 (77%) cases the alignment of the stem was considered neutral, in 76 (19%) cases it was considered mild varus-valgus and in 15 (4%) cases severe varus-valgus. Trabeculae hypertrophy was observed in 84 cases (21%) at zone 3, in 45 cases (11%) at zone 5 and 5 cases (2%) at zone 4. There was grade 1 stress shielding (calcar round-off) in 5 cases (2%). No hypertrophy at zones 8-14 (lateral view) were observed. Stem subsidence > 3 mm, in addition to the one symptomatic case revised, was observed 4 more times (4 mm, 7mm, 6 mm and 10 mm respectively). In all these 4 cases, the absence of pain and the tolerated leg length discrepancy did not compromise the good final functional result.
Finally, 445 (86.4%) surgeries (11 bilateral) were performedthe DAA using a standard operating room table and 54 (19.4%) surgeries (7 bilateral) were performed using the Amis Mobile Leg. Comparison between demographic characteristics and the incidence of complications in the two patient groups (anatomical and straight stem) did not reveal significant differences (Table 2).

DlSCUSSlON
This study was undertaken to evaluate DAA-THA complication rates. For this reason, we retrospectively evaluated clinical and radiographic complications at a mean follow-up of 64.8 mo (range 12-120 mo) in 381 patients (399 hips). All patients received a cementless anatomical short stem or a tapered wedged short stem according to inclusion criteria.
Truly the man would have had no objection to be rich, but he thought to himself: I must first ask my daughter about this, so he went in and told them that there was a great white bear outside who had faithfully promised to make them all rich if he might but have the youngest daughter
Incidence of dislocation is certainly the most relevant result of our study. Commonly considered to be lower than that of others approaches, the small dislocation rate of the DAA is one of the reasons for the great popularity of this approach, although a widely accepted consensus has not been reached yet and some authors report higher complication rates[25].
The fagot-maker grew at last quite out of patience, for she repeated it above twenty times, that they should repent of it, and that she was in the right of it for so saying. He threatened to beat her if she did not hold her tongue. It was not that the fagot-maker was not, perhaps, more vexed16 than his wife, but that she teased him, and that he was of the humor of a great many others, who love wives to speak well, but think those very importunate17 who are continually doing so.12 She was half-drowned in tears, crying out:
We found one case of hip dislocation on 399 hips (0.2%) (Figure 3), which represents the one of the lower dislocation incidences reported in literature in case of large study group[26], with the latest works reporting dislocation rate from 0.23% to 2.5%[27,28].


Despite these good results, the choice of the ideal surgical approach of THA is still controversial and studies on larger samples are needed.
We retrospectively reviewed a group of 394 consecutive patients who underwent DDA-THA from January 2010 to December 2019 of whom 18 were operated bilaterally in a single procedure, for a total of 412 hips; twelve patients lost to three-month follow-up and one patient who died from causes not related to surgery were excluded from the study. The remaining 381 patients (399 hips) were 263 (65.9%) female and 136 (34.1%) male. The average age at the time of surgery was 61 years (range from 28 to 78 years). The preoperative diagnosis was primary osteoarthritis in 328 cases (14 bilateral), avascular necrosis of the femoral head in 38 cases (3 bilateral), rheumatoid arthritis in 11 cases (1 bilateral), traumatic osteoarthritis in 18 cases, and other causes in 4 cases. Demographic data of patients are sumarized in Table 1. Mean follow-up time was 64.8 mo (range 12-120 mo). In 238 cases an anatomical stem was used, in 161 cases a straight stem was used. Three hundred forty-four surgeries were performedthe DAA using a standard operating room table (86.2%) and 44 (13.8%) surgeries were performed using the AMIS mobile leg.
Although the use of different femoral heads size has been described in many studies[33,34], it’s known that the use of larger femoral heads increases the head-neck ratio and consequently increases the range of movement before reaching the point of primary impingement thus reducing dislocation rates, as reported in the published literature[35-37]. Also aware of this, in our series we used only 32 mm or 36 mm diameter heads.
DAA is associated to less surgical trauma, minimal dissection of soft tissues, lower blood loss, shorter rehabilitation times and lower incidence of dislocation. Complication rate can be reduced by mindful patient selection, preoperative planning with proper implant choice, sufficient learning curve, use of intraoperative imaging to check cup and stem orientation and to mitigate the tendency to undersize the femoral implant.
In the literature are reported various revision rates, rising from 0%[39] to 3.3%[28] with different follow up time. In our series, the global revision rate was 1.8% and revision rate for aseptic loosening was 1% at a mean follow up of 65 mo, with particular attention to three clinically symptomatic early subsidence revised respectively 5, 6 and 7 mo after surgery; especially in these cases it is critical, in our opinion, the intraoperative imaging to mitigate the tendency to undersize the femoral implant associated to DAA-THA[32].
The risk of intraoperative fractures is due to the difficult exposure of the femur. Early studies reported a high complication rate with the use of a fracture table[40]. Most of these were avulsions of the greater trochanter. The evolution of specialized traction tables for DAA, promoting greater patient hip positioning than patient hip traction, has reduced the incidence of complications. Although the differences between complications during the traction table or the standard table are still debated in the current literature, the incidence of intraoperative fracture in DAA is reported between 1.3% and 2.4%[41-43]. The use of short femoral stems is described as a reduction in the risk of intraoperative fractures[44-46]. Dietrich[44] reported a significantly reduced fracture rate of 1.6%6.8% in 457 DAA with conventional straight stems. Luger[45] reported 0.9% of intraoperative fractures after 1052 DAA- THA with the same straight stem used in our study. In our opinion, the use of short stems with specific instruments for DAA favors the introduction into the femoral canal, decreases the points of conflict with cortices during introduction and decreases the incidence of complications. We observed 3 major complications (0.7%) related to intraoperative fractures (Figure 4). Our rate of intraoperative fracture increases to 2% including minor complications (intraoperative cerclages due to calcar incomplete fractures). Our results encourage us to continue our experience with short stems, both with the use of the standard table and the traction table[8]. Surprisingly, however, Greco[42] report an opposite experience. They observed higher femoral complications (1.27%) with short stem standard profile as compared to full length standard profile (0.77%). The Authors concluded that short stem may impart greater stress concentration in the proximal femur during broaching and stem insertion which could increase the risk of fracture. On the contrary, a longer stem aids with the direction of broaching and may prevent inappropriate contact against the femoral cortices. One of the Authors has decided to avoid use of the short stem option in elderly female patients given the compounded risk of femoral complication.
Despite DAA utilizes an internervous plane between Tensor fasciae lata and Gluteus medius muscles (Superior gluteal nerve) and Sartorius and Rectus femoris muscles (Femoral nerve), nerve complications are however possible.
Injury to lateral cutaneous femoral nerve (LCFN) is a not rare minor complication. LCFN is a pure sensory nerve is a sensory nerve that forms from the roots of L2 and L3; travels along the posterolateral aspect of the psoas e iliac muscles through the anterosuperior iliac spine, ending superficially at the sartorius muscle. Then LCFN pierces the fascia lata beneath the inguinal ligament and runs laterally and distally within the subcutaneous tissue of the anterolateral region of the thigh. Some authors describe a division of the LFCN into an anterior (femoral) and posterior (gluteal) branch after passing behind or through the inguinal ligament. Rudin[47] classified the branching pattern of the LFCN in three as Sartorius-type (dominant anterior branch on the lateral border of the Sartorius muscle and further branches in the anterior aspect of the thigh), posterior-type [strong posterior branch equal in thickness to, or thicker than, the anterior branch. It runs laterally and crosses the medial border of the tensor fascia lata (TFL) muscle distal to the anterior superior iliac spine (ASIS)] or fan-type (multiple nerve branches of equal thickness on the anterolateral region of the proximal aspect of the thigh, crossing over the TFL and the lateral border of the Sartorius). They reported 36% of sartorius-type, 32% of posterior-type and 32 of fan-type after dissection of twenty-eight cadaveric hemipelves from 18 donors. In contrast to this data, Thaler[48], after a study on 44 Limbs and hemipelves from 22 formalin-preserved cadavers, showed a Sartorius-type branch pattern (70.5%) of the LFCN in the majority of cases, while a posteriortype and a fan-type were detected in 13.6% and 15.9% of cases, respectively. If these data were confirmed, injury to branches of the LFCN should be avoided in most cases by a skin incision 2 cm lateral to the ASIS end its distal extension as lateral as possible.
The true incidence of this complication remains unclear. The reported incidence in literature ranges from 0.1% to 81%. This is due to both the diagnostic difficulty and the degree of accuracy of the clinical examination at follow up. In fact, symptoms ranging from hypoesthesia to painful paresthesias and there is no validated diagnostic tool for LFCN neuropraxia. Patients with LFCN injury often report numbness, paresthesias, or even dysesthesias analogous to meralgia paresthetica within the cutaneous distribution of the anterolateral thigh. In our experience, patients often do not report dysesthesia during postoperative follow-up. The disorder is in fact reported only if the patient is directly questioned about the problem of skin sensitivity. Only in 6 cases patients did report dysesthesia or numbness as a symptom that occasionally caused discomfort. We did not include direct skin sensitivity assessment forms in our follow-up, this is a possible reason of our low incidence (1.5%) of LCFN injury. Homma[49] investigating skin sensitivity problems using a dedicated questionnaire, showed 31.9% of LFCN injury. In the same way Patton[50] reported numbness in 37% of patients with decreasing of incidence to 11% of patients from 6-8 years post op. The fact that symptoms related to LCFN lesion are often reported only after a specific question further suggests that it is a minor complication. Furthermore, in most cases, the presence of LCFN lesions appears to be independent of hip function scores and does not affect final result.
The superior gluteal nerve is a motor nerve, which is formed from the roots of L4 and L5 and the first sacral spinal nerves that supply the gluteus medius, gluteus minimus, and TFL muscles. It runs sideways between the gluteus medius and minimus and then divides into upper and lower branches. Both the upper and lower branches innervate the gluteus medius and minimal muscles. Furthermore, the terminal branches of the inferior branch run anteriorly and supply the tensor of the fascia lata. Precisely these terminal branches represent the anatomical structure at risk. Overstretching the TFL muscle using retractors during surgery or coagulation of the near ascending branch of the lateral circumflex femoral artery can be causes of Injury. There is little information in the literature regarding injury to the TFL with respect to the DAA[51]. The consequences of atrophy of the tensor fasciae are cosmetic, but potential functional deficit is unknow.
Even if in our study we did not consider blood loss, it is reported that DAA THA is related to lower intraoperative blood loss and smaller changes in pre- and postoperative hemoglobin values, less blood drained, and lower volumes of blood transfusions required[52]. Moreover, Zhao[53] described no statistically significant differences in the rate of blood transfusion, hematoma, or re-bleeding between patients undergone ligation of the branches of the lateral circumflex femoral artery pediclethose treated with electrocautery.
There are some uncommon complications that are still to be taken into account; Hogerzeil[6] reported the case of a 69-year-old male patient who developed acute compartment syndrome of the thigh after elective DAA THA while using therapeutic low molecular weight heparin as bridging for regular oral anticoagulation. Also the risk of excessive radiation exposure to both the patients and the surgeons has to be considered; Jinnai[54] compared the intraoperative fluoroscopy time of DAATHA with that of osteosynthesis for proximal femoral fracture to determine if the level of radiation exposure exceeded safety limits and concluding that the intraoperative exposure level was significantly lower and the fluoroscopy time was significantly shorter in DAA-THA than in osteosynthesis.
“You must always remain with me,” said the emperor. “You shall sing only when it pleases you; and I will break the artificial bird into a thousand pieces.”
There are some limitations in this paper. First, the main weakness of our work is the retrospective design of the study. Second, we did not include direct skin sensitivity assessment forms in our followup controls and this could be a possible reason of our low incidence of LCFN injury. Third, the exclusion of ages of more than 80 could be considered a selection bias, improving clinical outcome and reducing the revision rate. Fourth, we did not use radiostereometric analysis to evaluate for stem subsidence, but only manual techniques of measurement.
The Emperor had them brought into a large hall, where the Princess was playingat Visiting, with the ladies of the court; and when she saw the caskets withthe presents, she clapped her hands for joy.
CONCLUSlON
An analysis of the Norwegian Arthroplasty Register found overall similar revision rates between hip approaches, but the posterior approach was associated with more than twice the risk of revision due to dislocation when compared with alternate approaches[38].
ARTlCLE HlGHLlGHTS
Research background
The direct anterior approach for total hip arthroplasty (DAA-THA) is increasing in popularity due to some advantages such as less surgical trauma, minimal dissection of soft tissues, shorter rehabilitation times, faster return to daily activities, lower incidence of dislocation with different reports in the published papers.
Research motivation
Some literature reports a high rate of perioperative complications, with many different rates and complication types among the published papers without reaching a clear consensus.
Research objectives
Research methods
We retrospectively collected data of all DAA-THA patients with one year minimum follow up who were operated at a single high-volume centre, between January 2010 and December 2019. All surgeries were performed using cementless short anatomical or straight stems and press fit cups. Patients’ followup was performed with clinical and radiological evaluation. Primary outcomes were stem revision for aseptic loosening and all-cause stem revision. Second outcome was intra-operative and post-operative complications identification.
Research results
All surgeries were done in all patients with the support of the standard operating room table or the Amis Mobile Leg positioner (Medacta International, Castel San Pietro, Switzerland).
Research conclusions
In our experience DAA is associated to good outcomes and lower incidence of dislocation. According to our results complication rate can be reduced by mindful patient selection, thorough preoperative planning, sufficient learning curve and use of intraoperative imaging.
Research perspectives
Unexpectedly, the case of hip dislocation found in our study was a posterior dislocation occurred after hip hyper-flexion and adduction, factually suggesting an inadequate cup anteversion, since the dislocation after THA performed with the DAA is usually anterior also due to the preservation of the musculo-tendinous attachments of the short external rotators which are important for hip stabilization after arthroplasty. Nevertheless, also Barnett[27] reported a prevalence of posterior dislocation.
Objectives of our study are to analyze our complications and comparing results with the literature reports and to report measures that we have taken to reduce complications rate.
All authors gave substantial contributions to conception and design of the study, acquisition of data, or analysis and interpretation of data, drafting the article and making critical revisions related to important intellectual content of the manuscript and final approval of the version of the article to be published.
The study and follow-up, respecting the criteria of the Declaration of Helsinki, were approved by the ASN/Sav Institutional Review Board.
In this retrospective analysis we used anonymous clinical data that were obtained after each patient agreed to treatment by written consent form; all patients accepted the proposed treatment and follow-up after adequate information and gave written consent. For full disclosure, paper copy is available at SS Annunziata Hospital, Savigliano, Italy.
The authors declare that they have no conflict of interest to this study.
I was a young bachelor then, and Visakhapatnam did not have much to offer. Every Sunday morning, I used to rise before dawn and head for Dolphin s Nose, to enjoy the dazzling spectacle of the sun majestically6() rising out of the sea. The fresh, salty sea breeze was a panacea7 for all the effects of hangovers caused by Saturday night excesses.
When did he come? Was he in the crowd? Wait a bit; we are coming to him! On the third day a little figure came without horse or carriage and walked jauntily27 up to the palace
39. Old witch: Belief in witches exists in nearly every culture worldwide (Leach 1949). In Jungian psychology, the witch is a personification of evil which eventually consumes itself. The witch symbolizes the destructive power of the unconscious (Luthi 1976).
Technical appendix, statistical code, and dataset available from the corresponding author at rivgio@libero.it. The presented data are anonymized and risk of identification is very low.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
I stayed in a simple apartment of a young couple and their three-month-old daughter, Anastasia. Their generosity10 was overwhelming. Although their living conditions were simple, they willingly shared what they had.
Italy
The Snow Queen might come home now when she pleased, for there stood his certainty of freedom, in the word she wanted, written in shining letters of ice
Fabrizio Rivera 0000-0003-0182-6165; Luca C Comba 0000-0001-7008-4455; Alessandro Bardelli 0000-0002-0749-8951.
Wang JL
A
At the foot of our bed is a brass8 chest that is filled with all of the greeting cards Patricia has received from me over the past fifteen years, hundreds and hundreds of cards, each one full of just as much love as the next. I can only hope that our life together will last long enough for me to fill ten brass chests with my weekly messages of love, affection and most of all thanks for the joy Patricia has brought to my life.
Wang JL
 World Journal of Orthopedics2022年4期
World Journal of Orthopedics2022年4期
- World Journal of Orthopedics的其它文章
- Existing fixation modalities for Jones type fifth metatarsal fracture fixation pose high rates of complications and nonunion
- lntegrity of the hip capsule measured with magnetic resonance imaging after capsular repair or unrepaired capsulotomy in hip arthroscopy
- Minimally invasive outpatient management of iliopsoas muscle abscess in complicated spondylodiscitis
- Comparing complications of outpatient management of slipped capital femoral epiphysis and Blount’s disease: A database study
- ls it necessary to fuse to the pelvis when correcting scoliosis in cerebral palsy?
- Lateral epicondylitis: New trends and challenges in treatment
