Cutaneous Manifestations and Treatment Advances of Adult T-Cell Leukemia/Lymphoma
Ying Zhang, Hao Chen∗, Jian-Fang Sun∗
Department of Pathology, Hospital for Skin Diseases (Institute of Dermatology), Chinese Academy of Medical Sciences and Peking Union Medical College, Nanjing, Jiangsu 210042, China.
Abstract Adult T-cell leukemia/lymphoma (ATLL) is an aggressive peripheral T-cell lymphoma caused by the human T lymphotropic virus type-1.The skin is affected in approximately half of ATLL patients,and skin lesions may be the first manifestation of the disease. The skin lesions of ATLL are polymorphous, and depend on the type of skin eruption,which makes it possible for doctors to predict the prognosis of the disease based on the characteristics of skin lesions.In this review article,we describe the clinical manifestations and histopathological patterns of skin lesions in ATLL,focus on its diagnostic and prognostic significance, and also summarize the advances in the treatment of ATLL.
Keywords: adult T cell leukemia/lymphoma (ALL), cutaneous, treatment advances
Introduction
Adult T cell leukemia/lymphoma(ATLL)is a peripheral T cell malignancy caused by human T-lymphotropic virus type-1 (HTLV-1) infection according to the 2016 World Health Organization classification of lymphoid neoplasms.1ATLL was divided into acute, chronic, lymphomatous, and smoldering subtypes based on clinical and hematoserological features and prognostic factors correlated with survival.2Skin lesions with various clinical and histopathological features can be observed in about 50%of patients,and rarely it presented as the first or exclusive manifestation of ATLL without leukemia or nodal lymphoma, especially in smoldering subtype.3Of note,skin lesion plays an important role in diagnosis and patient’s prognosis prediction.We made a searching using the topic words “adult T-cell leukemia/lymphoma”AND“cutaneous” OR “skin lesions” on PubMed and Google scholar databases from 2005.1 to 2019.10, to collect relevant literature for this article. In this article, we describe the clinical manifestations and histopathological patterns of skin lesions in ATLL, focus on its diagnostic and prognostic significance in ATLL, and summarize the advances in the treatment of ATLL.
Pathogenesis of ATLL and molecular background in relation to the skin lesions
HTLV-1 is a human retrovirus. It is endemic in southwestern Japan,the Caribbean basin,South America,and Western Africa. Notably, sporadic cases of ATLL were reported in Fujian province, southeast region of China.4Although HTLV-1 is causally related to ATLL,less than 5%of HTLV-1 infected individuals can develop into ATLL, and the latency period of viral persistence is usually more than 20 years.5
The exact pathogenesis of ATLL is unclear. Recently,researchers have identified Tax, a viral transactivator protein,plays a key role in viral replication and malignant transformation leading to ATLL.6Tax is a 40 kDa phosphoprotein encoded by an open reading frame in the pX region of the HTLV-1 genome. It can transactivate cellular promoters,causing varied protein expression and signaling cascades activation. It also silences cell cycle checkpoints,preventing DNA damage repair and favoring chromosomal missegregation. Of note, several molecules in relation to the skin involvement of ATLL have been reported as follows.
High expressed cutaneous lymphocyte antigen
Tumor cells can express cutaneous lymphocyte antigen(CLA) (CD162), which activates the CLA/CLA ligand(E-selectin) pathway, a predominant adhesion pathway between ATLL cells and vascular endothelium,and plays a key role in the initiation and enhancement of ATLL cells recruiting to the skin.7
High expressed chemokines/chemokine receptors
Tumor cells also express many chemokine receptors,especially chemokines/chemokine receptors (CCR)4,which is known as a transmembrane Th2 chemokine receptor.8Ishida et al.9analyzed the expression of CCL17/TARC and CCL22/MDC, known as ligands of CCR4,in peripheral blood mononuclear cells (PBMCs) and tissues of ATLL patients and healthy volunteers. Revealed both skin lesions and normal skin derived from ATLL patients were positive,whereas PBMCs from both healthy donors and ATLL patients and extracutaneous tissues were negative. As a result, the chemokine ligands expressed on skin play an important role in promoting the migration of CCR4 expressing tumor cells into skin. Sugita et al.10reported an ATLL patient with skin tumors progressed into leukemia due to the loss of CCR4 expression.Moreover, ATLL cells share the CD4+CD25+CCR4+phenotype with regulatory T cells(Tregs),and the ligands on skin may also chemoattract CCR4 expressed Tregs,which further suppress tumoricidal cytotoxic T lymphocytes, contributing to the immune escape of ATLL cells.
High expressed programmed cell death-1 and programmed cell death-ligand 1
PD-1 is a cell surface inhibitory receptor,primary regulates immune system. Kozako et al.11demonstrated that the increased expression of programmed cell death(PD)-1 on both neoplastic and non-neoplastic T cells in skin lesions and peripheral blood in ATLL patients compared to healthy person.They also found augmented expression of programmed cell death-ligand(PD-L)1,ligand of PD-1,on tumor cells compared to non-neoplastic cells in ATLL patients. The PD-L1 on tumor cells may suppress the function of PD-1 expressing CD4+T cells and CD8+cytotoxic T cells in skin, leading to immunosuppression.
Skin lesions of ATLL
About half of ATLL patients present skin lesions,according to the infiltration cells, it can be divided into specific and non-specific lesions.
Specific lesions
The specific lesions of ATLL are polymorphous.It may be the initial manifestation (skin-first) or present at the latestage of ATLL(skin-second).Sawada et al.12analyzed 119 ATLL patients and categorized the skin lesions into six types:patch,plaque,multipapular,nodulotumoral,erythrodermic, and purpuric types. They observed that almost all the skin-first patients were classified as the smoldering subtype and always presented patch and multipapular lesions, while the skin-second cases were more frequently belonged to the acute subtype and showed nodulotumoral,plaque or erythrodermic lesions.Moreover,other specific skin lesions manifesting as ulcerated nodules, vesicular eruption, keloid, sclerodermatous, ichthyosiform, and granuloma-like lesions also have been reported.13-14Of note, different type of lesions may coexist in one patient.Most lesions were asymptomatic,and seldom complained of pruritus.
Non-specific lesions
Patients with ATLL may develop non-specific skin lesions in which tumor cells are absent or not predominant.They may present as chronic actinic dermatitis, lichenoid dermatitis, alopecia areata, erythroderma, and other secondary dermatitis caused by CD8+cytotoxic T cells,which may relate to the elevated immunity to HTLV-1 infected CD4+T cells.15Various superficial or systemic infections,include infection by pathogenic fungi,bacteria,viruses, and parasites can be observed in ATLL patients,may in association with impairment of innate or adaptive immunity.16
Histopathological and immunohistochemical characteristics
Histologically, cutaneous lesions show various degrees of pleomorphiclymphomacell form bandlike,diffuse,nodular or perivascular infiltration pattern (Fig. 1A-1B). Mitotic figures and nuclear atypia are frequently seen.17Eosinophils and histiocytes may be present. The heterogeneity of histology patterns may reflect the different types of skin lesion:patch or erythrodermic type lesions usually manifest superficial banded dermal infiltrate with epidermotropism and Pautrier microabscesses mimicking mycosis fungoides/Sezary syndrome (MF/SS); multipapular or plaque type lesions often show nodular,diffuse or perivascular infiltration pattern in the dermis by small to medium-sized lymphoid cells with convoluted nuclei;nodulotumoral type lesions, however, always show medium to large-sized atypical lymphocytes infiltrating in a diffuse or nodular pattern in the dermis and extend into subcutaneous tissue,imitating peripheral T-cell lymphoma unspecified or anaplastic large T-cell lymphoma.
Immunohistochemically,tumor cells were positive for T cellmarkers:CD2,CD3,CD5,andCD45RO,but mostcells lack CD7. The majority of tumor cells are CD4+CD8-,occasionally CD4+CD8+or CD4-CD8+.Notably,CD25 is specifically positive in vast majority cases (Fig. 1C-1E).CD30 is occasionally expressed in large-sized cells.
Diagnosis and differential diagnosis
The diagnosis of ATLL is based on a combination of the clinicopathological presentation and the evidence of HTLV-1 infection. ATLL should be considered with the following clinicopathological features:primary nodulotumoral lesions in cases suspicious of MF/SS, large atypical lymphocytes infiltrate into epidermis forming Pautrier-like microabscesses or cases diagnosed as cutaneous T-cell lymphoma - not otherwise specified.
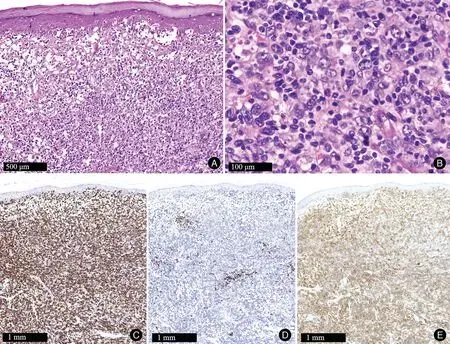
Figure 1. Histopathology and immunohistochemistry of patient with ATLL.(A)Diffuse infiltration of atypical lymphocytes in the dermis and into the epidermis(HE×100).(B)Higher magnification view showing medium to large-sized atypical lymphocytes(HE,×400).Tumor cells were CD3 positive (C), CD20 negative (D), and CD25 positive (E). ATLL: adult T-cell leukemia/lymphoma.
For the striking clinical, histopathological, and immunophenotypical features overlap, ATLL should be distinguished from various cutaneous T-cell lymphomas,especially MF/SS. Clinically, patients with ATLL always show aggressive clinical course with lymphadenopathy or leukemia. The skin lesions in ATLL primarily present as multipapular or nodulotumoral type and purpura is common.By contrast,at the onset of MF,patients usually have, skin lesions only, and experience a long time with patch and plaque stage before nodulotumoral. Immunohistochemically,the most significant phenotypes difference between the skin-infiltrating ATLL and MF are the expression of Leu8 (lymph node homing receptor),HLA-DR and CD25 antigens in the former.18In addition,serum interleukin-2 receptor level is higher in ATLL than in MF,which is a poor prognostic factor for ATLL.19The essential to distinguish ATLL from other diseases is that HTLV-1 is positive in the former both by serology and genomic analysis.
Prognostic significance of the skin lesions in ATLL
Many researchers have suggested that the prognosis of ATLL are associated with the appearance of skin lesions.
Clinically, Tukura et al.20compared the prognosis between ATLL patients with and without skin lesions in each clinical subtype, showed the presence of skin lesions are corresponding to a worse prognosis in the acute,chronic, and smoldering subtypes, other than in the lymphomatous subtype. Marchetti et al.13observed all chronic or smoldering subtypes present skin-first involvement at diagnosis, however, skin-second involved and skin-uninvolved patients were mainly classified as acute subtype and lymphomatous subtype, respectively. They also reported that skin-first involved patients had significantly longer overall survival. Notably, there was no difference after stratifying by clinical subtype.Sawada et al.12performed a retrospective analysis of 119 ATLL with skin lesions. To further evaluate patients’ condition,they applied the T stage of the tumor, node, metastasis and blood classification of MF/SS to ATLL skin lesions.They suggested that the type of skin eruption was an independent prognostic indicator for ATLL: erythrodermic type was the poorest,followed by nodulotumoral and multipapular types,patch and plaque types were associated with better survival rates, and the overall survival was worse as the T stage became more advanced.
Histopathologically, Yamaguchi et al.17suggested the prognosis was poorer in patients with nodular or diffuse infiltration pattern of medium to large-sized cells when compared to those with superficial or perivascular infiltration pattern of small to medium-sized cells, and the MF-like histological pattern was associated with a favorable prognosis. Recently, Cook et al.21proposed a new entity with a poor prognosis: lymphoma type of ATLL, extranodal primary cutaneous variant, which clinically mostly appears as nodulotumoral and histopathologically shows medium or large cells and scant epidermotropism.
Recently, Masaki et al.22reported a significant correlation between higher HTLV-1 provirus load and higher percentage of PD-1 positive neoplastic T-cells in ATLL patients.Higuchi et al.23evaluated 29 ATLL patients with skin lesions found that lesions with PD-1 expression over 50%have more advanced clinical type(nodulotumoral or erythrodermic) and histopathological pattern (nodular or diffuse) and possibly worse survival when compared to those with PD-1 expression under 50% cases, suggested PD-1 may serve as a biomarker to poor prognosis.Miyoshi et al.24recently found that the expression of PD-L1 on neoplastic or stromal cells is a poor or good prognostic marker for ATLL, respectively.
Skin-targeted therapy and treatment advances of ATLL
Skin-targeted therapy
The skin-targeted therapy using topical steroids, topical nitrogen mustard,psoralen plus ultraviolet A,narrowband ultraviolet B or local radiation may be helpful for patients’skin lesions.25Suga et al.26reported a ATLL patient presented as nodular lesion was completely eliminated after local electron beam irradiation. Interestingly, they performed polymerase chain reaction to detect clonal T cell receptor-γ gene rearrangements in the skin lesion before and after irradiation treatment,detected evidence of a rearranged band in the former,but not in the same lesion nor in peripheral blood after treatment. They suggested detecting clonal T cell receptor-γ gene rearrangements is useful for the evaluation of therapeutic effects and the early detection of lymphoma recurrence. Maemoto et al.27retrospectively reviewed 55 courses of radiotherapy for 41 ATLL patients, showed that symptomatic improvement was achieved in 92%of cases,and the mean total radiation dose in the complete and partial response groups differed significantly,was 38 and 25Gy,respectively.Recently,Xu et al.28found that hypericin was highly effective against ATLL cells by induction of apoptosis and suppression of viral transcription, highlighted the promising use of hypericin-photodynamic therapy as a targeted therapy for ATLL.
Targeted host cell surface and intracellular proteins treatment
Several monoclonal antibodies targeting surface proteins on the tumor cells of ATLL have shown encouraging results.CCR4 and its ligands are high expression on tumor cells providing potential targets for ATLL treatment.Mogamulizumab (KW-0761), a novel defucosylated humanized anti-CCR4 monoclonal antibody, which markedly enhances antibody-dependent cellular cytotoxicity activity, has demonstrated strong antitumor activity and dramatically improved the overall survival of ATLL patients.29–30The most common adverse events of Mogamulizumab were infusion reactions(89%) and skin rashes (63%).29However, cutaneous adverse reaction to Mogamulizumab was reported associated with a favorable prognosis, maybe due to Mogamulizumab is cytotoxic to tumor cells not only via antibody-dependent cellular cytotoxicity but also through the induction of CD8+cytotoxic T lymphocytes results from the suppression of CCR4+Tregs.31
Moreover, many inhibitors targeting intracellular proteins have been studied in patients with ATLL and also shown promising results.Such as anti-PD-1 drugs,nuclear factor-k-gene binding pathway inhibitors, DNA replication and repair inhibitors, histone deacetylase inhibitors,proteasome inhibitors, and so on.32
Treatment targeting HTLV-1 Tax protein
Tax protein is recognized as a potential therapeutic target because of its specific role in HTLV-1. Cesaire et al.33reported ST1926, a synthetic retinoid, can downregulate the Tax oncoprotein, upregulate p53 protein, induce cell cycle arrest and apoptosis in HTLV-1 infected cell lines.Ozaki et al.34found cyclosporine A can inhibit the production of Tax in Tax complementary DNA transfected cells and HTLV-1 infected T cells. Xiang et al.35observed that Niclosamide results the degradation of Tax protein in proteasome and inhibits the gene transcription of HTLV-1. Moreover, a newly developed Tax-DC vaccine is currently under phase I trial, revealing a promising efficacy to date. Therefore, Tax-DC vaccine may serve as a safe alternative maintenance treatment for Tax-positive ATLL patients, even as a prophylactic measures to the occurrence of ATLL among HTLV-1 carriers.36
Conclusions
However,the review has following limitations:1)ATLL is rare in the Chinese,and we could not collect enough cases of ATLL and clinical photos. 2) Although it is clear that ATLL is caused by HTLV-1 infection, the exact pathogenesis is unclear. 3) The clinical course of ATLL is heterogeneous, and there is still a lack of consensus treatment guidelines. Patients with ATLL often present skin lesions with heterogeneous clinical and pathological features,which make the diagnosis challenging.Therefore,accurate identification of ATLL associated skin lesions is of great significance for early diagnosis and specific treatment.
Source of funding
The word was supported by the CAMS Innovation Fund for Medical Sciences (No. CIFMS-2017-I2M-1-017),PUMC Youth Fund (No. 3332017168).
- 国际皮肤性病学杂志的其它文章
- Nail Changes as the Initial Sign of Psoriasis:A Case Report
- Tale of Two Alopecias: Alopecia Areata and Central Centrifugal Cicatricial Alopecia Occurring in the Same Patient
- Bullous Pemphigoid: Readability, Quality, and Treatments of Online Health Resources
- Bowen’s Disease on the Left Fifth Finger Successfully Treated with Photodynamic Therapy: A Case Report
- Concurrence of Merkel Cell Carcinoma and Squamous Cell Carcinoma in A Patient with Generalized Actinic Keratosis: A Case Report
- Nail Psoriasis: Treatment Options and Management Strategies in Special Patient Populations

