Access block and prolonged length of stay in the emergency department are associated with a higher patient mortality rate
Ting Cheng , Qian Peng, Ya-qing Jin, Hong-jie Yu, Pei-song Zhong, Wei-min Gu, Xiao-shan Wang, Yi-ming Lu, Li Luo,8
1 Department of Respiratory and Critical Care Medicine, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai 200025, China
2 Institute of Respiratory Diseases, Shanghai Jiaotong University School of Medicine, Shanghai 200025, China
3 Shanghai Key Laboratory of Emergency Prevention, Diagnosis and Treatment of Respiratory Infectious Diseases,Shanghai 200025, China
4 School of Public Health, Fudan University, Shanghai 200032, China
5 Jiading District Center for Disease Control and Prevention, Shanghai 201800, China
6 Department of Statistical Information, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai 201801, China
7 Department of Emergency, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai 200025, China
8 Key Laboratory of Public Health Safety of the Ministry of Education and Key Laboratory of Health Technology Assessment of the Ministry of Health, Fudan University, Shanghai 200032, China
Access block, known as exit block or boarding, is def ined as a situation in which patients who are admitted or planned for admission remain in the emergency department (ED) as they are unable to be transferred to an inpatient unit within a reasonable time frame (no longer than 8 hours).Access block often occurs due to insufficient hospital capacity and is a major issue in emergency medicine.
Patients delayed by access block consume the limited resources of the ED, while other patients are kept waiting for assessment and treatment. Access block is the most important indicator of ED crowding,which is also a global healthcare issue and results in delayed service delivery and poor-quality care.Moreover,patients undergoing access block have increased risks of medication delay, medication errors, and adverse events.Furthermore, access block may inf luence patient mortality rates. While most studies have reported that access block leads to increased mortality rates,some have reported that access block is associated with low mortalityand others showed no significant relationship between these factors.These discrepancies may occur because these previous studies included only patients who were eventually admitted to the inpatient area from the ED.
Few studies have assessed the outcomes of patients who stay in the ED for some time without being admitted to the inpatient area, such as those who leave the hospital directly or are transferred to other hospitals. Therefore, the present study aims to investigate the outcomes of all patients who come to the ED, regardless of whether they are admitted to the inpatient area, to fully assess the impact of access block, and to provide a theoretical basis for initiatives to improve hospital capacity or efficiency to mitigate delays in emergency care.
From August 1, 2013, to September 30, 2016, patients who presented to the observational area of the ED of Ruijin Hospital North, a suburban tertiary hospital in Jiading district, Shanghai, China, were included. Pediatric patients (<14 years), obstetric and gynecologic patients,and patients without vital signs at arrival were excluded.The ED observational area functioned to observe, treat, and resuscitate severely ill patients from the ED and outpatient department. Patients assessed with Emergency Severity Index (ESI, version 4) levels of 1-2 at triage or requiring close observation ordered by the doctors were placed in the ED observational area. There were 5 settled beds and up to 13 additional beds needed. Four doctors and 15 nurses observed and treated the patients on shift. The patients remained in this area until they were admitted to the ward,went home, or were transferred to other hospitals.
S ince access block is a dynamic situation, every patient was categorized into 6 situations at each time point (4 hours,6 hours, 8 hours, 12 hours, 24 hours, 48 hours, 72 hours, 7 days, and 14 days) after arrival at the ED: (1) situation A,admitted to the ward and discharged; (2) situation B, admitted to the ward but died in the hospital; (3) situation C, admitted to the ward and remained in the hospital; (4) situation D,remaining in the ED; (5) situation E, death in the ED; and(6) situation F, departure directly from the ED. At each time point, the outcomes of patients with situations D and C were compared to analyze the impact of access block.
Data on patient demographics, time of arrival, ED arrival by ambulance, ED disposition (discharge, admitted to inpatient area/ward, or death), length of stay (LOS),and mortality in the ED and ward were extracted from the Hospital Information System. Out-of-hospital survival data of the residents of Jiading district were obtained from the death reporting system of Jiading District Center for Disease Control and Prevention (CDC). The main diagnoses and chief complaints were extracted from patient’s records. The main diagnoses were coded according to the International Classification of Diseases(ICD-10) by a clinician and inspected by a medical record coder. The Major Diagnostic Category (MDC)and Adjacent-Diagnosis Related Groups (ADRG) of the patients were grouped based on the main diagnosis using DRG Grouper software, ChinaDRGs(www.chinadrgs.com) according to the CN-DRGsystem.
Count data were presented as the percentage frequencies of occurrence, followed by an analysis of their significant differences using Chi-square tests. Logistic regression analysis was conducted to identify the factors associated with in-hospital mortality. Cox regression analysis was performed to identify the factors related to the risks of death and ED revis it within a short time. Multivariate models were adjusted for all factors that were extracted as potential predictors based on clinical relevance and prior knowledge;i.e., access block or not; ED disposition; age (14-59, 60-79,or ≥80 years); sex; disease categories (classified by the ADRG of the main diagnosis); arrival by ambulance; arrival year, season, weekday or weekend; shift (8:00-19:59 or 20:00-7:59); birth in Shanghai or other places; and whether covered by local health insurance. The forward likelihood ratio method was used to identify the independent variables to build the regression equation. This exploratory model did not consider interaction terms. All statistical analyses were conducted using SPSS version 17.0 (SPSS Inc., USA).Forest graphs were generated using Stata 11.0 (Stata Corp.,College Station, USA).
This study included 4,972 patients (inclusion f lowchart in supplementary Figure 1). Among them, 2,312 patients were residents of Jiading district for whom out-ofhospital survival data were available. The demographic characteristics are shown in Table 1 and supplemen tary Table 1. The proportions of patients in each situation at each time point after ED arrival are shown in supplemental Table 2. Notably, 66%, 41%, and 19% of patients stayed in the ED at 8 hours, 24 hours, and 72 hours after arrival. A total of 1,998 (40.19%) patients were finally admitted to the ward.The mortality rates were 5.83% in the ED and 3.00% in the ward. The in-hospital mortality rate was 7.04%.
To analyz e the impact of access block, the outcomes of patients in situat ions D (remaining in the ED) and C(admitted to the ward and remaining in the hospital at the same time point) were compared for different time points after ED arrival. The results of univariate (Figure 1A and supplemen tary Table 3) and multivari ate (Figure 1B and supplementary Table 4) analyses showed a higher risk of in-hospital mortality for patients at situation D for more than 24 hours compared to that for the patients at situation C. The additional risk increased with the LOS in the ED(adjusted odds ratio [OR]=1.85, P=0.003 for situation D vs.situation C at 24 hours, and adjusted OR=10.78, P<0.001 at 14 days). Mor eover, the results of univariate (Figure 1C,supplementary Figure 2, and supplementary Table 3) and mult ivariate (Figure 1D and supplementary Table 5) analyses revealed a significantly increased risk of death within 30 days after ED arrival among patients at situation D for more than 24 hours. The additional risk increased with prolonged time in the ED (adjusted hazard ratio [HR]=2.60, P<0.001 for situation D vs. situation C at 24 hours and adjusted HR=12.42, P<0.001 at 14 days, respectively).
The risk of death within 30 days after ED departure was signif icantly higher in the patients who left the hospital directly or were transferred to other hospitals than in the patients who were admitted to the ward (mortality 14.6% or 19.2% vs. 6.0%; adjusted HR=2.8 and 2.6, respectively, all P<0.001) (Figures 1 E and F, supplementary Figure 3A, and supplementary Tables 3 and 6).
The risk of ED revisit within 30 days after hospital departure was significantly higher in the patients who left the hospital directly than in the patients who were admitted to the ward or transferred to other hospitals(revisit rate 10.3% vs. 2.5% or 3.6%; adjusted=3.8 and 2.6,=0.001 and 0.028, respectively, Figures 1 G and H, supplementary Figure 3B, and supplementary Tables 3 and 6).
The in-hospital mortality and risk of death within 30 days after arrival at the ED were signif icantly higher in elderly patients and those who arrived by ambulance(supplementary Tables 3-6). The risks of ED revisit within 30 days after hospital departure were lower in older patients (60-79 years or ≥ 80 years) and those who presented in winter (supplementary Tables 3 and 6).
The risks of death within 30 days after arrival at ED were lower in patients who arrived during a surge of more patients to the ED during a single shift (univariable analysis=0.93,=0.031 per additional arrival in the same shift, supplementary Table 3) and higher in the patient arrival at the time ED being more crowding(univariable analysis=1.04,=0.019 per additional patient in the ED at arrival, supplementary Table 3).The results of multivariable analysis are shown in supplementary Table 5.
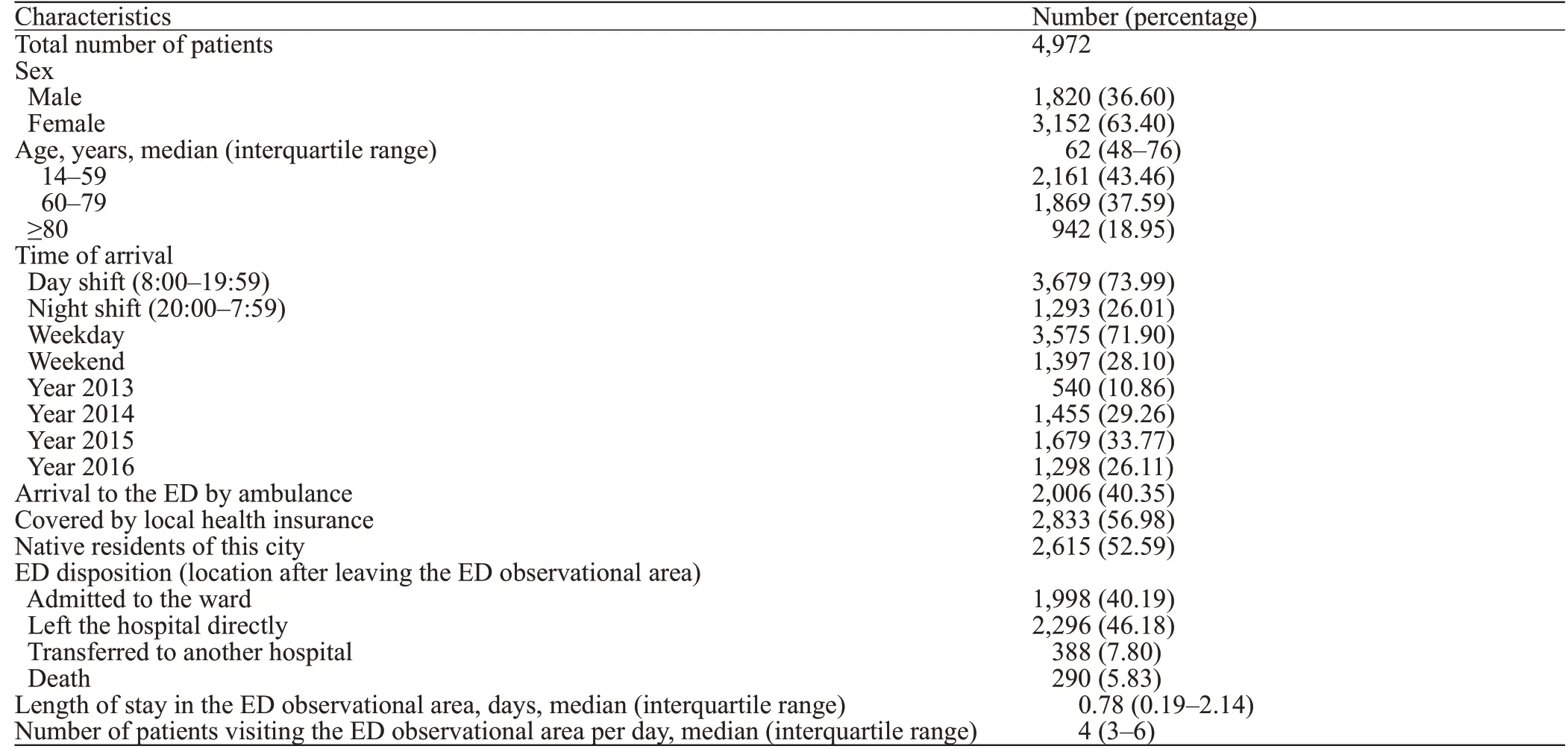
Table 1. Demographic characteristics of the patients admitted to the ED observational area
The results of our analysis of the risk of death in the patients eventually admitted to the inpatient area showed that the risk of death was not significantly higher in patients with a longer LOS in the ED (Figures 1 I-L).
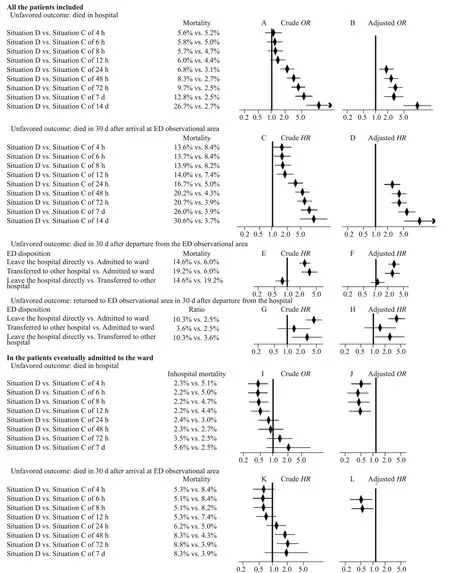
Figure 1. Forest plots showing the impact of access block on patient outcome. A-B: results of univariable and multivariable analyses of the risk factors for in-hospital mortality, respectively; C-D: results of univariable and multivariable analyses of the risk factors for mortality within 30 days after arrival to the emergency department (ED) observational area; E-F: results of univariable and multivariable analyses of the risk factors for mortality within 30 days after departure from the ED observational area; G-H: results of univariable and multivariable analyses of the risk factors for revisit to the ED observational area within 30 days after hospital departure; I-J: results of univariable and multivariable analyses of the risk factors for in-hospital mortality among patients eventually admitted to the ward; K-L: results of univariable and multivariable analyses of the risk factors for mortality within 30 days after arrival at the ED observational area among patients eventually admitted to the ward.
This retrospective study analyzed the impact of access block on patient mortality. Consistent with most previous reports that access block was related to poor outcomes,our results also showed increased risks of in-hospital mortality and death within 30 days after ED arrival in patients who stayed in the ED for longer than 24 hours. This additional risk increased with the LOS in the ED. However, among patients eventually admitted to the ward, the risk of death did not increase with the LOS in the ED, suggesting that patients who waited in the ED but were not eventually admitted to the ward might be the most severe situation for access block. Previous studies included only patients who were admitted to the ward from the ED, and reported that the inf luence of access block on mortality was not signif icant or conflicting (ranging from 0.95to 5.73);however, our study also included patients treated in the ED who were not eventually admitted to the ward. Thus,our results provided more definitive evidence of the adverse impact of access block on patient outcomes.
The causes of access block are complex. Access block reflects an imbalance between health care service demand and supply, especially for severe diseases. Previous studies have shown that the risk of no available beds for emergency admission is discernible for average bed occupancy rates >85% and that bed crises may occur for average bed occupancy rates exceeding 90%.However, the occupancy of our hospital often exceeded 90%, and that of many specialized wards often reached 100%.
The adverse effects of access block on patients outcomes may be attributed to delayed medication and order completion,failure to adhere to guidelines,and neglect of symptom management.In addition, EPs in ED tend to emphasize temporary rather than systemic treatment. Moreover, many nursing interventions, such as oral care, are not applicable in the ED. The observational area of the ED is often crowded and cluttered, which can lead to cross-infection due to difficulties in disinfection and isolation. Lastly, cardiopulmonary resuscitation and death are common in the ED, leading to patient overstressed and sleep deprivation.
Our results also showed that the patients who left the hospital directly from the ED had higher 30-day risks of death and revisit to the ED. This might be due to incomplete treatment, observation, and consultations as well as inadequate planning of care after discharge.Furthermore, the transfer of patients to appropriate facilities has been long considered as an effective measure to alleviate ED crowding and shorten LOS. However, our results showed that while transferring to other hospitals decreased the risk of ED revisit within 30 days, it did not reduce the risk of death. Further studies with a larger sample size are needed to conf irm this observation.
In addition to access block, old age and arrival by ambulance were also identified as the independent risk factors for death. These factors may be associated with patient weakness and disease severity. Moreover, the risk of death within 30 days after arrival was higher when more patients were treated on arrival but lower when more patients arrived during the same shift. Guttmann et alreported an increased short-term risk of death with longer ED waiting time within the same shift at arrival.Thus, we speculate that access block rather than the number of ED visits was a more important factor for ED crowding and threats to patient safety.
The strengths of our study were as follows: (1) its inclusion of patients with access block who were not admitted to the ward to more directly assess the harmful effects of access block; (2) because access block was a dynamic situation, only patients who were admitted to the ward and remaining in the hospital at the same time point(situation C) had the similar disease severity to patients remaining in the ED (situation D); thus, the comparisons of the outcomes of patients between situations D and C might be more reliable; (3) the risk of death within 30 days after ED departure and the risk of revisit to the ED within 30 days after hospital departure were also evaluated as endpoint outcomes.
Our study has some limitations. First, due to the retrospective design, we could only evaluate the associations between access block and patient outcomes but not the causality between them. Second, disease severity might still be a confounding factor influencing the effects of access block on patient outcomes in spite of the delicate multivariate analyses. Third, our study was a single-center analysis. Thus, the results should be extrapolated to other districts with caution and multicenter studies in different districts are needed. Lastly, the causes of prolonged LOS in ED and access block were complex and beyond the scope of the present study. Exploration of the causes of access block will help inform the design of effective strategies to improve patient outcomes.
Our results confirm that access block is associated with poor patient outcomes. Patients who remain in the ED for more than 24 hours and those who leave the ED directly have higher risks of death; and the extra risk increases over time. While transferring patients to other hospitals might have decreased the risk of revisit within 30 days, it does not decrease the risk of death. Our f indings suggest the need for policies to encourage more prompt admission of ED patients to the ward.
This study was supported by the Project of Science and Technology Commission of Jiading, Shanghai (JDKW-2016-W03); the Scientific Research Projects of the Shanghai Municipal Health Commission for Youths (20204Y0016); and the National Natural Science Foundation of China (72174041).
The retrospective cohort study was approved by the institutional review board, which waived the requirement for and written informed consent.
The authors declare that they have no competing interests.
TC and QP contributed equally to this study. LL,YL, TC and QP: conception and design of the research; YJ, HY,PZ, WG and XW: acquisition of data; YJ, HY, PZ, WG and XW:analysis and interpretation of data; YJ, HY, PZ, WG and XW:statistical analysis; LL and YL: obtaining funding; TC and QP:drafting the manuscript; LL and YL: revision of manuscript for important intellectual content. All authors read and approved the f inal manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
