A cadaveric model for transesophageal echocardiography transducer placement training: A pilot study
Ryan W. Horton, Kian R. Niknam, Viveta Lobo, Kathryn H. Pade,4, Drew Jones,5, Kenton L. Anderson
1 Department of Emergency Medicine, Stanford University School of Medicine, Palo Alto 94304, USA
2 Emergency Medicine Residency Program, University of Texas at Austin Dell Medical School, Austin 78756, USA
3 University of California San Francisco School of Medicine, San Francisco 94143, USA
4 Department of Emergency Medicine, Rady Children’s Hospital, San Diego 92123, USA 5 Department of Emergency Medicine, University of Central Florida/HCA Ocala Regional, Ocala 34471, USA
KEYWORDS: Cardiopulmonary resuscitation; Echocardiography; Education; Simulation
Point-of-care echocardiography (POC Echo) is regarded as a useful adjunct in the management of cardiac arrest patients in the emergency department(ED) setting. A number of reports describe the potential prognostic and diagnostic roles of POC Echo during cardiac arrest.POC Echo is also used to monitor and improve the quality and location of chest compressions.More recently, POC transesophaeal echocardiography (TEE) has been gaining popularity among emergency physicians (EPs) in the management of cardiac arrest because higher-quality images can usually be obtained during ongoing chest compressions without being limited by body habitus or the placement of defibrillation pads. These advantages allow for improved compression fraction (shortened pulsecheck pauses) during cardiopulmonary resuscitation(CPR), improved diagnostic yield, and improved chest compression quality via continuous echo monitoring.
With an increased utilization of POC TEE, the American College of Emergency Physicians (ACEP)published guidelines on the use of POC TEE during cardiac arrest in 2017.These guidelines outline the minimum training requirements that should be met for EPs who are already facile with POC Echo. These training requirements generally follow the educational protocol outlined by Arntfield et alin 2015 with the notable exclusion of the bicaval view. The ACEP guidelines state that training can be performed on live humans or simulators; Arntfield et alused simulators for TEE image acquisition training and airway mannequins for TEE transducer insertion training. The use of mannequins and simulators allows EPs, who have limited access to live humans for training, to acquire TEE proficiency. Although TEE simulators likely provide adequate image acquisition training for EPs,who are already experienced with POC Echo, the plastic mannequins that are designed for airway simulation are likely not ideal for simulating TEE transducer placement.More work is needed to develop an adequate simulated TEE transducer placement training model.
In this pilot study, we hypothesized that using a fresh cadaver model for TEE transducer placement training would be feasible and would increase conf idence in TEE placement skills among novice users. We also assessed whether TEE knowledge or confidence was influenced by training level.
This was a cross-sectional convenience sample of emergency medicine resident physicians from a single postgraduate year (PGY) 1-3 training program that participated in an annual procedure education session conducted on a single day. All session participants who had completed at least 25 POC Echo examinations prior to the education session were eligible for inclusion in the study.
Following recruitment and after providing informed verbal consent, participants were given a pre-session assessment to gauge existing TEE manipulation knowledge and confidence levels (supplementary file 1). The pre-session assessment consisted of 10 multiple choice questions regarding TEE manipulation knowledge as well as two questions regarding prior experience with TEE and one question regarding PGY level of training.The pre-session assessment also included a separate question regarding confidence in TEE transducer insertion. Confidence ratings were on a Likert scale of 1 (not at all confident in performing the task) to 5(completely confident in performing the entire task independently without supervision). The assessment questions were developed by three clinical ultrasound fellowship-trained EPs and were tested on an additional five EPs with mixed prior ultrasound experience to validate that the survey items were clear, understandable,and relevant to the construct; the survey that was sent to the study population was the third iteration which had undergone minor changes to increase clarity or to decrease the potential for incorrect entries based on these initial assessment responses.
During the education session, participating residents rotated to the TEE probe insertion station in groups of f ive which were pre-determined by residency leadership;each group consisted of residents from each of the three PGY levels. This was the first year our institution provided a TEE probe insertion station, so none of the residents had received this education in prior years. Each group received a brief standardized didactic and hands-on educational training session, which lasted approximately 20 minutes. The training presented indications and contraindications for POC TEE, knobology, and a demonstration on correct TEE transducer placement;each of the residents then had the opportunity to practice on cadaver models. There were four fresh cadavers available for practice purposes, including the one cadaver used for demonstration and assessment purposes.
Subsequently, each participant individually completed a standardized assessment of technical skill(SATS) on a single fresh cadaver model; the SATS was assessed by two emergency ultrasound fellowshiptrained EPs (supplementary file 2). The SATS was repeated if necessary until participants completed all critical elements as judged by both assessors. The two emergency ultrasound fellowship-trained study personnel who scored the SATS were trained and familiar with the research protocol prior to the event and interrater agreement was assessed using f ive practice subjects who were also included in the analysis.
Participants subsequently completed a post-session assessment with questions similar to the pre-session assessment (supplementary f ile 3).
The delta between pre- and post-session knowledge and conf idence levels were determined, and the number of attempts at the SATS for each participant was recorded.
Descriptive statistics with 95% confidence interval() were used to analyze training level data. Cohen’s Kappa (κ) was used to assess interrater agreement between SATS scoring for the practice subjects.Wilcoxon sign-rank tests were used to compare preand post-session assessments and linear regression was performed between training level and assessment results.Analyses were run using Stata 15.1/SE for Windows(StataCorp, LP College Station, TX).
Twenty-five residents were enrolled during the education session. Twenty-four residents were novices on the POC TEE and all completed the TEE educational training. Levels of training as well as pre- and post-session knowledge assessment scores are shown in Table 1.
There was 100% agreement between the two assessors for the practice SATS (κ =1.0, 95%1.0-1.0). The mean number of SATS sessions required was 1.3±0.5 (95%1.0-1.6) for the PGY1, 1.1±0.3 (95%0.9-1.4) for the PGY2, 1.2±0.4 (95%0.6-1.8) for the PGY3 and 1.2±0.4 (95%1.0-1.3) for all groups combined.
Mean TEE manipulation knowledge and conf idence levels both increased after the training session (Tables 1 and 2). Participants’ level of training did not contribute to the pre-session scores nor to the post-session delta(-value >0.05 for all training levels).
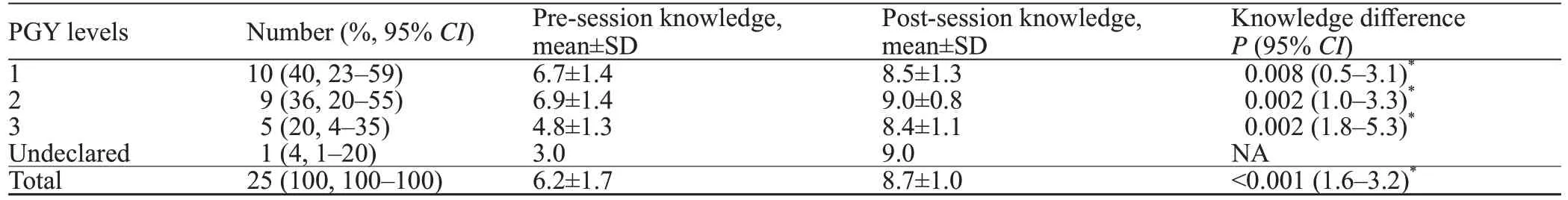
Table 1. Training level of participants and the pre- and post-session knowledge assessment scores
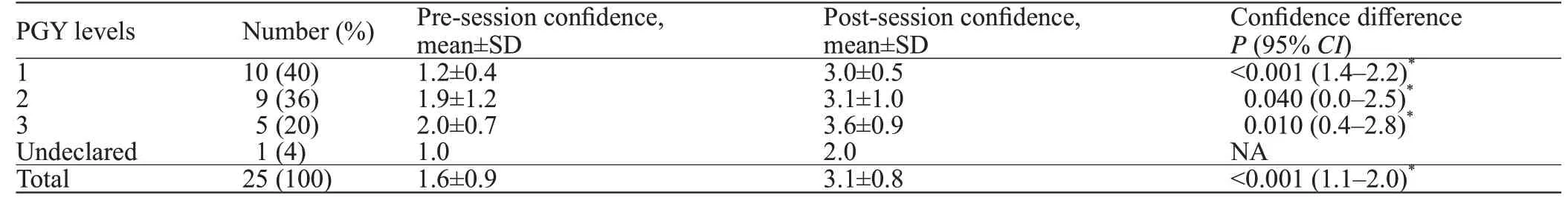
Table 2. Pre- and post-session conf idence assessment scores
This is the f irst study to describe the feasibility of a cadaver model for TEE transducer placement training;one prior study describes the anatomic variation encountered in TEE placement using a cadaveric model.
The relative rarity of cardiac arrest management is one of the limitations to implementing TEE training in the ED setting since the current ACEP guidelines only recommend the use of TEE during cardiac arrest. Thus,an alternative to training solely on cardiac arrest patients is needed. Arntfield et aldescribed an educational protocol that used a TEE simulator to teach image acquisition skills and an airway mannequin to simulate TEE placement since none of the current commercially available TEE simulators have human-like oropharyngeal anatomy. Although an airway mannequin may provide novice TEE users with a rudimentary idea of how to place a TEE transducer, airway mannequins are known to be limited in important aspects such as tissue rigidity,cervical spine mobility, and anatomical proportions.Furthermore, none of these limitations take into account the fact that airway mannequins are designed to simulate endotracheal intubation and not TEE placement.
A cadaveric model allows novice TEE users to experience anatomic variation. The upper esophageal sphincter most commonly lies behind and to the right of the larynx; however, it may also lie directly behind the larynx or side-by-side, which will affect the placement of the TEE transducer.Although rare (<1% in noncardiac arrest patients), esophageal perforation in TEE is often due to using excessive force, poor understanding of anatomic barriers, and unexpected variations in esophageal anatomy.The ability for novice users to experience normal anatomic variation with multiple cadavers and the resistance of human tissue is valuable.
This pilot study was designed to test the feasibility of using a cadaveric model to educate novice TEE users on transducer placement. The variance in knowledge and conf idence may be used to estimate sample size for future work on the subject. Our group plans to expand this model into a mastery-learning exercise that will combine both TEE probe placement and TEE image acquisition as well as simulation of cardiac arrest cases.
This cadaveric model for TEE transducer placement does not assess image acquisition. Unfortunately, in our laboratory, even when the thoracic and cardiac cavities are f illed with saline, the cadaveric cardiac structures are barely recognizable, which limits the use of cadavers for image acquisition training. However, TEE simulators that provide image acquisition training with built-in anatomic variation and pathology are already available and may be used in conjunction with the cadaveric probe placement model.
Our model only used fresh cadavers. The mechanical properties of cadaver tissues are known to change depending on how they are preserved.Whether there is an important difference in regards to improving successful probe placement or decreasing morbidity after training is yet to be determined.
We did not assess the financial feasibility of our training modality. We performed this study in conjunction with an annual procedure education session that used cadaver models for purposes other than TEE education. Institutions with similar training sessions would be best suited to adopt such a model without incurring extra cost, and they would also have the benef it of maximizing the use of donated human tissue. When contrasting the f inancial cost of cadaver models to other models available on the market, one must consider that the cost of cadaver models varies by region. Airway mannequins may be purchased at a fraction of the cost of human cadaver models; mannequins can also be reused with some additional cost for maintenance, but they suffer from the limitations discussed earlier. Synthetic cadaver models have also been used to aid in TEE introduction training, but to date this use has not been described in the medical literature and it is unknown if there is any benefit to using these models over other airway mannequins in TEE education. The f inancial cost of an entire synthetic cadaver is much higher than that of a human cadaver, but the synthetic cadaver may be re-used with some additional cost for maintenance. A synthetic cadaver airway model (partial cadaver) may be similar in cost to a human cadaver in some regions. The limitations of a synthetic cadaver would be similar to any other airway mannequin as discussed earlier.
There was a single participant that did not complete question 13 of the pre-assessment to declare their PGY level of training. We included their data in the analysis under a separate “undeclared” PGY category rather than removing all of their data due to a single missing data point. Fortunately, this was the only missing data in this analysis.
This was a single education session that did not assess retention. Future work will be necessary to determine what training is required for skills retention.
In this pilot study, the use of a cadaveric model to teach TEE transducer placement methods among novice users is feasible and improves both TEE manipulation knowledge and conf idence levels.
None.
The study was approved by the Stanford University Institutional Review Board.
The authors have no competing interests relevant to the present study.
RWH and KLA conceived and designed the study;RWH, KRN, VL, KHP, DJ, and KLA contributed to collecting the data or analyzing and interpreting the data; RWH and KLA contributed to writing the manuscript or providing critical revisions that are important for the intellectual content, and RWH, KRN, VL, KHP, DJ, and KLA contributed substantially to approving the f inal version of the manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
