Palliative care for Parkinson’s disease patients and their caregivers
Zhao Wang, Yue Wang, Zhang-Yi Wang, Chao-Kai He,Xiao-Li Pang
Abstract Parkinson's disease is still incurable and the long-term care needs of patients represent a huge challenge for health systems.Palliative care as an alternative therapy can greatly alleviate the suffering and burden on patients and caregivers through effective medical symptom management,the provision of mental health support,and the development of health plans.This paper explores the current status and challenges regarding palliative care for patients with Parkinson's disease in recent years through a literature review approach.The findings can provide scientific evidence for researchers,clinical practitioners and policy makers in this field.We not only reviewed the systematic and effective therapy, but also concluded a new multidisciplinary cooperation model.TCM teams such as acupuncturists,TCM pharmacists and TCM physiotherapists should be key members of the new multidisciplinary team for the palliative care of Parkinson's disease.
Keywords:Parkinson’s disease;palliative care;hospice care;disease management;caregivers
Background
Parkinson’s disease (PD) is a slow progressive multi-system neurodegenerative disease, commonly in the elderly.Studies have shown that the incidence rate and death rates of Parkinson’s disease are increasing with population aging [1].It is the leading cause of death worldwide.Motor symptoms and non-motor symptoms of patients with advanced Parkinson’s disease will gradually deteriorate.Motor symptoms include dyskinesia, rigidity,static tremors and postural instability.Non-motor symptoms include anosmia, sleep disorder, depression, constipation and other manifestations.These are important factors that affect the quality of life of people with Parkinson’s disease and will exacerbate the cognitive impairment and physical disability of patients.The impact on the patients’ quality of life is often more serious than dyskinesia.At the same time, patients usually develop long-term disabilities and rely on family caregivers to meet their basic daily care needs.Caregivers suffer from insomnia, fatigue, anxiety,depression, guilt and impaired immune response [2].Parkinson’s disease is a chronic lifelong disease.At present, there is no effective method to slow down or halt the progression of the disease [3].Palliative care (PC)refers to the comprehensive and individualized care provided by a professional multidisciplinary medical team for patients with incurable diseases and their caregivers.It is a nursing model committed to improving the quality of life of patients and their caregivers and saving on medical costs.Currently, the object of palliative care has changed from a single cancer patient to a wide range of chronic diseases, such as heart failure and Parkinson’s disease [4].Studies have shown that palliative care can meet the needs of patients with Parkinson’s disease, including symptom control, communication needs and nursing staff support.Its purpose is to alleviate the suffering of patients and their caregivers through physical, psychological and spiritual support [5].Palliative care is now included in national Parkinson’s disease guidelines in the UK [6],USA [7], Canada [8]and other countries.This article summarizes the present situation of palliative care for Parkinson’s disease and provides a reference for future research.
Assessment of palliative care needs for Parkinson’s disease
Studies have shown that the demand for palliative care among Parkinson’s patients increases over time [9].It has been reported that patients with Parkinson’s disease similar to or even more need palliative care than patients with advanced cancer [10].Currently, the palliative care needs of patients with Parkinson’s disease are assessed primarily through needs assessment tools.Needs assessment tools should reflect disease progression and enable a rapid and quantitative assessment of palliative care needs.The palliative care needs assessment tool is based on common symptoms in patients with Parkinson’s disease.It is related according to the effect and frequency of symptoms on patients.Nurses can choose intervention measures to meet the needs of patients according to symptoms of patients with high frequency [11].The Parkinson’s disease needs assessment tool was developed from cancer needs assessment form to specifically assess the care needs of patients with Parkinson’s disease[12].The tool has good reliability and validity and can be used by medical staff to evaluate patients and caregivers.In addition to symptoms,it should also include prognosis, complications (such as pulmonary infection, cognitive impairment, etc.), auxiliary needs, caregiver needs,etc.In addition, the demand for palliative care-related facilities and services is also an important factor in evaluating the quality of palliative care, but the relevant evaluation methods are not clear enough, and the specific requirements for palliative care teams for patients with Parkinson’s disease and environmental evaluation tools still need to be improved.Edmonton Symptom Assessment Scale can score patients’symptoms.It is commonly used for symptom screening and longitudinal monitoring of both clinical and outpatient palliative care patients.The overall score can evaluate the effect of the palliative intervention.It assesses nine common symptoms, such as pain, fatigue, nausea, depression,anxiety, sleepiness, appetite, well-being and respiration [13].A study revised ESAs to form the Edmonton Symptom Assessment Scale for Parkinson’s disease, which covers the clinical symptoms related to Parkinson’s disease, including constipation, dysphagia, muscle stiffness and disturbance of consciousness.It is named the Edmonton Parkinson’s disease symptom assessment scale[14].
The timing of palliative care is different
At present, there is no consensus among experts on when to carry out palliative care for Parkinson’s disease.The main reason is that the prediction method of survival time of Parkinson’s disease is not mature.The uncertainty of survival time will affect the chances of communication between professional nurses and patients, and then affect the opportunity for patients to carry out palliative care.According to the definition of WHO [4] and the British NICE guidelines [5], palliative care for Parkinson’s disease should begin with the diagnosis of the disease.However, clinical studies have also been conducted on when palliative care should be administered, and the duration of the implementation period of the palliative care scheme is still controversial.The evaluation methods for patients with Parkinson’s disease mainly include late symptoms, the British gold standard framework guidelines for hospice care and the American guidelines for hospice care for neurological diseases,etc.as shown in Table 1 for details.
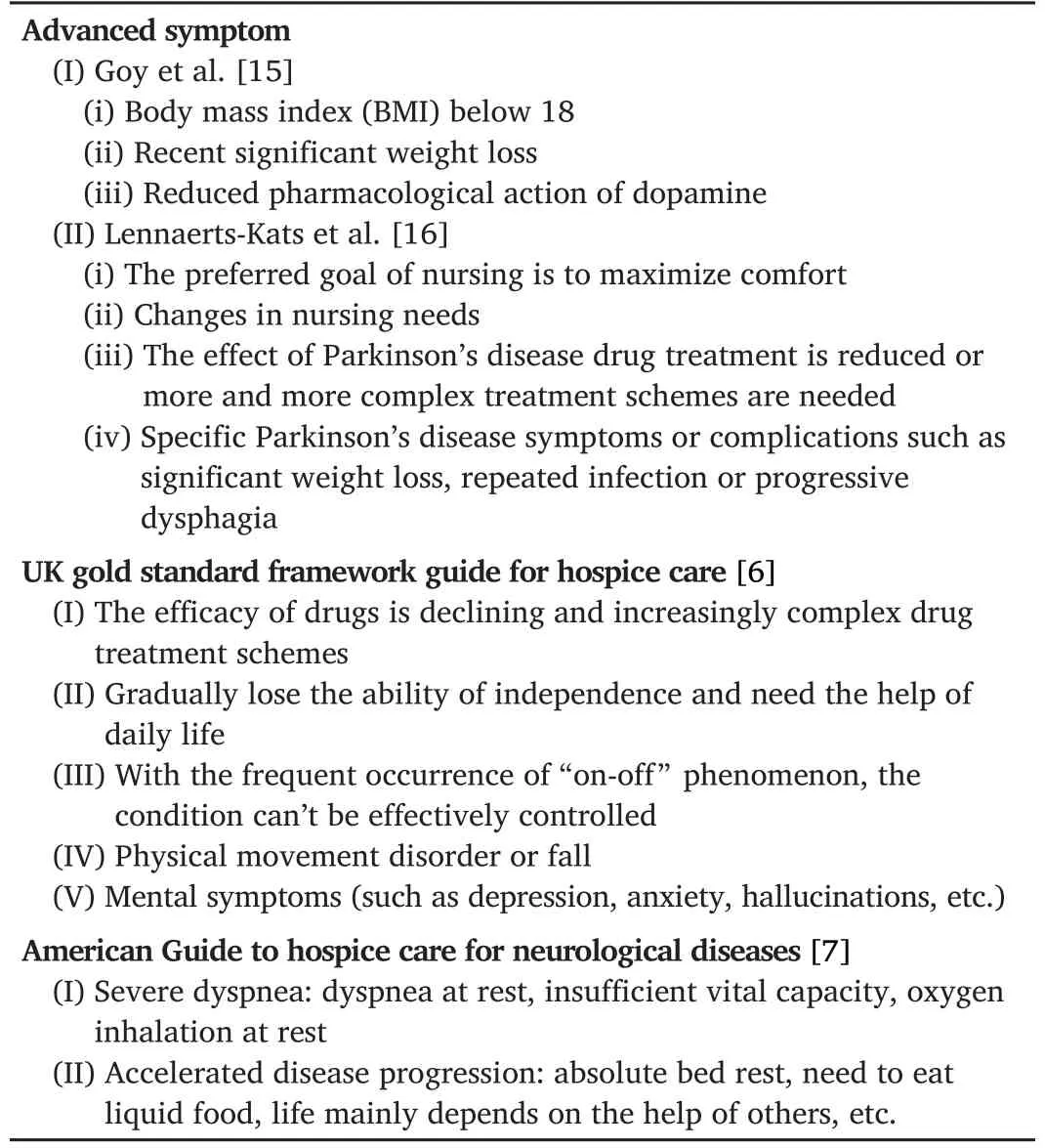
Table 1 Evaluation method of implementation timing of palliative care for patients

Table 2 TCM treatment of Parkinson’s disease
Palliative care should create a multidisciplinary team
It is well known that the symptoms of Parkinson’s disease are complex and the burden on patients and caregivers is heavy.In 2015, the International Conference on palliative care and Parkinson’s disease noted the importance of professional multidisciplinary teamwork in palliative care at the outpatient level, which is essential for the provision of quality palliative care [17].As shown in Figure 1, the team includes neurologists,professional palliatives, Parkinson’s disease nursing experts, chronic neurologists, etc.All members of the multidisciplinary team should receive professional skill training in palliative care in order to provide palliative care intervention to patients, such as the discussing of treatment objectives, disease prognosis and future care planning [18, 19].The nurses should be principal members of this multidisciplinary team,responsible for formulating pre-established medical care plans, guiding patients to fill in relevant medical documents, skin integrity management,nutrition management,medication care and diet care[18].
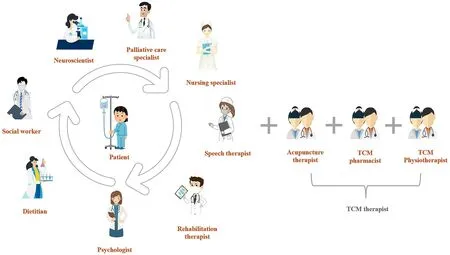
Figure 1.Multidisciplinary diagnosis and treatment model.A patient-centered multidisciplinary team is very important for palliative care of Parkinson's disease.Multidisciplinary team members should include neurologists, palliative care experts, nursing experts, speech therapists, rehabilitation therapists, nutritionists,psychologists,social workers,etc.TCM therapists should be key members of this team,including acupuncture therapists,TCM pharmacists and TCM physiotherapists.
Acupuncture therapists, traditional Chinese Medicine (TCM) pharmacists and physiotherapists could be the characteristic therapists in this multidisciplinary team.TCM characteristic care can not only meet the needs of patients with Parkinson’s disease in many aspects but also minimize side effects and improve the quality of life of patients.Relevantstudies show that acupuncture therapists can treat diseases by needling acupoints on patients’ bodies, and Du Meridian is the preferred acupoint for the treatment of Parkinson’s disease.Similarly, Dan meridian, Gan meridian and Yang Meridian are also effective acupoints [20].TCM pharmacists use TCM therapy to treat patients with Parkinson’s disease,and have made some progress in the clinic.The researchers found that the method of tonifying the kidney and detoxifying can improve the TCM syndrome and cognitive function of patients with mild cognitive impairment of Parkinson’s disease.IncludingRehmannia glutinosa,Cistanche deserticola,Angelica sinensis, Radix Paeoniae Alba, Radix Puerariae,Radix Scutellariae,Coptis chinensisand roasted licorice [21].TCM physiotherapists are responsible for leading patients to exercise rehabilitation training.It is reported that Tai chi and Qigong have good effects on the walking speed and balance ability of patients with Parkinson’s disease [22].Traditional Chinese medicine, acupuncture and traditional Chinese health care therapy have good curative effects on Parkinson’s disease, but there are still some problems in the current related research.A unified and standardized standard for syndrome differentiation and curative effect evaluation has not been formed.In the future, more high-quality research needs to provide more objective and scientific evidence-based medical evidence for TCM treatment of Parkinson’s disease.
Today, some developed countries are collaborating on multidisciplinary cooperative palliative care for Parkinson’s disease.A review of evidence from multidisciplinary team interventions in people with Parkinson’s disease has covered 13 studies including 6 RCTs [23].The studies involved patients with both early and late stage by Hoehn and Yahr staging of disability in Parkinson’s disease.Overall, the multidisciplinary team approach has been shown to improve the health related quality of life and functioning of patients with Parkinson’s disease and the quality of life of their caregivers.The model of multidisciplinary team model abroad has gradually matured.However, due to the shortage of medical resources and the scarcity of palliative care professionals, it is still a challenge to create interdisciplinary teams in developing countries.In our country, for example, the development of palliative care is slow.Due to the lack of formal palliative team, real palliative care has not been carried out in China.In order to truly implement palliative care research in the future,we need to start with the palliative team.The state should strengthen the training of general practitioners and clinical nursing specialists, draw on the experience of foreign palliative care teams, and establish a palliative care team in line with China’s national conditions and suitable for the current medical environment.Building the palliative care force of the primary health care system is very necessary to seek any comprehensive,sensitive and sustainable care model for Parkinson’s disease.In addition,the core skills of general practitioners and neurologists in symptom management need to be developed.At the same time, it is suggested that medical colleges should increase relevant courses of palliative medicine,help medical staff master the skills and knowledge of palliative care,clarify the functions of multidisciplinary team members in palliative care,and lay the foundation for the practice of palliative care practice.
The intervention content was mainly non-motor symptom manage‐ment
Currently, survival rates for patients with Parkinson’s disease tend to be more than 15 years.Studies have shown that non-motor symptoms such as pain, sleep disorders, dysphagia, constipation, anxiety and depression will accompany the whole course of Parkinson’s disease, leading to the decline of patients’ quality of life and serious burden on caregivers [24].Therefore, one of the priorities points of palliative care is the management of non-motor symptoms.First of all, in terms of pain management, we can discuss the goal of pain management with patients, give drugs to nourish
nerves and improve circulation to relieve pain, and take positive and effective measures to prevent pain, such as maintaining joint activity and caring for squashed skin [25].In terms of sleep disorder management,dopamine receptor agonist, melatonin and doxorubicin drug therapy can be considered, and non-drug methods including daily exercise,mindfulness training, cognitive behavior therapy and acupuncture therapy can also be used to treat insomnia [26, 27].In the treatment of dysphagia,patients were given liquid food or semi liquid food, and patients were encouraged to eat more, eat less and eat more.Those who could not eat by mouth were given nasal feeding and intravenous nutrition [28].In constipation management, encourage patients to develop good living habits, regular defecation every day, intake of sufficient fiber and fluid,massage the abdomen for patients, and encourage patients to carry out exercise rehabilitation training [29].In the area of anxiety and depression management, those with mild symptoms can alleviate their psychological burden by relieving negative emotions, while those with severe symptoms can be evaluated by psychological experts in a multidisciplinary team to implement relevant diagnosis and treatment plans, and targeted intervention can be carried out by professional psychotherapy programs such as cognitive behavior therapy, or massage, music therapy and other methods[30].Most studies have shown that palliative care can improve the symptom burden and quality of life of patients with Parkinson’s disease[31-34].However, researchers conducted a study on hospitalized patients seriously affected by long-term neurological diseases in seven palliative care hospitals in the United Kingdom, and the results showed that there was no significant difference between patients receiving palliative care and standard care [35].The heterogeneity of the underlying conditions may be a contributing factor to poor detection results.Patients with multiple sclerosis, motor neuron disease, idiopathic Parkinson’s disease,multi-system atrophy or progressive supra nuclear palsy have differences in pathophysiology, clinical characteristics and natural course.Whether palliative care can improve the symptom burden and quality of life of patients with Parkinson’s disease still lack high-quality evidence support.It is suggested to use a large sample size and heterogeneous groups for further research.
I mplementation of advance care planning
Advance care planning (ACP) means that the patient discusses personal values with medical staff, family members and friends, ascertains decisionmakers, and fill in medical advance instructions, care plans, life support treatment orders and other documents with a clear understanding of the condition, the condition and prognosis and other relevant information[36].ACP is particularly important in palliative care of people with Parkinson’s disease because of the decline in cognitive, motor and decision-making abilities.Studies have shown that in the early stage of the disease, some patients are often reluctant to talk about ACP related issues due to fear, denial of the disease, or hope for treatment [37-41].However, some patients and their families would like to know the prognosis and trajectory of the disease as soon as possible [42].At present, there is no expert consensus on the initial stages of the disease which recommends them to they be treated with ACP in the early stages of Parkinson’s disease [43, 44].However, some experts suggested that ACP should not be discussed at an early stage, as the focus should be on the treatment of the patients [39].Due to the uncertainty of the disease and the patient’s personal factors, it is difficult to accurately judge the timing of ACP initiation.However, due to the uncertainty of the disease and the patient’s personal factors, it is difficult to accurately determine the onset of ACP.Therefore, discussion on ACP depend on the individual and disease characteristics of the patient, such as age, values, attitude,disease progression, disease status and nursing needs [38, 45].Therefore,in the process of palliative care, medical staff should fully respect the patient’s autonomy and decision-making power, continuously communicate the disease progress with the patient and caregivers, and guide patients in establishing pre-established medical care plans to achieve the desired treatment and care for Parkinson’s disease patients and improve the patient’s quality of life.
Support for caregivers of patients with Parkinson’s disease
Caregivers of patients with Parkinson’s disease are both implementers and recipients of palliative care, and play a vital role in home care for patients with Parkinson’s disease [46].With progress of the disease, caregivers'sense of responsibility, social isolation, lack of preparation and the increase of physical and mental diseases also follow [47, 48].A study found that caregivers of patients with Parkinson’s disease generally have expected sadness, depressive symptoms and high care burden [49].Researchers used multidisciplinary psychological education intervention method to intervene caregivers of Parkinson’s disease [50].The research results showed that multi-disciplinary psychological education intervention method can improve the coping skills and psychosocial adaptability of caregivers of Parkinson’s disease, so as to greatly improve the quality of life of patients and caregivers [51].Researchers used a multidisciplinary palliative care method similar to Navarta Sanchez to study 175 caregivers.After 12 months of intervention, caregivers’ burden was reduced the quality of life significantly improved[34].
Conclusion
Parkinson’s disease is in great demand for palliative care.Palliative care should be demand-based and focus on improving the quality of life of patients and caregivers.Advance care planning is an essential part of palliative care.According to individual differences, it is very important to respect patients’ autonomy and decision-making power, and guide patients to establish pre-established medical care plans.In the future, medical staff in multidisciplinary palliative care should be actively trained,multidisciplinary palliative care teams should be established and patientcentered multidisciplinary palliative care interventions should be formulated.The main content of intervention is non motor symptom management, using large sample size and heterogeneous groups to do more in-depth research, and deeply explore the application of palliative care model in Parkinson’s disease.
- Life Research的其它文章
- Molecular mechanism of different viruses associated with autoimmunity
- Utility of convalescent plasma for addressing the COVID-19 infection:brief review and case reports
- Graft rejection after deep anterior lamellar keratoplasty in fellow eye in macular corneal dystrophy:a case report
- Low expression of novel biomarker RCSD1 predicts poor prognosis of lung adenocarcinoma
- Advances of biodegradable magnesium-based implants for orthopaedics
- Intracranial hemangiopericytoma with right-sided aortic arch:a case report and summary of experience