Comparison of the clinical performance of i-gel and Ambu laryngeal masks in anaesthetised paediatric patients:A meta-analysis
INTRODUCTION
Supraglottic airway devices (SGAs) have gained widespread acceptance for use in routine anaesthesia and emergency airway management in children since the 1980s,owing to advantages such as easy insertion,decreased use of neuromuscular blocking agents,hemodynamic stability,and low risk of postoperative airway complications compared with tracheal intubation[1-3].To solve the deficiencies of classic laryngeal masks,including airway leak,gastric insufflation,and risk of aspiration with positive pressure ventilation[4,5],the design of the perfect paediatric SGA has undergone a long and productive evolution leading to i-gel and Ambu laryngeal masks,which are two improvements based on classic laryngeal masks.
The i-gel airway (Intersurgical Ltd.,Wokingham,United Kingdom),a representative disposable second-generation SGA,has been available in small sizes since 2010.Made from a soft medical-grade thermoplastic elastomer with a non-inflatable cuff,i-gel was designed to create an anatomical seal of the pharyngeal,laryngeal,and peri-laryngeal structures while avoiding compression trauma.Moreover,its built-in drainage channel allows for gastric catheter placement to facilitate the efflux of gastric fluids.Studies in children have reported its easy insertion,high oropharyngeal leak pressure (OLP),and few postoperative adverse effects[6,7].However,as some studies have shown that its straighter design makes it prone to sliding out and becoming displaced,it should be cautiously used especially in very small children[8,9].
我不知该怎样表达自己的感激了。我躬着身子,一步一句地道谢林老板。出了总经理室,我迅速给阿花发了个信息:谈得很成功!然后跟着李霞去了抛光车间。不少老同事一见我,欢呼雀跃了,争着说阿坤,要不要我?早就不想在这鸟厂干了。我说不要老朋友要谁?要!我挑了十个人,包括刘建,都是我以前的同事。他们都是大发厂抛光车间的中坚力量,技术非常娴熟。我还担心大发厂舍不得放呢,没想到李霞和夏俊都没提出异议,大概是林强信发了话,他们只有遵照执行了。
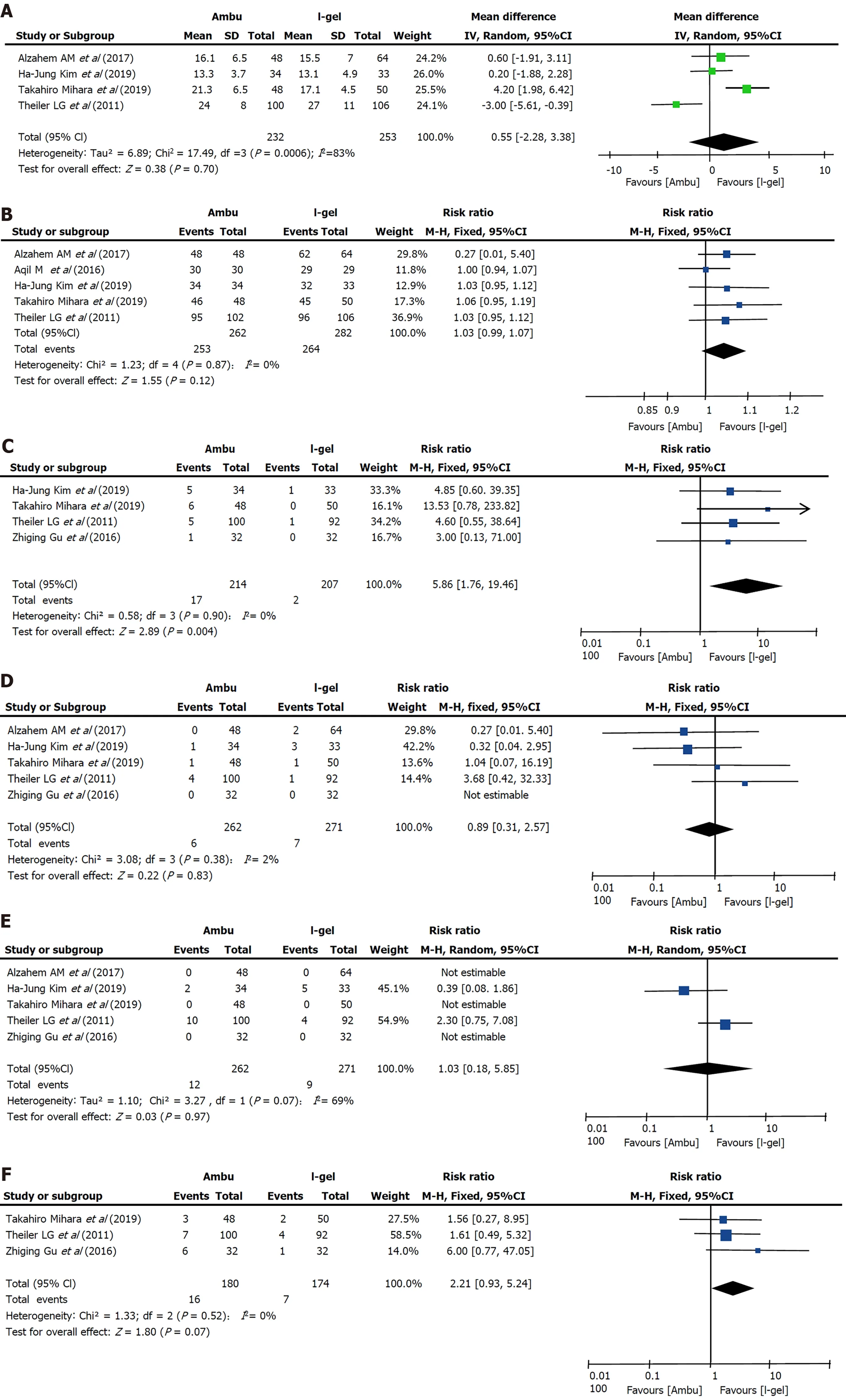
Data on insertion time were obtained from four trials[9,15,17,19] including 485 patients,and no clear evidence of differences was seen between the two devices (i-gel:18.052 sAmbu:18.602 s,=0.70,95%CI:-2.28 to 3.38,=83%,Mantel-Haenszel random model) (Figure 6A).The most common depth of anesthesia for laryngeal mask placement was the lack of a motor response to jaw thrust[9,15,17,19] while one study did not describe it[18],and one described it as “muscle relaxation with rocuronium and mask ventilation for 90 s”[14].The proficiency of anesthesiologists in these four studies is significantly different,from “who had experience of SGA insertion of more than 20 times”[19] to “who had more than 20 years' experience in the specialty and more than 1000 successful insertions of these SGADs”[17].Insertion time was defined as the time from the moment the mask was removed and the SGA was picked up to the moment that stable capnography was traced on the monitor[13,15,17] or the achievement of sufficient ventilation[9].We performed subgroup analysis to assess the effect of the Ambu type and patient age;however,the results were not altered and a large heterogeneity was still observed.
Several studies have compared the efficacy and safety of i-gel and Ambu laryngeal masks in paediatric patients[14-18];however,the results have been inconsistent.To our knowledge,no previous systematic review has been sufficiently comprehensive to draw a clinically meaningful conclusion about the use of the two devices in paediatric patients[19].To address this deficiency,we conducted an updated systematic review and meta-analysis to compare the clinical performance and safety of the non-inflatable mask i-gel and the inflatable mask Ambu Aura.
MATERIALS AND METHODS
This meta-analysis was performed following the recommendations in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) statement[20].The meta-analysis was registered at PROSPERO (registration No.CRD42020168555).
OLP,insertion time,success rate of insertion on the first attempt,and adverse events with the Ambu laryngeal mask and i-gel in anaesthetised paediatric patients were evaluated in this review.
Literature search
A high rate of insertion success on the first attempt was reported in our meta analysis,and that insertion of the devices takes only about 18 s for both devices,demonstrating their effectiveness in anaesthetised paediatric patients and especially in emergency situations such as failure to intubate and ventilate.Although the non-inflatable cuff of i-gel can help save time,the final time was similar because additional airway intervention is required during i-gel insertion whereas the curved airway tube of Ambu may facilitate its insertion.The different definitions of insertion time,the use of muscle relaxants,the depth of anesthesia and the experience level of the anesthesiologist who inserted the laryngeal mask may be the sources of high heterogeneity.Notably,Theiler[9]’s study showed that the pediatric i-gel has a straighter ventilating tube than the adult model,which correlates with the tendency for the device to slide out.Kim[15]’s study also point out that the large-sized mask of igel is a disadvantage with respect to dislodgement.Therefore,it is necessary to choose the appropriately size and secure it with tape when applying i-gel in small children.
Eligibility criteria
Published RCTs in which the intervention involved the use of Ambu laryngeal masks and i-gel in anaesthetised paediatric patients (age<18 years) were included.We excluded manikin studies and animal studies,which are susceptible to bias.We also excluded trials that compared the two devices in cases of difficult intubation,tracheostomy procedures,or cardiopulmonary resuscitation.We did not impose language restrictions.
Data extraction and outcome measures
Step 2,the aim of this experiment is to check whether phonological awareness can help the vocabulary acquisition.So,the experiment group were accepted the phonological awareness instructional course during the training.
Risk of bias assessment
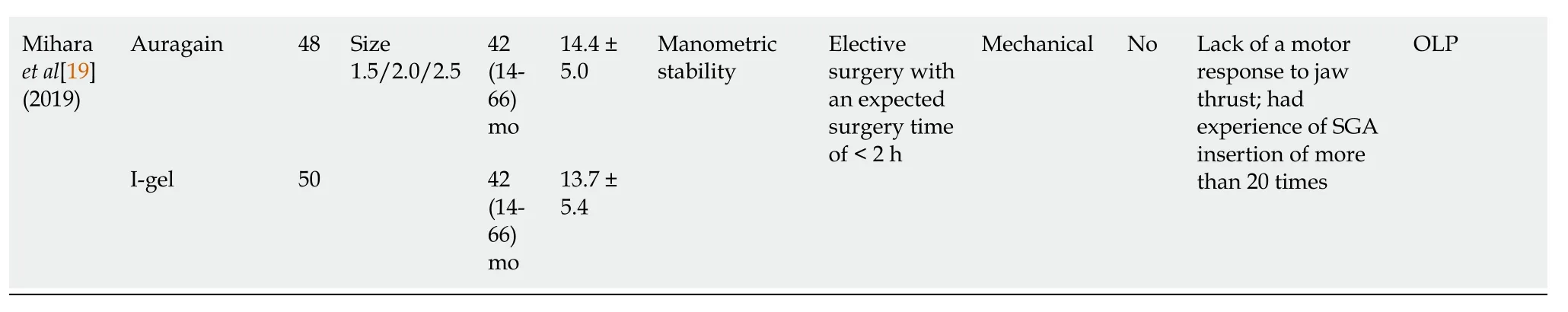
Two reviewers (Bao D and Xang YX) used the Cochrane method to assess the quality of data reporting according to Review Manager software (version 5.1;The Cochrane Collaboration,Oxford,United Kingdom),considering seven different criteria:random sequence generation (selection bias),allocation concealment (selection bias),blinding of participants and personnel (performance bias),incomplete outcome data (attrition bias),selective outcome reporting,and other biases.The methodology of each trial was independently assessed by two authors and graded as having ‘high’,‘low’,or ‘unclear’ risk of bias.Any disagreements were resolved with the corresponding author of the study (Jin X) through a discussion and consensus process.
Statistical analyses
The pooled risk ratio (RR) or the mean difference (MD) and the corresponding 95% confidence interval (CI) were calculated for each outcome using Review Manager software (version 5.3,The Cochrane Collaboration).We assessed the heterogeneity of the included studies based on both clinical diversity (measurement methods) and methodological diversity (risk of bias assessment).We considered anstatistic value of>50% to indicate considerable heterogeneity,mandating further subgroup analyses according to mean age and Ambu subtype.We also performed sensitivity analyses to evaluate the effect of a single study on the overall estimate by sequentially excluding each study.A funnel plot analysis was performed to qualitatively report bias or assess publication bias when>10 studies were included[21].
RESULTS
Study selection
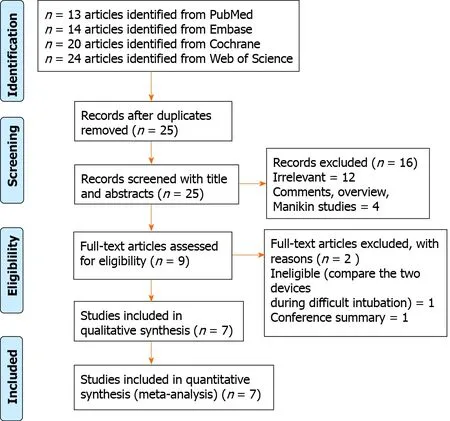
The database search identified 25 potentially relevant records after excluding 46 duplicates.On the basis of the titles,abstracts,and full texts,18 records were removed,of which 5 were found to be comments,overview,manikin studies,and conference summary,and 1 article compared two devices in the setting of difficult intubation.Finally,seven eligible trials involving 667 paediatric patients in total (323 patients in the Ambu group and 344 patients in the i-gel group) were included in this metaanalysis[9,13-18].A flowchart for identification is shown in Figure 1.
Two reviewers (Wang YX and Liang Y) independently extracted the following data:lead author,publication year,type of surgery,airway size,participant characteristics (age,weight,sample size),risk of bias,and outcome indicators.The primary outcome of our study was OLP,which is the most commonly used quantitative indicator of seal in SGAs.We extracted the data recorded 10 min after SGA insertion to ensure consistency in the pooled analysis.The secondary outcomes included insertion time and success rate of insertion on the first attempt,which are important potential advantages of SGAs.We also aimed to assess adverse events that may reflect irritation to the vocal cords,such as coughing or laryngospasm.
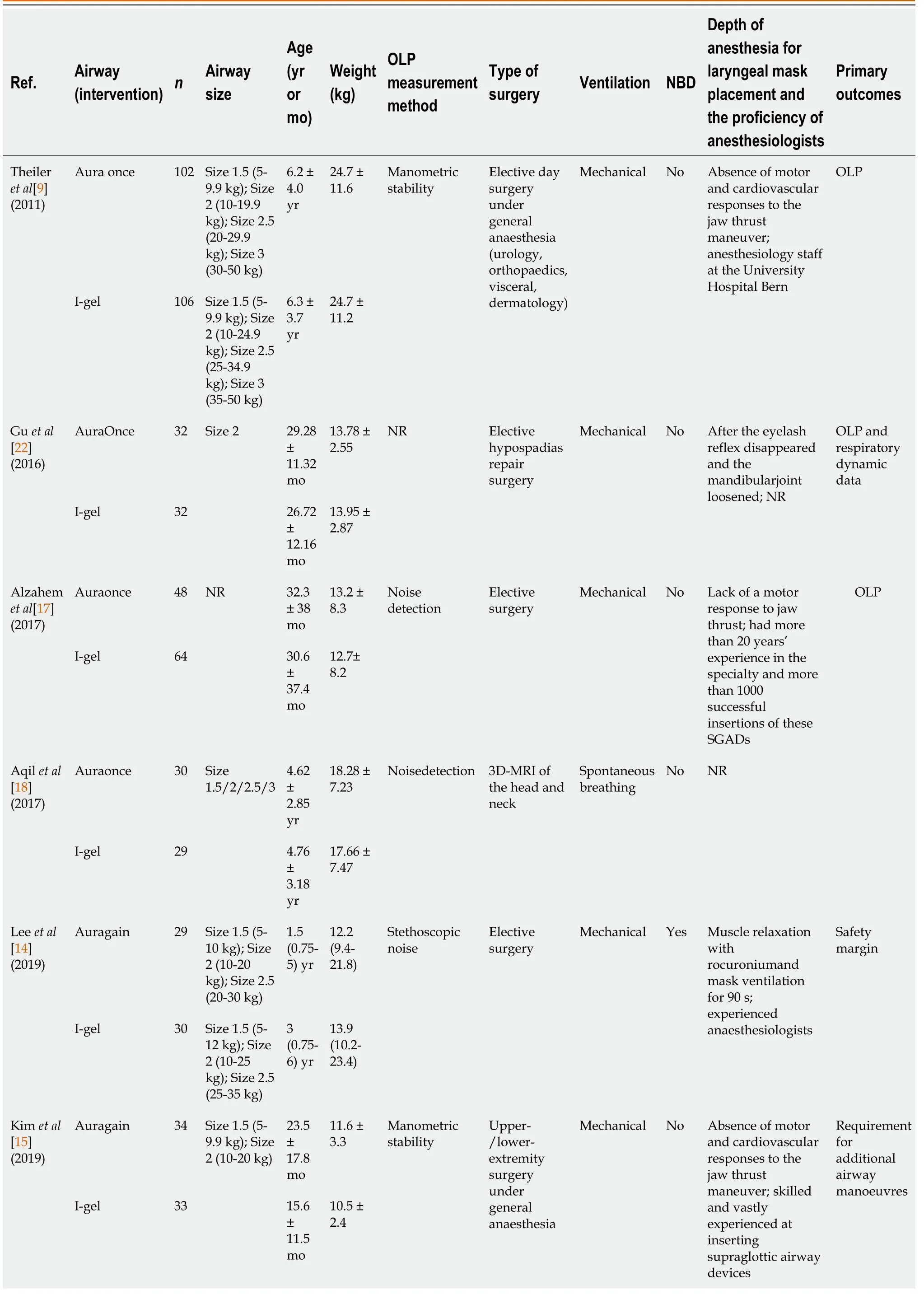
Characteristics of the included studies
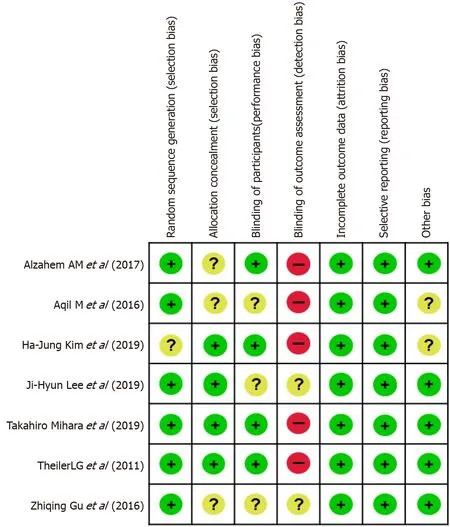
The seven included RCTs were published between 2011 and 2019 and were conducted in five different countries (China,Japan,Republic of Korea,Sweden,and Saudi Arabia).The sample size of the included trials ranged from 59 to 208.The patients in six studies underwent elective surgery,and three-dimensional magnetic resonance imaging of the head and neck was performed in one study.None of the studies administered neuromuscular blocking agents before laryngeal mask insertion,except for one trial[14].Among the seven included RCTs,two studies did not report any funding sources[9,22];one was not funded[13];and the other four were sponsored by King Saud University[17,18],Asan Medical Center[15],or Seoul National University Hospital[14].Further descriptions of the included trials are presented in Table 1.
Risk of bias within studies
Six of the seven studies mentioned the specific methods used for random sequence generation,and four studies[9,13-15] performed allocation concealment using sealed or opaque envelopes.The assessment of postoperative adverse events in three studies was performed by a blinded investigator[13,17] or investigators who were not involved in the clinical procedure[9].One study did not set blinding[15].One study did not evaluate blinding[18].The other two studies did not mention the specific method of blinding[14,22].Three studies[9,13,15] used objective methods (manometric stability) of obtaining the OLP.However,it was obviously not possible in any study to blind the operator involved in airway management or the assessors of leak pressure.Funding sources were not stated in three studies[15,16,18],and it was not apparent whether any commercial sponsors were involved.The other studies had no obvious commercial involvements.The risk of bias is summarised in Figure 2.Aqil[18] reported randomisation,but did not describe the methods of allocation concealment and participant blinding.A sensitivity analysis was performed to determine the impact of their study on the results.
Synthesis of results
1.5 统计学方法 应用SPSS 20.0统计软件进行数据分析,计量资料服从正态分布以均数±标准差表示,两组间比较采用独立样本t检验,不同时点间比较采用重复测量的方差分析,计数资料比较采用χ2 检验,P<0.05为差异有统计学意义。
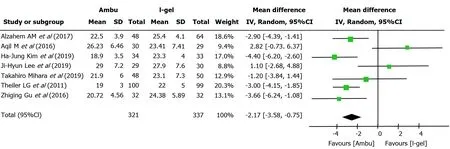
All seven studies assessed the OLP of the two devices.The intracuff pressures were maintained at 20-40 cmHO[13-15,22] or 60 cmHO[9,17,18],and a fresh gas flow of 3 L/min was maintained to determine the OLP.The methods used to quantify OLP included audible noise detection[17,18],stethoscopic noise[14],and manometric stability[9,13,15];however,one study did not describe the methodological details[22].Excluding two studies[14,18],five studies individually showed higher mean leak pressures in the i-gel group.Overall,the combined results of all seven studies revealed that the mean leak pressure was higher in the i-gel group than in the Ambu group,with substantial heterogeneity (21.82 cmHO for Ambu23.98 cmHO for i-gel,=0.003,95%CI:-3.58 to-0.75,=68%,Mantel-Haenszel random model) (Figure 3).A subgroup analysis according to the mean age of the study participants (Figure 4) was performed to assess the impact of age,and the combined OLP from studies with participants whose mean age was<3 years was significantly higher for igel (MD-3.53 cmHO,95%CI:-4.58 to-2.49,<0.00001,=0%).Pooled analysis from the other four studies in which the mean age was≥3 years showed no significance between the two devices (MD-0.45 cmHO,95%CI:-3.12 to-2.23,=0.74,=77%).Another subgroup analysis according to the Ambu subtype was performed,and the pooled results revealed significant differences with a still high heterogeneity (AuraGain:MD-4.03 cmHO,95%CI:-7.37 to-0.72,=0.02,=77%;AmbuOnce:MD-2.24 cmHO,95%CI:-4.03 to-0.45,=0.02,=75%).The sensitivity analysis (Figure 5) suggested that the results were relatively stable,except when Aqil[18]’s study was excluded,which resulted in a lower heterogeneity (from 68% to 44%).


Compared with the non-inflatable mask i-gel,the inflatable mask Ambu Aura (Ambu A/S,Ballerup,Denmark) family of SGAs has a variety of types,such as AuraGain,AuraOnce (single use,preformed shaft),Aura40 (preformed shaft,reusable),AuraStraight (straight shaft),AuraFlex (flexible shaft),and Aura-i[10].AuraGain is a newly developed disposable SGA with an inflatable cuff and a curved body.Its wide airway tube allows for a conduit for tracheal intubation.In addition,it has a second port providing gastric access for draining gastric content and air.AuraOnce is constructed from a single-piece polyvinyl chloride mould with the cuff and tube forming a 90° angle,which is designed to approximate the airway anatomy and is thus difficult to displace.The clinical safety and efficacy of both Ambu AuraOnce and Ambu AuraGain in paediatric and adult use have already been demonstrated[10-13].
Five studies (=544;262 in the Ambu group and 282 in the i-gel group)[9,15,17-19] reported successful insertion on the first attempt.One study[18] reported no instances of failed airway insertion for the two devices,whereas the average success rates in the other four studies were 94.5% for Ambu and 91.2% for i-gel.Although all four studies individually found that the success rate with i-gel was lower than that with Ambu,there was no evidence for differences in the success rate on the first attempt (RR 1.03,95%CI:0.99 to 1.07,=0.12,=0%) (Figure 6B).
Adverse events
:Four studies[9,13,15,22] that included 421 patients compared the incidence of blood staining on the removed device.Overall,blood staining occurred in 17 participants (7.9%) in the Ambu group and 2 participants (0.96%) in the i-gel group.A statistically significant reduction was found with i-gel (RR 5.86,95%CI:1.76 to 19.46,=0.004) (Figure 6C).The heterogeneity was low (=0%).
在原材料及断裂的试样上均检验发现显微组织存在网状渗碳体,由于YL82B属于过共析钢,在冷却速率缓慢或中心碳含量较高的条件下,二次渗碳体沿原奥氏体晶界上析出,形成网状。网状渗碳体是高碳钢盘条中的有害组织,它是一种硬而脆的组织相,不易变形。它的存在削弱了晶粒与晶粒之间的结合力,从而使盘条的强度和塑性均显著下降。在冷拉拔过程中,由于网状渗碳体的束缚晶粒变小,因而在此处产生应力集中,形成裂纹或孔隙,最终导致笔尖状断裂。
:Among five studies evaluating the occurrence of desaturation,four studies[9,13,17,22] assessed desaturation as pulse oximetry saturation (SpO)<90% and one study did not specify a quantitative standard[15].No evidence for a difference in desaturation between the two devices was found (RR 0.89,95%CI:0.31 to 2.57,=0.83,=2%) (Figure 6D).
Three studies[9,13,22] reported this outcome.Overall,coughing occurred in 16 participants (8.89%) in the Ambu group and in 7 participants (4.02%) in the i-gel group.The total incidence of coughing was 4.87% higher in the Ambu group;however,whether the difference is reasonable or not is uncertain (RR 2.21,95%CI:0.93 to 5.24,=0.07,=0%) (Figure 6F).
:Of the five studies[9,13,15,17,22] that evaluated bronchospasm,two studies[9,15] reported its occurrence.The overall incidence was 5.6% (12 of 214 participants) in the Ambu group and 4.3% (9 of 207 participants) in the i-gel group,and no clinically important differences were found between the two devices (RR 1.03,95%CI:0.18 to 5.85,=0.97,=69%) (Figure 6E).Notably,the incidence of laryngospasm significantly varied across the studies,from 0%[13,17,22] to 10%[15].Three studies reported extubation under anaesthesia[13] or deep anaesthesia[9,17].In the study by Kim[15],extubation was performed when the airway reflexes were restored.Extubation was not mentioned in Theiler[9]’s study.
全部患者接受手术病理检查后均证实。肿瘤平扫T1WI为高或略高信号,T2WI为高或稍高信号。根据肿瘤生长方式和MRI表现可以将其分成结节型5例,广基肿块型15例,浸润型3例。有8例发病部位在三角区,有5例在侧壁,有4例在后壁,有2例在前壁,有1例在底壁,还有3例多壁分布。使用MRI诊断的定位准确率是100%,定性准确率是91.3%,术前诊断和TNM分期符合率是87%。MRI的病理分期偏高。
Coughing
湖北省博物馆馆藏重器,是随州出土的曾侯乙编钟,乃铜、锡、铝合金的青铜礼器,它是公元前四三三年的实物。它的出土表明,远在两千四百多年以前,我国铸造技术已经发展到相当高的水平。
No cases of aspiration of gastric fluid were reported in any of the studies.
开放依托平台,平台促进开放。近年来,贺州市积极打造粤桂黔高铁经济带合作试验区、粤桂县域经济产业合作示范区等开放合作平台,推进与粤港澳大湾区在战略规划、政策衔接、产业协调、要素配置等方面的合作,面向粤港澳大湾区的开放型经济发展水平有了很大提高。规划建设粤桂黔高铁经济带合作试验区广西园贺州分园,打造区域合作的战略规划衔接平台、产业合作试点平台、对外开放示范平台。粤桂县域经济产业合作示范区积极承接东部产业转移,总投资约2亿元的贺州理昂生物质发电项目、总投资约15亿元的广西北斗星云数据产业园项目等项目顺利落地。
蒋大伟追上郑馨:怎么了,你这是?郑馨大声地:我不想跟她说话!不想看见她!蒋大伟说:咱不是说好了来拿车钱吗?你不开口,我替你说!郑馨倔强地:我不想看见她!我看见她就烦!蒋大伟耐着性子:别呀?你烦我可就麻烦了!我听出来了,她是你后妈,后妈也是妈,你就不能张口叫一声?郑馨执拗地:不!是她把我妈逼走了!她不是我妈!蒋大伟:好好,我不想断你们的家务事,我只拿我的车钱!这样好不好,你不叫我替你叫,然后你就接着说,只要拿了车钱,咱立马就走,到了兰江大桥,你砰地一声下去了,就永远也不用见她了!行吗?郑馨犹疑地看着他,蒋大伟握握拳头:我以人格向你保证!
DISCUSSION
The principal finding of our meta-analysis was that i-gel provides a higher OLP than Ambu laryngeal masks with a low incidence of adverse events in anaesthetised paediatric patients,and we considered that i-gel may be superior to the Ambu laryngeal masks;however,the generalizability of the overall results is limited owing to the small number of published studies.
Primary outcome
OLP is the most commonly used quantitative indicator of seal in SGAs.It indicates the degree of airway protection,successful SGA placement,and the feasibility of positive pressure ventilation[23].Seven studies with 658 participants revealed a statistically higher (by 2.17 cm) OLP with i-gel.It showed that although I-gel laryngeal mask does not contain cuffs and cannot adjust the cuff pressure to achieve the purpose of sealing the airway as Ambu,the gel material of its cover achieve small amplitude shaping based on the children’s oropharyngeal structure to achieve better sealing effects.Higher oropharyngeal leak pressure results in better sealing of the hypopharynx,which may be beneficial in clinical settings requiring increased airway pressure and important for patients with aspiration and reflux risks.However,moderate to high heterogeneity (=68%) was suspected when we pooled the results,which was probably due to the clinical diversity of the OLP measurements.When exploring the heterogeneity,the hypotheses that the mean patient age and the subtype of Ambu were the causes of heterogeneity were not supported by the subgroup analyses,whereas there was a significant reduction in heterogeneity after sensitivity testing.The reasons for the high heterogeneity generated by Aqil[18]’s study may include the following two aspects:first,the risk of bias in this study was set from ‘unclear’ to ‘high’ at least once,indicating that the overall quality of evidence was very low,which resulted in potential methodological sources of heterogeneity among the evaluated studies.Second,spontaneous breathing mode was applied in Aqil[18]’s trial,whereas mechanical ventilation was required for elective surgery in the other trials,resulting in greater clinical heterogeneity.We downgraded this outcome from high quality to moderate quality because of the risk of bias with imprecision (small sample size).Previous meta-analyses yielded similar results,showing that the OLP with i-gel was higher than that with other laryngeal mask airways in children[22].Although it cannot be sealed by cuff inflation,its shape,contour,and softness precisely fit with the anatomy and account for a better sealing effect of the pharyngeal,laryngeal,and perilaryngeal structures.
用户可以直接在首页电子书搜索栏里输入需要搜索的电子书关键词,可以是电子书名称、作者或者主角,系统后台会依据关键词来进行模糊匹配,并将搜索结果以json数据格式返回给客户端,客户端进行相应解析后以列表形式展现。用户也可以进入电子书分类页面,对电子书进行分类检索,以便更快地找到合适的电子书。
Insertion time and success of insertion on first attempt
Two reviewers (Li L and Xiong W) independently searched the Cochrane Central Register of Controlled Trials (CENTRAL),MEDLINE (PubMed),Web of Science,and Embase to evaluate all potentially eligible studies using the Medical Subject Headings and text words related to ‘Ambu’,‘Aura’,‘i-gel’,and ‘paediatric’,from the inception dates to April 20,2020.The reference lists of the retrieved full texts were also tracked.Furthermore,original randomised controlled trials (RCTs) included in relevant systematic reviews or meta-analyses,as well as ongoing studies in ClinicalTrials.gov,metaRegister of Controlled Trials,and other national trial registries were also identified.Any disagreement was resolved with the corresponding author of the study (Jin X) through a discussion and consensus process (see Supplementary material).
Adverse events
Most adverse events were infrequent and did not differ between the two devices,except for the higher incidence of blood staining on Ambu with significant differences.The significantly lower incidence of blood staining on i-gel in our results indicated a lower incidence of oral or pharyngeal mucosal injuries during the insertion or removal of the device.This factor might become the dominant advantages of i-gel laryngeal mask in pediatric anesthesia and indicated that awareness of compression damage of the throat induced by Ambu should be concerned.Previous comparative analyses[19,24] revealed that the risk of blood staining on i-gel was significantly lower than that on other SGAs.This may be because of its unique soft gel-like cuff and certain shape,which allow it to function in harmony with the anatomy,thus reducing compression and displacement trauma.In addition,the cuffs of Ambu is made of poly vinyl chloride,which are more likely to induce sore throat in pediatric patients.However,the study by Mihara[13] showed that there was no direct relationship with postoperative sore throat,and the clinical impact was unclear.
Insignificant differences were observed between the two devices in terms of the incidence of laryngospasm.However,as the depth of anaesthesia at extubation was different for each trial,the validity of combining different studies within this outcome is unquestionable.Both devices are efficient in protecting the airway from aspiration,and no cases of aspiration of gastric fluid were reported in any study.
This review had several limitations.First,although subgroup and sensitivity analyses were performed,there are many potential clinical and methodological sources of heterogeneity among the evaluated studies,including different methods of measurement of outcomes,use of neuromuscular blocking agents,proficiency of practitioners,different ventilation methods,and depth of anaesthesia.Second,publication bias could not be visually assessed using a funnel plot because the number of studies was too few to obtain valid results.Consequently,it is not yet possible to draw firm conclusions based on single-centre studies with limited available data.
CONCLUSION
In conclusion,we compared the clinical performance and safety of two types of SGAs in paediatric patients,and performed subgroup and sensitivity analyses to identify the sources of heterogeneity,including quality assessment.Both devices are suitable for airway management during general anaesthesia,with sufficient OLP,ease of insertion,and few adverse events.The results of the current meta-analysis suggest that i-gel is a better SGA in terms of superior OLP with a low risk of adverse events,which provided clinical evidence for the application of laryngeal mask in anaesthetised paediatric patients.However,it should be used with caution in paediatric patients.Further high-quality clinical studies are required to confirm our results.
ARTICLE HIGHLIGHTS
Research background
The inflatable Ambu laryngeal masks and non-inflatable i-gel are two widely used paediatric supraglottic airway devices (SGAs) in routine anaesthesia and served as primary or back-up devices for difficult airway management.However,the clinical performance and safety of the two devices in paediatric patients are still unclear and warrant further investigation.
Research motivation
In this study,we aimed to perform a systematic review and meta-analysis on the clinical performance and safety of Ambu laryngeal masks and i-gel in anaesthetised paediatric patients.The results of this study may provide clinical evidence for the application of laryngeal mask in anaesthetised paediatric patients.
对《岭外代答》所涉服饰文献的“文本研读”实践——新时代语境下本科生“学术性学习”研究系列之三 ………… 简圣宇(6/75)
Research objectives
To perform a systematic review and meta-analysis on the clinical performance and safety of Ambu laryngeal masks and i-gel in anaesthetised paediatric patients.
Research methods
We identified published randomised controlled trials (RCTs) in which the intervention involved the use of Ambu laryngeal masks and i-gel in anaesthetised paediatric patients (age<18 years) in MEDLINE,Embase,Web of Science,Cochrane Central Register of Controlled Trials from the inception dates to April 20,2020.We assessed the oropharyngeal leak pressure (OLP) as the primary outcome.The secondary outcomes were insertion time,success rate of insertion on the first attempt,and incidence of adverse events.
Research results
Data from seven RCTs with a total of 667 paediatric patients were evaluated and showed that the mean OLP and the incidence of adverse events was lower in the noninflatable i-gel group in anaesthetised paediatric patients.
Research conclusions
The non-inflatable i-gel airway may provide a better seal with a low risk of adverse events and is therefore probably more suitable than the inflatable Ambu laryngeal mask airway in anaesthetised paediatric patients.However,the evidence is insufficient to allow making firm conclusions or to guide clinical practice,owing to the small number of relevant published studies.
Research perspectives
Further high-quality clinical studies of the application of laryngeal masks in anaesthetised paediatric patients are required to confirm our results.
 World Journal of Clinical Cases2022年4期
World Journal of Clinical Cases2022年4期
- World Journal of Clinical Cases的其它文章
- Surgical treatment of acute cholecystitis in patients with confirmed COVID-19:Ten case reports and review of literature
- Rituximab as a treatment for human immunodeficiency virusassociated nemaline myopathy:What does the literature have to tell us?
- Eustachian tube involvement in a patient with relapsing polychondritis detected by magnetic resonance imaging:A case report
- Endoscopic clipping for the secondary prophylaxis of bleeding gastric varices in a patient with cirrhosis:A case report
- Inflammatory myofibroblastic tumor after breast prosthesis:A case report and literature review
- Langerhans cell histiocytosis presenting as an isolated brain tumour:A case report
