Heart failure in COVlD-19 patients:Critical care experience
Kevin John John,Ajay K Mishra,Chidambaram Ramasamy,Anu A George,Vijairam Selvaraj,Amos Lal
Kevin John John,Department of Critical Care,Believers Church Medical College Hospital,Thiruvalla 689103,India
Ajay K Mishra,Chidambaram Ramasamy,Anu A George,Department of Internal Medicine,Division of Cardiovascular Medicine,Saint Vincent Hospital,Worcester,MA 01608,United States
Vijairam Selvaraj,Division of Medicine,The Miriam Hospital and Warren Alpert Medical School of Brown University,Providence,RI 02906,United States
Amos Lal,Department of Medicine,Division of Pulmonary and Critical Care medicine,Mayo Clinic,Rochester,MN 55902,United States
Abstract Patients with heart failure(HF)may be at a higher risk of coronavirus disease 2019(COVID-19)infection and may have a worse outcome due to their comorbid conditions and advanced age.In this narrative review,we aim to study the interaction between COVID-19 and HF from a critical care perspective.We performed a systematic search for studies that reported HF and critical carerelated outcomes in COVID-19 patients in the PubMed and Medline databases.From a total of 1050 papers,we identified 26 that satisfied the eligibility criteria for our review.Data such as patient demographics,HF,intensive care unit(ICU)admission,management,and outcome were extracted from these studies and analyzed.We reported outcomes in heart-transplant patients with COVID-19 separately.In hospitalized patients with COVID-19,the prevalence of HF varied between 4% and 21%.The requirement for ICU admission was between 8% and 33%.HF patients with COVID-19 had an overall mortality rate between 20% and 40%.We identified that HF is an independent predictor of mortality in hospitalized COVID-19 patients,and patients with HF were more likely to require ventilation,ICU admission and develop complications.Patients with HF with reduced ejection fraction did worse than those with HF with midrange ejection fraction,and HF with preserved ejection fraction.COVID-19 patients with HF should be identified early and managed aggressively in an attempt to improve outcomes in this cohort of patients.
Key Words:Heart failure;COVID-19;Critical care;Intensive care;Mortality
lNTRODUCTlON
Coronavirus disease 2019(COVID-19)emerged from China in December of 2019 and continues to be a public health emergency of international concern.As of March 12,2021,more than 118 million cases have been diagnosed worldwide with 29.3 million patients reported from the United States.Patients with pre-existing comorbidities,cardiac dysfunction and immunocompromised status continue to be at high risk of morbidity and mortality.The literature on COVID-19 infection in patients with heart failure(HF)is limited.Patients with HF may be at higher risk of COVID-19 infection and have a worse outcome due to their comorbid conditions and advanced age.
The currently available literature regarding the role of critical care and a multidisciplinary approach in treating patients with HF and COVID-19 infection,remains scarce.In this narrative review,we aim to study the interaction between COVID-19 and HF from a critical care perspective.We also aim to explore the various outcomes as reported in the literature in this subgroup of patients and to provide a summary of the current evidence and practices in the management of HF in COVID-19 patients in the intensive care unit(ICU).
In this review,we have attempted to summarize all the articles published on the presentation and management of patients with COVID-19 and HF.We searched the PubMed and Medline database for the MeSH terms “COVID-19”,“heart failure" and”critical care”.Studies published in English,including adults with HF and COVID-19 infection were eligible to be included in this review(Figure 1).All studies published before March 2021 were included.Studies that provided details on patient demographics,HF,ICU admission,management,and outcome were analyzed.Various treatment details including medications such as beta blockers,angiotensin converting enzyme inhibitors(ACEi),aldosterone receptor blockers(ARB),angiotensin receptor-neprilysin inhibitors(ARNi),automatic implantable cardioverterdefibrillator,permanent pace-maker and cardiac resynchronization therapy were included.Critical care details that were obtained were the type of organ dysfunction,the requirement of non-invasive and invasive ventilation,administration of vasopressor support,extra-corporeal membrane oxygenation(ECMO)and outcome.Articles that did not have the patient’s details,opinions,comments,letters,and articles not published in English were excluded from the analysis.Studies that included cardiac transplant patients were analyzed separately.Two independent clinicians reviewed all articles.
As of March 2021,a total of 1050 papers were identified(Figure 1).Among these,26 satisfied the eligibility criteria for our study.One study was a prospective cohort study,while all others were retrospective studies.Studies were principally published from North American and European nations.There were significant differences in the study design,data collection and measured outcomes among the studies which made the comparison of data difficult.Therefore,we divided the studies into four categories and reported the outcomes separately.The four categories were:(1)Studies highlighting prevalence of HF,requirement of ICU level of care and outcomes in hospitalized COVID-19 patients;(2)Studies reporting outcomes in COVID-19 patients admitted to ICU;(3)Studies reporting outcomes in HF patients with COVID-19;and(4)Studies reporting outcomes in heart-transplant patients with COVID-19(Figure 2).
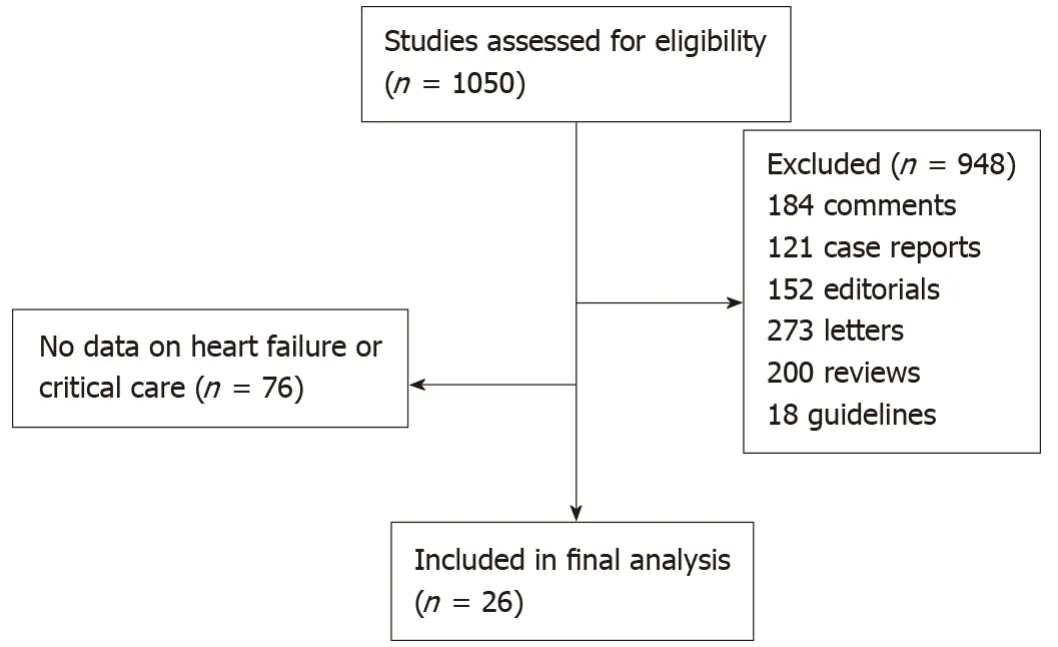
Figure 1 CONSORT diagram.
Figure 2 Coronavirus disease 2019 and heart failure.
lNCREASED RlSK OF HEART FAlLURE lN COVlD-19 PATlENTS
Among studies that reported outcomes in hospitalized patients with COVID-19,we found 11 studies that provided data on HF and ICU admission(Table 1)[1-11].The total number of patients in this group was 9420,with studies from the United States contributing the maximum number of patents.The diagnosis of COVID-19 was uniformly established with reverse transcription polymerase chain reaction(RT-PCR)in all of the patients.The proportion of patients with pre-existing HF varied from 1%to 21%,which was almost ten times the community prevalence of HF,as reported by the Framingham study[12].This suggests that patients with HF are more likely to require hospitalization for COVID-19.Zyllaet al[3]reported that 3% of patients developed newly diagnosed(de novo)left ventricular(LV)dysfunction after admission,while Zhouet al[9]and Chenet al[10]reported a number close to 25%.This highlights the fact that HF can be both a risk factor,as well as a complication of COVID-19.Most studies reported a male preponderance with a mean age above 60 years.The requirement for ICU admission was between 8% and 33%.Patients with HF were more likely to require mechanical ventilation and develop complications such as thromboembolism,sepsis,stroke and acute kidney injury.The overall mortality rate for hospitalized patients with COVID-19 was between 4% and 40%.Inciardiet al[1]noted that chronic therapy with an ACEi,ARB,or ARNI had to be discontinued in 77% of casesbecause of severe hypotension,and patients who died were more likely to have a history of HF.In the same study,the mortality rate remained higher in patients with cardiac disease compared to those without(26%vs9%;P= 0.039),even after excluding patients who were denied intubation due to comorbidities or age.Another study used multivariate regression modelling to identify an increased risk of atrial fibrillation among COVID-19 patients with HF(RR 1.88;P= 0.023),which in-turn increased the odds of ICU or intermediate care ward admission(OR 2.37;95%CI:1.10-5.09;P= 0.03)[4,5].HF was also linked to brady-arrhythmias(OR 9.75;95%CI:1.95-48.65)by a separate group of investigators[5].Three separate meta-analysis identified that HF was independently associated with an increased risk of mortality in patients with COVID-19[13-15].
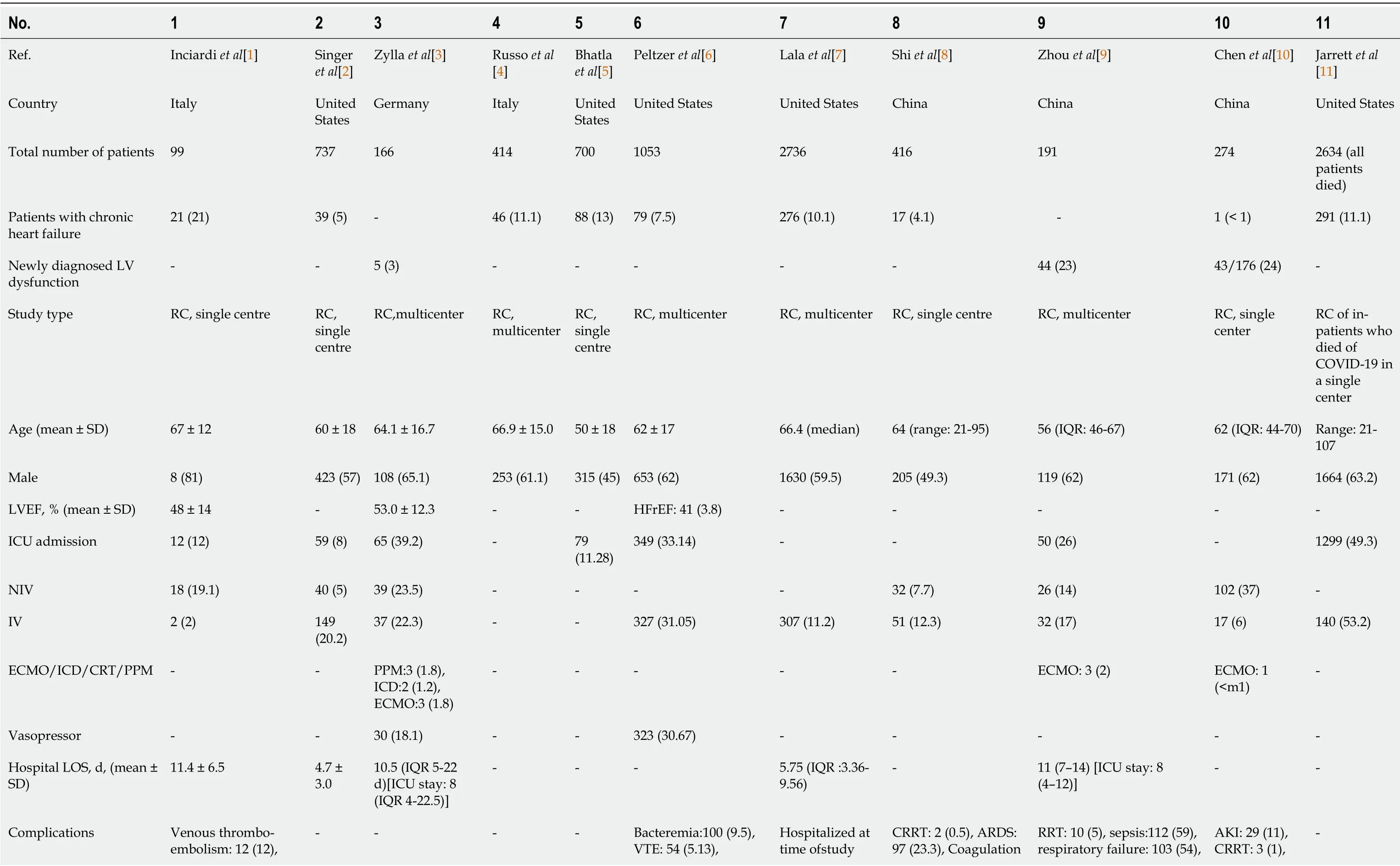
Table 1 Studies highlighting prevalence of heart failure,requirement of intensive care unit level of care and outcomes in hospitalized coronavirus disease 2019 patients,n(%)
- Signifies that the variable was not reported in the study.LV:Left ventricle;RC:Retrospective cohort;LVEF:Left ventricle ejection fraction;HFrEF:Heart failure with reduced ejection fraction;ICU:Intensive care unit;NIV:Non-invasive ventilation;IV:Invasive ventilation;ECMO:Extracorporeal membrane oxygenation;ICD:Implantable cardiovascular-defibrillator;CRT:Cardiac resynchronisation therapy;PPM:Permanent pacemaker;LOS:Length of stay;IQR:Inter-quartile range;VTE:Venous thrombo-embolism;TIA:Transient ischemic attack;AKI:Acute kidney injury;CRRT:Continuous renal replacement therapy;RRT:Renal replacement therapy;ARDS:Acute respiratory distress syndrome;ALI:Acute liver injury;DIC:Disseminated intravascular coagulation.
NEED FOR lNTENSlVE CARE UNlT LEVEL OF CARE
We found six studies that reported HF data in COVID-19 patients who were admitted to the ICU,while excluding patients who were hospitalized without requiring ICU care(Table 2)[5,16-20].These studies had a total patient number of 6539,with a major patient population contributed from the United States.The mean age in this group of patients was above 60 years and there were more men than women.Between 10% and 43% of these patients had pre-existing HF.This range was higher than what was observed among hospitalized patients overall.It was also noted that more patients developedde-novoHF in this group(up to 33%)[16].The average ICU length of stay was between 2 to 5 weeks and a majority of patients required ventilatory assistance.In addition,advanced life-sustaining supportive interventions such as ECMO were also utilized by 3% to 15% of these patients.As a group,these patients had a higher mortality rate,which was as high as 52%.A cross-sectional observational multi-centre nationwide survey in Italy identified that obesity,chronic kidney disease andhypertension in men,and obesity(OR 2.564;95%CI:1.336-4.920;P< 0.0001)and HF(OR 1.775;95%CI:1.030-3.057)in women were associated with higher rate of ICU admission[19].Similar observations were made from a single academic medical centre in New York City and Long Island which found that the strongest risk factors for critical illness besides age were HF(OR 1.9;95%CI:1.4-2.5),BMI > 40(OR 1.5;95%CI:1.0-2.2),and male sex(OR 1.5;95%CI:1.3-1.8)[17].
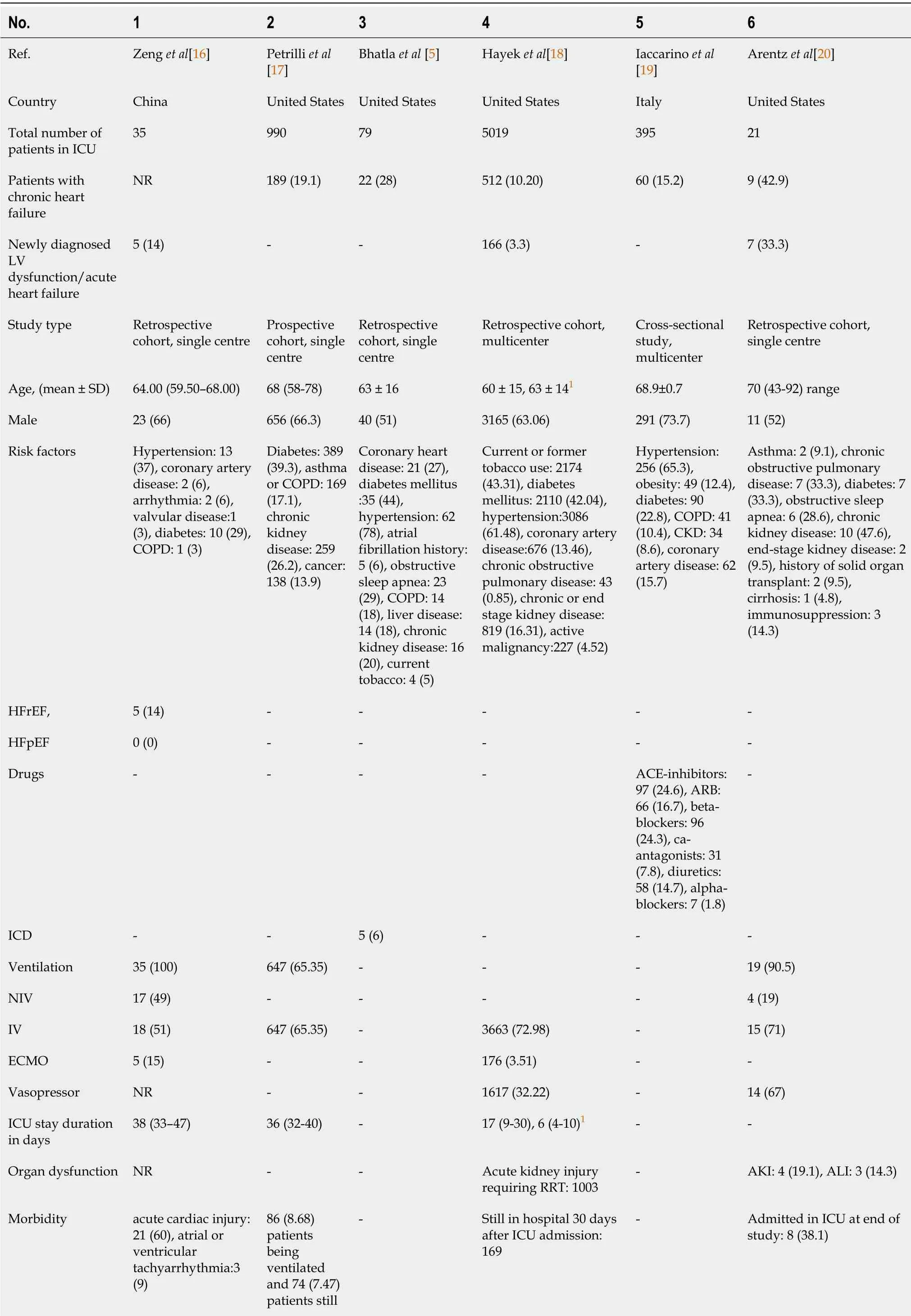
Table 2 Studies reporting outcomes in coronavirus disease 2019 patients admitted to intensive care unit,n(%)
1Baseline characteristics of patients who did not have cardiac arrest and those who had cardiac arrest respectively.- Signifies that the variable was not reported in the study.ICU:Intensive care unit;LV:Left ventricle;COPD:Chronic obstructive pulmonary disease;CKD:Chronic kidney disease;HFrEF:Heart failure with reduced ejection fraction;HFpEF:Heart failure with preserved ejection fraction;ACE:Angiotensin converting enzyme;ARB:Angiotensin receptor blocker;ICD:Implantable cardiovascular-defibrillator;NIV:Non-invasive ventilation;IV:Invasive ventilation;ECMO:Extra-corporeal membrane oxygenation;ECMO:Extra-corporeal membrane oxygenation;RRT:Renal replacement therapy;AKI:Acute kidney injury;ALI:Acute liver injury.
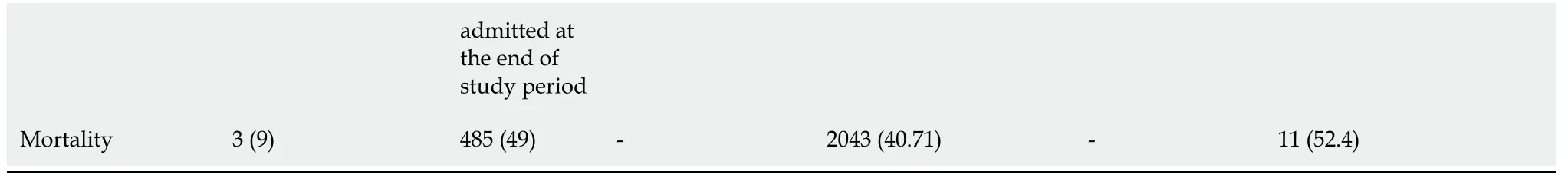
OUTCOMES lN CRlTlCALLY lLL COVlD-19 PATlENTS WlTH PREEXlSTlNG HEART FAlLURE
There were five studies(from North America and Europe)that focused on the outcomes of COVID-19 infection in patients with pre-existing HF(Table 3)[21-25].Three of them were from the United States,one was from Italy and the last one was from Denmark.Together,these studies included 9191 patients.Maximum number of patients were contributed by the study by Bhattet al[21].The mean age of patients in these studies were above 70 years,which was about 10 years higher than what was observed in the two previous groups.Two out of the five studies had more women than men.This was in contrast to the uniform male predominance observed in the two previous groups.ICU admission rates were reported by two studies and ranged between 23% and 29%.ECMO was used by three patients in one study[21].An overall mortality rate between 20% to 40% was observed.Overall mortality variation in multinational studies have ranged from close to 30 % to over 90 %.There was also a significant inter-hospital variability in the outcome of critically ill patients which could not be attributed to the location or performance of the treating facility[26].Tomasoniet al[24]reported more in-hospital complications such as acute HF(33.3%vs5.1%,P<0.001),acute renal failure(28.1%vs12.9%,P< 0.001),multiorgan failure(15.9%vs5.8%,P= 0.004)and sepsis(18.4%vs8.9%,P= 0.006)in COVID-19 patients with a prior history of HF.This suggests that patients with HF and COVID-19 have a poorer outcome than the general population.When compared to hospital admissions for other causes,HF patients admitted for COVID-19 were older,more likely to identify as Black and/or Hispanic,had higher rates of diabetes and kidney disease and used more healthcare resources such as ICU beds(29%vs15%),mechanical ventilation(17%vs6%),and central venous catheter insertion(19%vs7%;P< 0.001 for all)[21].They also had higher in-hospital mortality(24.2%vs2.6%)as well as higher skilled-nursing and rehabilitative care requirement among survivors(13%vs41%)[21].Similar conclusions were drawn by Alvarez-Garciaet al[22],who noted that the history of HF was an independent risk factor for the need for ICU care(adjusted OR 1.71;95%CI:1.25-2.34;P= 0.001),intubation and mechanical ventilation(adjusted OR 3.64;95%CI:2.56 -5.16;P< 0.001),and in-hospital mortality(adjusted OR 1.88;95%CI:1.27-2.78;P= 0.002).Furthermore,the former was the only study to look at outcomes stratified by left ventricular ejection fraction(LVEF)and found that cardiogenic shock(7.8%vs2.3%vs2%;P= 0.019)and HF-related causes for 30-day readmission(47.1%vs0%vs8.6%)were significantly higher in patients with HF with reduced ejection fraction(HFrEF)than in those with HF with midrange ejection fraction(HFmrEF)or HF with preserved ejection fraction(HFpEF)[22].Multivariate cox regression identified older age,more severe HF[baseline New York Heart Association(NYHA)functional classes III and IV],previous mitral regurgitation,lower systolic blood pressure,lower oxygen saturation,lower lymphocyte count,and increased troponin concentrations as risk factors for in-hospital mortality in COVID-19 patients with HF[22].
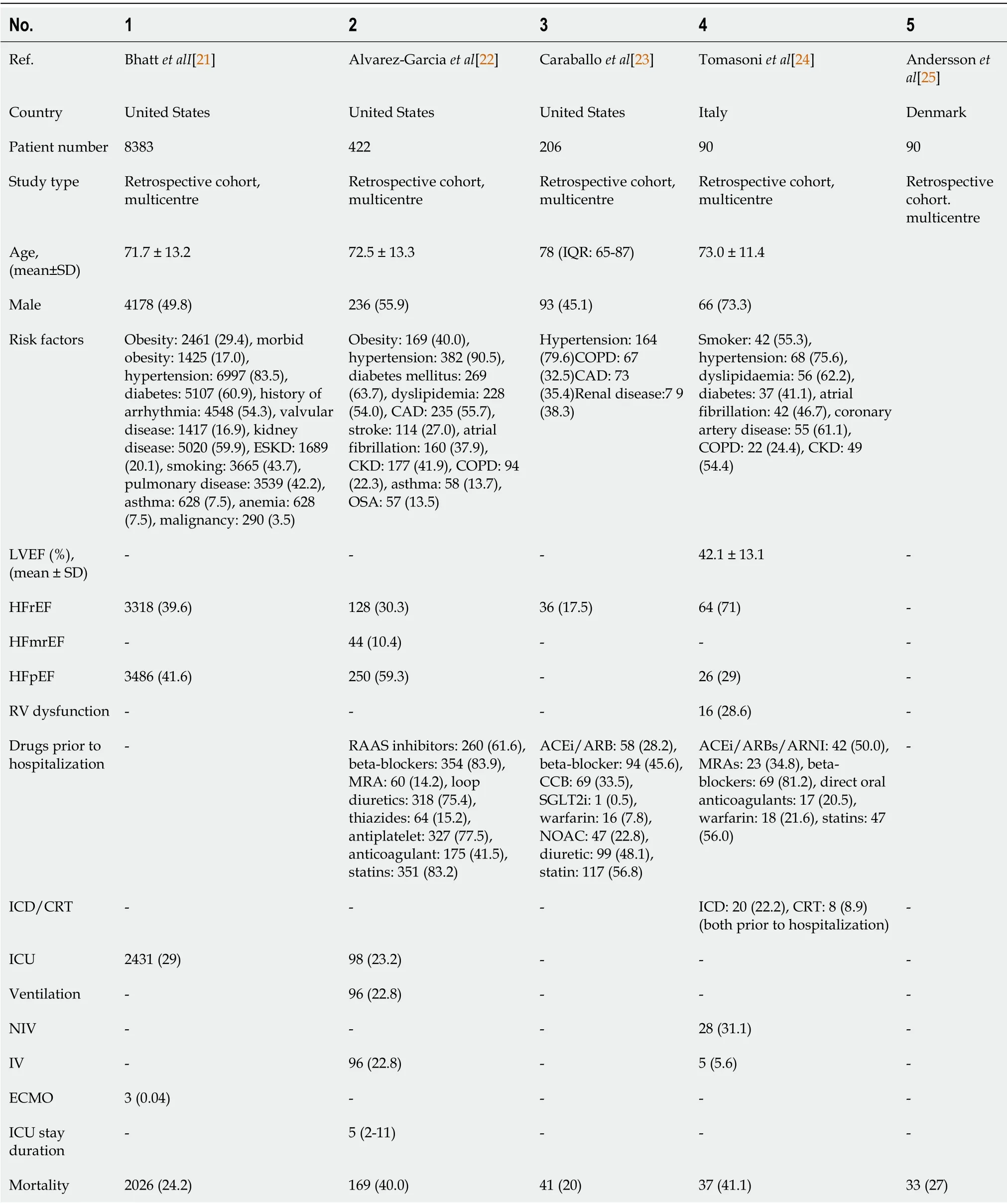
Table 3 Studies reporting outcomes in heart failure patients with coronavirus disease 2019,n(%)
DATA ON CARDlAC TRANSPLANT PATlENTS WlTH COVlD-19
We analyzed studies that included heart transplant patients separately because they are a distinct subset of patients who are likely to be on immunosuppressive therapy.We found five retrospective studies with a total of 99 patients(Table 4)[27-31].This was a group of predominantly male patients with a mean age above 55 years and a wide variation in requirements for ICU level of care;ranging from 10.5% to 100%.The patients who were admitted to ICU were sicker as evidenced by increased requirement of vasopressors,mechanical ventilation,and renal replacement therapy(83%vs38%)[28].The mortality rate was between 18% and 37%.In one study,all patients who required ICU admission died[29].This was higher than the mortality rate in the general population,but not much more than non-transplanted HF patients or patients in ICU.Bottioet al[31]reported that older age(P= 0.002),diabetes mellitus(P= 0.040),extracardiac arteriopathy(P= 0.040),previous percutaneous coronary intervention(P= 0.040),cardiac allograft vasculopathy score(P= 0.039),lower glomerular filtration rate(P= 0.004),and higher NYHA functional classes(P= 0.023)were all significantly associated with in-hospital mortality among heart-transplant patients with COVID-19[31].We know that steroids are beneficial in severe COVID-19,and cardiac transplant patients are often on multiple immunosuppressive medications that include steroids,calcineurin inhibitors and anti-metabolites[32].Whether these immunosuppressive medications protected these patients from severe disease is a question that warrants further investigation.
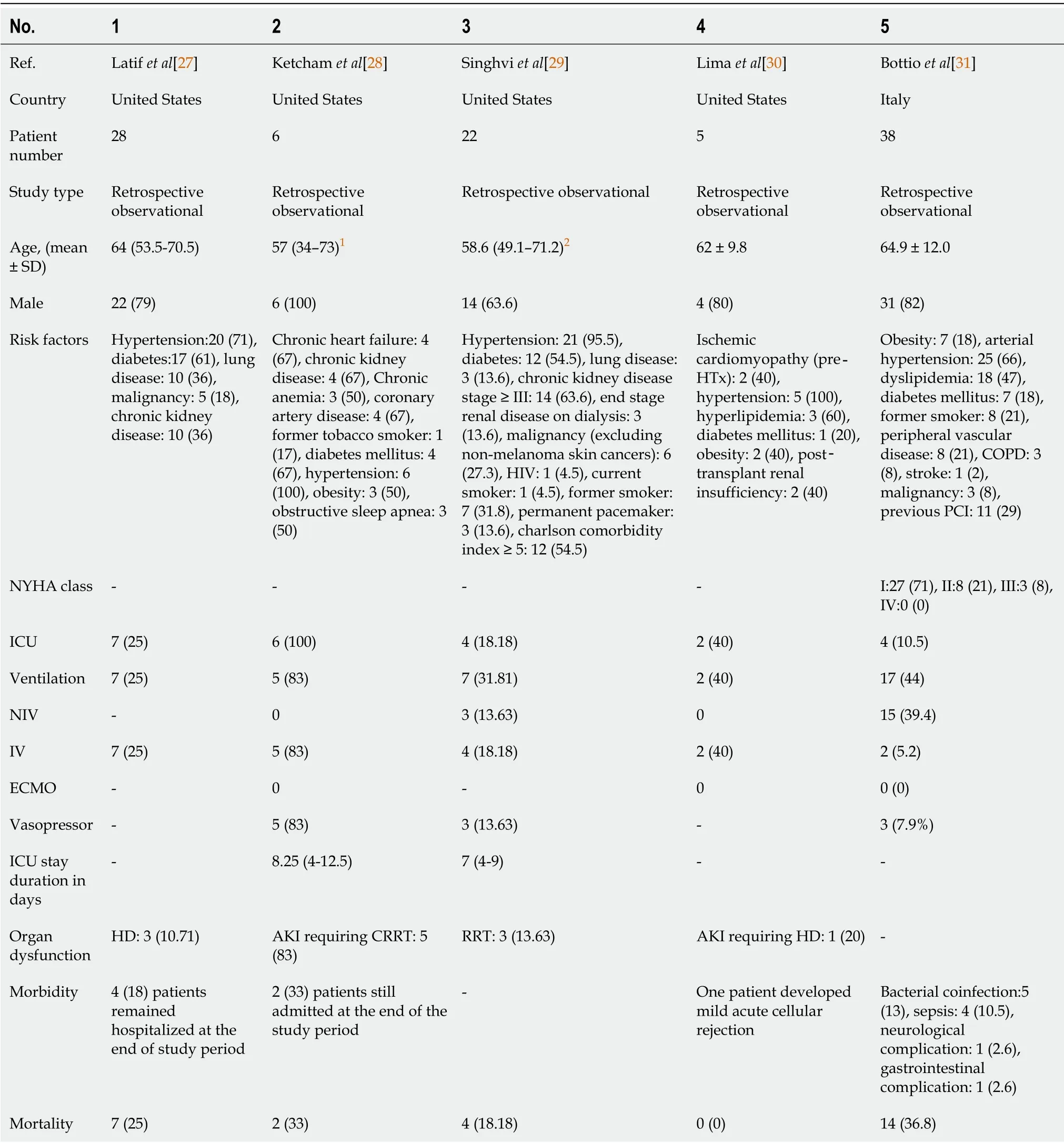
Table 4 Studies reporting outcomes in heart-transplant patients with coronavirus disease 2019,n(%)
In this review,we summarized the relationship between HF,COVID-19 and the role of intensive care in patients with COVID-19 and HF.Our review of literature revealed many interesting observations.The evidence suggests that patients with HF are more likely to be hospitalized after COVID-19 infection.Exact quantification of risk will require community-level studies and cannot be derived from the hospital-based studies included in this review.Also,patients with COVID-19 are at increased risk of developingde novoHF after admission to the hospital;a risk that increases substantially with admission to the ICU.The reversibility and long-term morbidity of COVID-19 relateddenovo HF is unclear at this point and will require future studies with longer durations of follow up.Patients with COVID-19 and HF had increased chance of requiring ICU admission,mechanical ventilation,vasopressors and renal replacement therapy.They also had more complications and a higher mortality rate when compared to non-HF patients.These differences may be due to the effect of additional organ injury and decreased physiologic reserve leading to faster decompensation.This may also be an indirect marker for variation in practices.While it is expected that patients admitted to the ICU are at increased risk for development of complications and mortality,what is interesting is that the presence of HF represents an additional independent risk factor for the same.Furthermore,due to the similarity in clinical presentation,HF in COVID-19 patients is probably underdiagnosed.Therefore,it stands to reason that the risk estimate from the studies reported thus far are lower than the true risk estimate.It was noteworthy that the outcomes in critically ill heart transplant patients with COVID-19 was not very different from critically ill non-heart transplant patients.Whether the immunosuppressive medications that heart transplant patients are on,provides them with a selective advantage in combating the‘cytokine storm’seen in COVID-19 is a question worth asking.What is clear from our analysis of the existing literature is that HF is inextricably linked with the outcomes of COVID-19 infection.What is not known is the exact mechanisms by which they are linked and therefore,this is a field with immense scope for future research.There are many reasons to study HF in COVID-19 patients.Heart-lung interactions dictate that insult to one organ,affects the other.Acute respiratory distress syndrome(ARDS)is the most common manifestation of severe COVID-19 disease.While hypoxia and positive pressure ventilation stresses the right heart,the left heart has to compensate for increased metabolic demand.These problems are compounded in patients with pre-existing HF.Therefore,it is vital that we investigate the interaction between HF and COVID-19 so that we have a better understanding of its pathophysiology,optimal management and outcome.
PATHOGENESlS OF HF lN COVlD-19
Cardiac troponins were elevated in 8%-12% of COVID-19 cases and the percentage rose up to 23%-33% in critically ill patients[1,33,34].COVID-19 is theorized to injure the myocardium indirectly and directly.The systemic inflammatory response andcytokine storm increases blood viscosity and coagulability,which causes endothelial dysfunction[35,36].The sympathetic activation,tachycardia,increased myocardial oxygen consumption and energy expenditure can also injure the myocardium.More cases of takotsubo cardiomyopathy are being diagnosed in patients with severe COVID-19[37].Elevated positive end-expiratory pressure during mechanical ventilation in COVID-19 patients with severe ARDS increases right ventricular wall stress and can further reduce the cardiac output in a failing heart[38].In a series of consecutive autopsy cases,Lindner and colleagues documented SARS-CoV-2 in 24 of
39 patients(61.5%),suggesting that direct viral myocardial damage is also possible[39].SARS-CoV-2 attaches to human cells after binding with its spikes to the ACE2,which are upregulated in patients with cardiovascular disease,diabetes,and those treated with ACEi or ARB[40-42].In light of this observation,role of ACE2 and ACEi in the pathogenesis of COVID-19 related myocardial injury has also been investigated from a therapeutic point of view.
While there are multiple factors contributing to HF in COVID-19,the incidence of true ‘myocarditis’in COVID-19 in unclear[43].Some authors estimate that myocarditis may account for up to 7% of COVID-19 deaths[44].This estimate is fundamentally flawed because the diagnosis cannot be confirmed in a vast number of cases.Also,the presentation of acute coronary syndrome,sepsis-related cardiomyopathy and takotsubo cardiomyopathy can mimic myocarditis,making this a challenging diagnosis.Myocarditis,even when subclinical,can worsen patient outcomes.In the short term,it can increase the risk of arrythmias and precipitate decompensated HF,especially in patients with pre-existing chronic HF[45].In the long term,the resultant myocardial fibrosis and negative remodeling can accelerate the decline of systolic function leading to a limitation of physical activity.Therefore,in the ICU,it is important to screen patients for subclinical myocarditis,by following the AHA recommendation of testing patients with signs consistent with myocarditis with one or more cardiac imaging methods such as echocardiogram or cardiovascular magnetic resonance[46].
SCREENlNG FOR HF lN THE lCU
Up to one-third of COVID-19 patients admitted to the ICU develop cardiomyopathy,and cohort studies from Wuhan have estimated the proportion of COVID-19 patients with cardiac injury to be between 20% and 28%[8,47].Therefore,it would be prudent to screen all COVID-19 patients admitted to the ICU for HF.Critically ill patients in the ICU,are not able to communicate their complaints,and physical examination findings are often limited.A screening algorithm such as the one suggested by the Cardiac Society of Australia and New Zealand can be employed in the ICU[48].Incorporation of such a screening algorithm into the treatment protocol will help identify more patients with HF and optimize treatment.
Although major society guidelines recommend the measurement of natriuretic peptides when the diagnosis of HF is uncertain,they should be interpreted in the context of other clinical information due to their high sensitivity and limited specificity[49,50].In addition to its diagnostic value,natriuretic peptides also have prognostic significance with higher pro-brain natriuretic peptide(pro-BNP)values associated with increased mortality[51,52].Therefore,natriuretic peptides can be used for risk stratification of COVID-19 patients with HF.Elevations in cardiac troponins have also been observed in COVID-19 patients and may indicate both coronary and noncoronary disease[53].Acute coronary syndrome,microvascular ischemia,myocarditis,takotsubo cardiomyopathy and arrythmia are some of the reasons for an elevated troponin in COVID-19 patients[54].While this makes the measurement of cardiac troponins less useful from the point of view of diagnosing HF,an elevated troponin level cannot be ignored as it may point towards underlying heart disease in an asymptomatic COVID-19 patient.
ROLE OF CARDlAC POlNT OF CARE ULTRASOUND
The American Society of Echocardiography defines cardiac point of care ultrasound(POCUS)as ‘focused exams with specific imaging protocols based upon suspicion of a specific disease’and differentiates it from ultrasound assisted physical examination[55].POCUS has multiple uses in the diagnosis and management of HF in COVID-19 patients in the ICU.POCUS has the added benefit of reducing risk of exposure to the health-care worker,when compared to the use of stethoscopes[56].Adhering to a setprotocol such as the one described by Huanget al[57],will reduce inter and intraobserver variability.Documenting POCUS findings is important and if possible,the images should be stored on the device or on a central server.As this technology is relatively new,using mannequins for standardized training in image acquisition and interpretation may be helpful[58].
ECHOCARDlOGRAPHY
The American Society of Echocardiography,in a statement endorsed by the American College of Cardiology,recommends that Transthoracic echocardiography should be performed if it is expected to provide clinical benefit[59].In the ICU,this can be done at the bedside,with adequate airborne precautions[59].Echocardiography(ECHO)can provide more information when compared to cardiac POCUS and can also be used to risk stratify patients to aid in follow up.A study of 75 hospitalized patients with COVID-19 showed a significant association between lower LVEF and mortality[60].The mortality among the patients with LVEF < 50% was 65% compared to 26% in the group with LVEF ≥ 50%.The patients with LVEF < 50% also had higher troponin T and pro-BNP levels[60].Stepwise modelling demonstrated that mechanical ventilation(OR 22.6;95%CI:3.0-170.4),LVEF < 50%(OR 8.2;95%CI:1.4-46.9),and pro-BNP above the cohort median value(OR 5.8;95%CI:1.4-23.9)were the strongest predictors of mortality[60].Similar findings were reported by Alvarez-Garciaet al[22],as mentioned previously.Both left ventricular global longitudinal strain(HR 1.39;95%CI:1.11-1.76)and right ventricular longitudinal strain(HR 1.33;95%CI:1.15-1.53)were associated with increased mortality in COVID-19[61,62].ECHO also allows for more detailed evaluation of right heart function,including tricuspid annular plane systolic excursion/pulmonary artery systolic pressure ratio(HR 0.026;95%CI:0.01-0.579;P=0.019)which was an independent predictor of mortality in one study[63].
MANAGEMENT OF ACUTE HEART FAlLURE lN THE lCU
Management of acute HF in COVID-19 patients in the ICU should be done according to established guidelines and protocols.Although questions have been raised about the potential deleterious effects of ACEi and ARBs in COVID-19,a joint statement from the Heart Failure Society of America and American College of Cardiology/American Heart Association recommends continuation of these medications in patients with HF,if hemodynamics allow[64].An effort must be made to identify HF due to takotsubo cardiomyopathy,which may masquerade as an acute coronary syndrome,but is increasingly being recognized in the context of COVID-19[37].Since catecholamine-excess is considered to be part of the pathogenesis behind takotsubo cardiomyopathy,this subset of patients may benefit from restricting the use of catecholamine-inotropes such as dobutamine and dopamine and replacing them with non-catecholamine inotropes such as levosimendan and milrinone[65-67].In patients who develop HF refractory to inotrope support,mechanical circulatory support,e.g.,veno-arterial ECMO or other cardiac assistive devices such as Impella(Abiomed,Danvers,MA,United States)may be used.These interventions are resource intensive and may not be available in all centres.In patients with suspected myocarditis or cytokine mediated injury,high dose corticosteroids,intravenous immunoglobulin and even selective cytokine blockade are options that can be considered on an experimental basis,given the absence of strong evidence of their benefit[68].
EXTRA-CORPOREAL MEMBRANE OXYGENATlON
The World Health Organization has recommended that ECMO can be used in experienced centres for the management of critically ill COVID-19 patients with ARDS with or without HF[69].The Extracorporeal Life Support Organization has emphasized that ECMO should be judiciously used as a rescue strategy in severely ill patients since it is a resource-intensive,highly specialized,and expensive form of life support with the potential for significant complications[70].Key considerations while implementing ECMO include proper patient assessment and selection,personnel assignment,infection control measures before and during ECMO initiation as well as devising protocols for ECMO weaning,decannulation and rehabilitation[71].Given the resource intensive nature of ECMO,some authors have raised the question of whether it is worth using during a pandemic[72].Barbaroet al[73]used the data from the ELSO registry and determined that the mortality in COVID-19 patients who required ECMO was less than 40%.This shows that in the appropriate setting,ECMO is indeed beneficial in critically ill COVID-19 patients.
The role of ECMO after CPR(E-CPR)is unclear at this point,and as of February 3,2021,the Extracorporeal Life Support Organization registry has reported 32 COVID-19 patients who underwent E-CPR[74].Current guidelines recommend judicious use of E-CPR and only in centres that already have experience in its use[70,75,76].Candidate selection should be done with due consideration of the patients comorbidities,other organ function,short and long-term life expectancy,availability of ECMO resources and risk of infectious exposure during cannulation and bed-side management[71].
LEFT-VENTRlCULAR ASSlST DEVlCES
Literature on left ventricular assist devices and COVID-19 are scant.LVADs have been used with varying success in the management of HF in COVID-19.Valchanovet al[77]have described a case of a 43-year patient with severe COVID-19 ARDS and HF who was managed with veno-arterial ECMO and an Impella 5.0 ventricular assist device.The patient,however,succumbed to his illness after a 3-wk period.There are casereports and case-series of patients on long-term LVAD who developed COVID-19[78-82].It is important to recognize that COVID-19 patients with LVADs are particularly prone to thrombotic complications.This requires intensivists to walk a fine line between potential complications of bleeding and thrombosis.In recipients with COVID-19 infection,daily interrogation of LVAD parameters can help in the early recognition of early signs of hemodynamic compromise,pump thrombosis,right ventricular failure,vasoplegia associated with secondary infection,or innate device malfunction[83].
REHABlLlTATlON OF HF PATlENTS WlTH COVlD-19 AFTER lCU DlSCHARGE
Rehabilitation of COVID-19 survivors who were in the ICU is critical.In those who developed HF,this becomes even more important.COVID-19 survivors who were critically ill often develop respiratory sequelae,cognitive sequelae,deconditioning,critical-illness related myopathy and neuropathy,dysphagia,joint stiffness and pain and psychiatric problems[84,85].An early physical medicine and rehabilitation consultation,will help identify and address these issues early on.Rehabilitation can be initiated while the patient is still in ICU.However,more holistic rehabilitation will require assessment of respiratory capacity,muscle strength,exercise capacity,gait speed,balance and activities of daily living[86].This is preferably done in a dedicated rehabilitation facility,after the patient is discharged home[82].A graded exercisebased cardiac rehabilitation strategy can be prescribed,in accordance with standard HF guidelines[87].
Home based cardiac rehabilitation programs with telemonitoring methods can also be considered[88].Few authors have reported promising results with remote cardiac care during the COVID-19 pandemic with telemonitoring devices such as the V-LAP™(Vectorious Medical Technologies,Ltd)device for monitoring left atrial pressure as well as the HeartLogic platform(Boston Scientific,Marlborough,Massachusetts)[89,90].Although this technology is relatively new,we may soon see its integration into rehabilitation protocols for patients with HF,after ICU discharge.
LlMlTATlONS
We identified that only very few studies discussed the medical management of sick patients with COVID-19 in the background of HF.While many studies reported prevalence of ‘cardiovascular disease’and ‘cardiac injury’(usually defined as troponin I above the 99thpercentile upper reference limit or new abnormalities shown on electrocardiography and echocardiography)in COVID-19 patients,the number of studies that reported chronic andde novoHF in this cohort was limited.Part of the reason may be the similarity in presentation of severe COVID-19 ARDS and acute decompensated HF.This is particularly challenging in the ICU patients,in whom both conditions often coexist.Moreover,HF is both a risk factor and a complication of COVID-19.Moreover,studies included in this review were retrospective and lack granular details on the severity of the disease,medical treatment,comorbidities,drug interactions,and outcome.Details of COVID-19 infection on the management of HF and vice versa were also not uniformly addressed.Outcomes in different studies were different.Details of treatment of COVID-19,duration of therapy,length of hospital stay,the long-term outcome were not uniformly available.Details of intensive care treatment,including mode of ventilation,pressors of choice,renal replacement therapies,the role of sedatives and paralytics on this subgroup of populations were also not discussed in all studies.However,the strength of the studies was that it included studies with patients having COVID-19 in the background of HF from all over the world.We also tried to identify the predictors of morbidity and the role of intensive care therapy in these patients,from the literature.More research focusing on this subset of patients is necessary to clarify the pathogenesis,improve screening methods and identify optimal therapeutic strategies.
CONCLUSlON
In this review,we identified that HF is an independent predictor of mortality in hospitalized COVID-19 patients.Patients with HF were more likely to require ventilation,ICU admission and develop complications.Patients with HFrEF did worse than those with HFmrEF and HFpEF.COVID-19 patients with HF should be identified early and managed aggressively in an attempt to improve outcomes in this cohort of patients.
 World Journal of Virology2022年1期
World Journal of Virology2022年1期
- World Journal of Virology的其它文章
- Role of vitamin D deficiency and comorbidities in COVlD-19
- Repurposing the antioxidant and anti-inflammatory agent N-acetyl cysteine for treating COVlD-19
- Rethinking hospital psychiatry in ltaly in light of COVlD-19 experience
- Chronic hepatitis B:New potential therapeutic drugs target
- Animal models for SARS-CoV-2 and SARS-CoV-1 pathogenesis,transmission and therapeutic evaluation
- COVlD-19:A pluralistic and integrated approach for efficient management of the pandemic
