Precision medicine in sepsis and septic shock: From omics to clinical tools
Juan Carlos Ruiz-Rodriguez, Erika P Plata-Menchaca, Luis Chiscano-Camón, Adolfo Ruiz-Sanmartin, Marcos Pérez-Carrasco, Clara Palmada, Vicent Ribas, Mónica Martínez-Gallo, Manuel Hernández-González, Juan J Gonzalez-Lopez, Nieves Larrosa, Ricard Ferrer
Juan Carlos Ruiz-Rodriguez, Luis Chiscano-Camón, Adolfo Ruiz-Sanmartin, Marcos Pérez-Carrasco, Clara Palmada, Ricard Ferrer, Intensive Care Department, Vall d’Hebron Hospital Universitari, Vall d’Hebron Barcelona Hospital Campus, Barcelona 08035, Spain
Juan Carlos Ruiz-Rodriguez, Erika P Plata-Menchaca, Luis Chiscano-Camón, Adolfo Ruiz-Sanmartin, Marcos Pérez-Carrasco, Ricard Ferrer, Shock, Organ Dysfunction and Resuscitation Research Group, Vall d’Hebron Institut de Recerca (VHIR), Vall d’Hebron Barcelona Hospital Campus, Barcelona 08035, Spain
Juan Carlos Ruiz-Rodriguez, Luis Chiscano-Camón, Adolfo Ruiz-Sanmartin, Ricard Ferrer,Departament de Medicina, Universitat Autònoma de Barcelona, Bellaterra 08193, Spain
Erika P Plata-Menchaca, Department of Intensive Care, Hospital Clínic de Barcelona, Barcelona 08036, Spain
Vicent Ribas, Data Analytics in Medicine, Digital Health Unit, Eurecat, Centre Tecnològic de Catalunya, Barcelona 08005, Spain
Mónica Martínez-Gallo, Manuel Hernández-González, Immunology Division, Vall d’Hebron Hospital Universitari, Vall d’Hebron Barcelona Hospital Campus, Barcelona 08035, Spain
Mónica Martínez-Gallo, Manuel Hernández-González, Diagnostic Immunology Research Group,Vall d’Hebron Institut de Recerca (VHIR), Vall d’Hebron Barcelona Hospital Campus,Barcelona 08035, Spain
Mónica Martínez-Gallo, Manuel Hernández-González, Department of Cell Biology, Physiology and Immunology, Universitat Autònoma de Barcelona, Bellaterra 08193, Spain
Juan J Gonzalez-Lopez, Nieves Larrosa, Department of Clinical Microbiology, Vall d’Hebron Hospital Universitari, Vall d’Hebron Barcelona Hospital Campus, Barcelona 08035, Spain
Juan J Gonzalez-Lopez, Nieves Larrosa, Department of Microbiology and Genetics, Universitat Autònoma de Barcelona, Bellaterra 08193, Spain
Abstract Sepsis is a heterogeneous disease with variable clinical course and several clinical phenotypes. As it is associated with an increased risk of death, patients with this condition are candidates for receipt of a very well-structured and protocolized treatment. All patients should receive the fundamental pillars of sepsis management, which are infection control, initial resuscitation, and multiorgan support. However, specific subgroups of patients may benefit from a personalized approach with interventions targeted towards specific pathophysiological mechanisms. Herein, we will review the framework for identifying subpopulations of patients with sepsis, septic shock, and multiorgan dysfunction who may benefit from specific therapies. Some of these approaches are still in the early stages of research, while others are already in routine use in clinical practice, but together will help in the effective generation and safe implementation of precision medicine in sepsis.
Key Words: Sepsis; Septic shock; Organ dysfunction; Precision medicine; Biomarkers;Phenotype; Endotype
lNTRODUCTlON
Sepsis requires a structured and protocolized treatment, which have been thoroughly reviewed in the literature[1-3]. The last version of the Surviving Sepsis Campaign(SSC) guidelines was released in 2021[4], and the hour-1 bundle was updated in 2018[5]. The implementation of the SSC recommendations and bundles[6] is associated with a sustained reduction in the risk of death. Still, mortality from sepsis remains unacceptably high[7].
All patients with sepsis are candidates for receipt of the main pillars of sepsis treatment: Infection control, initial resuscitation, and multiorgan support. However,specific subgroups of patients not responding to conventional therapies may benefit from other therapies, which can be considered therapeutic rescue strategies.
Currently, sepsis is defined as organic dysfunction associated with a dysregulated response of the host to infection[8]. The host response is initiated when bacterial endotoxin or other bacterial structures interacting with the host´s immune system stimulate the production of a cascade of immune mediators that activate and target leukocytes, leading to organ dysfunction.
SEPSlS: A HETEROGENEOUS DlSEASE
We have to ask ourselves whether all septic patients' clinical courses are predictable.Does dysregulated host response to infection progress and manifest similarly in all patients? The answer is clear and resounding: No. In sepsis, there is significant heterogeneity between individuals. In a certain way, such heterogeneity is foreseen based on the existing differences in age, causative microorganisms, types of sepsis foci, and comorbidities. Pathophysiologically, there are also significant differences. The inflammatory response occurs in two distinct stages: The pro-inflammatory and the antiinflammatory phases. These phases vary among individuals and within the same individual, depending on a particular moment within the clinical course. This could explain the observed heterogeneity in responses to available immunomodulating treatments (e.g., corticosteroids, elimination of cytokines, and anti-cytokine antibodies).
Therefore, patients with a low risk for adverse outcomes are candidates to receive conventional treatments. In contrast, patients with a high risk of clinical deterioration could benefit from specific therapies addressing their particular pathophysiological characteristics. This gives rise to so-called ‘precision medicine’. This term comes from oncology and described the adaptation of a treatment to each patient’s traits based on the genomic study and the molecular characteristics of tumors.
In this narrative review, we explain the different strategies to create and implement precision medicine for sepsis, with the intent of supporting individualization of patients’ management (Figure 1). In the first part of this manuscript, we will review the technologies developed to identify endotypes and phenotypes (omics-based biomarkers, bioinformatics, and biomarkers commonly used in the clinic). In the second part of the manuscript, we will describe the different endotypes with their specific potential treatments (e.g., immunoglobulins, endotoxin- and cytokinehemadsorption, restoration of immunoparalysis) (Table 1). Omics-based biomarkers research is still in the early stages, while other biomarkers are now available and in use in the clinic.

Table 1 Clinical applicability of precision medicine strategies
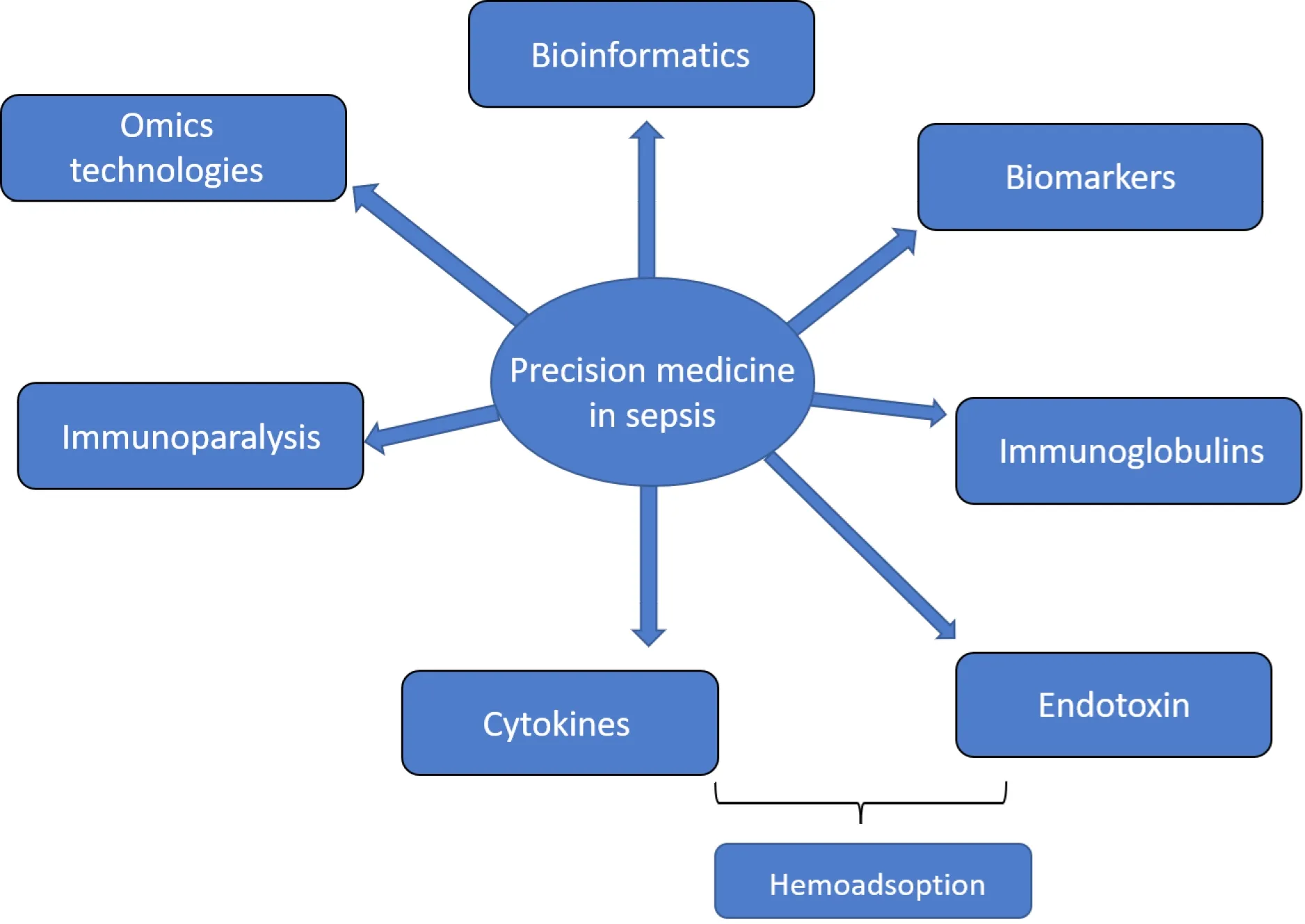
Figure 1 Strategies to create precision medicine in sepsis.
TECHNOLOGlES DEVELOPED TO lDENTlFY ENDOTYPES AND PHENOTYPES
Omics technologies
Novel technologies have been developed in recent years to detect different evolutionary patterns or other patterns in response to different therapies in sepsis.Omics-based biomarkers and bioinformatics can select various endotypes and phenotypes of sepsis patients indistinguishable from the clinical point of view at the bedside. Therefore, they help in the adaptation of specific therapies to patients according to their individual characteristics[9].
Genomics and epigenomics:Genomics is defined as the study of genes and their functions. The different clinical presentations and prognoses of sepsis patients have already been associated with particular genetic variants. A genetic polymorphism is an allelic variant that exists in an unalterable state in a population, with a frequency(generally > 1%) that cannot be accounted for by new mutations. Various polymorphisms have been described in the genes that encode pro-inflammatory and antiinflammatory cytokines. This is also true for cytokine receptors, cellular recognition pathways, intracellular signaling pathways, and hemostasis molecules. All these pathways are involved in the severity and risk of mortality in sepsis[10].
Epigenomics studies the additional changes that alter gene expression without changing the DNA sequence. These include DNA methylation, non-coding (nc)RNAs,histone variants, and histone post-translational modifications. Epigenetic modifications can respond to environmental stimuli by activating or inhibiting gene transcription. Lorente-Sorollaet al[11] showed that sepsis patients undergoing widespread changes in the methylome of their circulating monocytes had associated aberrant levels of interleukin (IL)-10 (IL-10) and IL-6, and a high occurrence of organ dysfunction. Changes in histone modifications, especially histone acetylation, can lead to abnormal expression of IL-10 mRNA[12]. An ncRNA is a functional RNA molecule transcribed from DNA, though not translated into a protein. ncRNAs regulate gene expression at the transcriptional and post-transcriptional levels. The three major classes of short ncRNAs are known as micro (mi)RNAs, short interfering (si)RNAs,and piwi-interacting (pi)RNAs. Plasma levels of miR-133a are higher in critically ill patients with sepsis than in patients with non-infectious inflammation, and predict intensive care unit (ICU) and long-term mortality[13]. Consequently, epigenetic biomarkers could help detect patients with clinical deterioration and unfavorable evolution[11-14].
Individualized treatment based on the genetic characteristics of the host has not yet been implemented in clinical practice, even though it is undoubtedly one of the most promising research fields for the future management of patients with sepsis and septic shock.
Transcriptomics:The transcriptome is the set of messenger RNAs and ncRNA molecules in a specific cell or tissue. Transcriptomics is the study of the transcriptome of one particular cell or tissue in a specific circumstance, based on the analysis of gene expression profiles. It aims at monitoring gene activity and regulation. Transcriptomic studies have made possible the characterization of different gene expression profiles in sepsis.
Interindividual transcriptome variation in sepsis has been evaluated in several large cohorts. Masloveet al[15] identified two subtypes in septic patients. The subtype 1 gene expression profile is characterized by a significantly increased expression of genes involved in inflammatory and Toll-like receptor (TLR)-mediated signaling pathways. This profile is associated with a higher prevalence of sepsis. Davenportet al[16] analyzed peripheral blood leucocyte global gene expression of 265 critically ill patients with community-acquired pneumonia and organ dysfunction. That transcriptomic study showed two distinct sepsis response signatures:SRS1andSRS2.SRS1, present in 41% of patients, identified patients with an immunosuppression phenotype that included features of endotoxin tolerance, T cell exhaustion, and downregulation of human leucocyte antigen class II.SRS1was associated with higher 14-,28- and 60-d mortality thanSRS2. Sweeneyet al[17] performed an unsupervised clustering analysis on pooled transcriptomic profiles from 14 datasets of sepsis patients (n= 700). The authors described three transcriptomic subtypes based on their functional analysis: the inflammopathic, adaptive, and coagulopathic subtypes. The adaptive subtype was associated with a lower clinical severity and lower mortality rate than the other subtypes. The coagulopathic subtype was associated with higher mortality and occurrence of clinical coagulopathy than either the adaptative or inflammopathic subtypes. Septic shock was more frequent in the inflammopathic subtype.Wonget al[18,19] conducted a genome-wide expression profiling using whole bloodderived RNA from 98 children with septic shock, and identified three subclasses of patients, which they designated as A, B, and C. Patients in subclass A were characterized by repression of genes corresponding to adaptive immunity and glucocorticoid receptor signaling. The subclass A patients had higher illness severity and mortality rate than the patients in subclasses B and C.
In the future, transcriptomic studies should help us in the early identification of patients with evolutionary patterns associated with greater severity and mortality,allowing for more personalized treatment.
Metabolomics:Metabolomics is the study of the metabolome, a collection of small molecules produced by cells[20]. This technology has been increasingly used in various investigations, such as the identification of biomarkers, drug activities, or drug-induced toxicity and metabolism. Critical illnesses, such as sepsis, alter the metabolomic profile. Thus, metabolomic studies in sepsis have been aimed at discovering metabolites that discriminate between patients with sepsis and noninfectious systemic inflammatory response syndrome (SIRS), identifying prognostic factors, and recognizing changes in response to treatment[21].
Suet al[22] studied a total of 65 patients (35 with sepsis, 15 with SIRS, and 15 healthy subjects). Levels of dimethylisine, 2-phenylacetamide, glyceryl-phosphoryl-ethanolamine, and D-cysteine were associated with the severity of sepsis. In addition, four other metabolites (S-(3-methylbutanoyl)-dihydrolipoamide-E, glycerophosphocholine,and S-succinyl-glutathione) were elevated within 48 h prior to death, indicating their potential use in predicting mortality. Neugenbaueret al[23] demonstrated that high levels of putrescine,lysoPCaC18:0, andSM C16: 1are associated with higher mortality in community-acquired pneumonia and intra-abdominal infections. In a previous study, Mickiewiczet al[24] found 20 metabolites significant for discrimination between survivors and non-survivors. The pathways highlighted in this study were related to energy metabolism and branched-chain amino acid processes.
Metabolomic studies have characterized the fundamental role of lysophospholipids,especially lysophosphatidylcholine (LPC), in sepsis prognosis[25-27]. Ferrarioet al[28]studied the changes in lipid homeostasis that occur during sepsis progression. Plasma samples from 20 patients with septic shock were studied on days 1 and 7 of septic evolution. The authors identified 137 metabolites, many of which were significantly different between survivors and non-survivors. LPC and phosphatidylcholine were found at lower levels in non-survivors than in survivors on day 1 and day 7. Using regression models, the lowest levels of LPC on day 7 were identified as the strongest predictors of mortality. Drobniket al[26] observed that the LPC concentration was markedly reduced in patients with sepsis compared to controls, and a negative correlation between these levels and mortality was found. Instead, Choet al[25] found no association between low LPC levels and severity of the disease in septic patients.They also observed no differences in LPC levels between survivors and non-survivors.
In sum, metabolomics is a tool that allows for predicting the severity and prognosis of sepsis patients. This technology also provides a higher level of biochemical detail and knowledge than other systems biology approaches.
Proteomics:Proteomics is the part of omics that is responsible for the study of the proteome. The proteome comprises the set of all proteins expressed by the genome of a cell, tissue, or organism at a given time and under certain conditions of time and environment[29]. This technology provides an analysis of the expression, location,function, and interaction of proteomes. Compared to other immunological tests,proteomics is a novel method that has the advantage of having high throughput,sensitivity, and specificity. The development of proteomics has provided a means to study cellular processes, such as cell signaling, identifying protein modifications, and the characterization of specific biological markers[30].
For more than a decade, the study of proteomics has been sought to find new biomarkers determining sepsis diagnosis and prognosis. Suet al[31] selected 192 proteins in patients with sepsis and septic shock for investigation. Of these, vimentin(a molecule that modulates lymphocyte apoptosis and inflammatory response)increased significantly in patients with sepsis and septic shock compared to controls.The non-survivors had higher vimentin levels in serum, and its expression was increased in lymphocytes in particular. As such, this molecule could be a marker for prognosis prediction in patients with sepsis. In a previous study of 16 critically ill patients, Punyadeeraet al[32] found that a combination of various proteins [e.g., IL-1α,interferon gamma-induced protein 10 (IP-10), soluble tumor necrosis factor receptor(sTNF-R)2 and soluble cell death receptor (sFAS)] could induce the progression of sepsis to septic shock. Furthermore, a combined measurement of matrix metalloproteinase (MMP)-3, IL-1α, IP-10, soluble IL-2 receptor (sIL-2R), sFas, sTNF-R1, soluble receptor for advanced glycation end products (i.e., sRAGE), granulocyte-macrophage colony-stimulating factor (GM-CSF), IL-1β, and eotaxin could differentiate survivors from non-survivors. Latour-Pérezet al[33] observed that increased levels of activator receptor 1 expressed in myeloid cells (i.e., sTREM-1) throughout the first 3 d of evolution were associated with high mortality in critically ill patients with sepsis. The high initial severity of illness explained this finding. Gibotet al[34] found that the progressive decrease in plasma concentrations of sTREM-1 indicated a favorable clinical course during the recovery phase of sepsis and discriminated between survivors and non-survivors. Decouxet al[35] analyzed the serum proteome in a group of patients with early sepsis. To cope with the large dynamic range of serum protein samples, the authors performed N-glycosylation, a chemical enrichment of glycopeptides and subsequent differences were found in the serum proteome between survivors and non-survivors. For instance, some modified proteins and glycopeptides belong to common pathways, such as the coagulation cascade and the complement system. The authors also found decreased total neutrophil gelatinase-associated lipocalin (NGAL) and vascular cell adhesion molecule 1 (VCAM-1) levels in nonsurvivors, two molecules believed to be part of the inflammatory response. Thus, even though VCAM and NGAL increase in sepsis, their study suggested that these increases may be part of a beneficial response necessary for survival, and pointed to the complexity of the regulatory network that is already activated in these patients at an early stage.
Proteomics has also helped to understand the role of proteolysis in sepsis by studying circulating peptides. Bauzá-Martinezet al[36] described a higher number of circulating peptides in patients with septic shock than in sepsis patients or non-hospitalized healthy subjects. The peptide count and abundance in septic shock patients were higher in non-survivors than in survivors, suggesting an association between the magnitude of proteolysis and the outcome. The predominant role of serine proteases,such as chymotrypsin and MMPs, in causing the observed proteolytic degradation was demonstrated.
Ultimately, proteomics helps increase our understanding of the pathophysiology of sepsis and identify new molecules that can predict patients’ evolution. This technology also aids in the identification of significant prognostic factors in sepsis patients.Therefore, proteomic approaches are promising for clinical applications and biomarker studies of sepsis.
Bioinformatics
A major trend today in research is improving the accuracy of the diagnosis of sepsis.The definition of sepsis was updated in 2016 and advocated using the quick Sequential Organ Failure Assessment (qSOFA), which assesses blood pressure, respiratory rate,and mental status for sepsis diagnosis[8]. A major criticism by the medical community of this score lies in its low specificity[37]. For this reason, different research teams are trying to enhance this scale through the addition of bedside parameters (e.g., biomarker data), which could improve these diagnostic criteria. Another critical aspect in clinical research is obtaining a set of baseline phenotypes and patient trajectories in the ICU through multivariate analysis techniques, such as principal component analysis,factor analysis, and probabilistic clustering. For instance, a previous study[38] defined the following four different phenotypes for sepsis through consensus k-means clustering: (1) Patients with low vasopressor titration; (2) Patients with chronic conditions and renal dysfunction; (3) Patients with high inflammation and pulmonary dysfunction; and (4) Patients with liver dysfunction and septic shock. Another study[39] defined the following phenotypes predicting ICU outcomes: (1) Patients requiring mechanical ventilation support; (2) Patients with severe organ dysfunction; (3) Patients with high severity scores; and (4) Patients with hepatic dysfunction.
Therefore, improved versions of the qSOFA scale are evaluated in the context of all available data at hospital admission through standard machine learning techniques,such as multivariate logistic regression, relevance vector machines, support vector machines, shallow neural networks or random forests, taking the diagnosis of sepsis confirmed through hemocultures as the main outcome. To predict organ dysfunction before its onset, phenotypes are now being improved by adding different clinical traits and biomarkers that become altered before organ dysfunction is detected at a systemic level. Current initiatives are intended to enhance these phenotypes by applying a generalization of the factor analysis method with Deep Autoencoders to assess the strength of associations between variables and their importance within each patient phenotype.
Deep Reinforcement Learning has also become an important research line for assessing the continuum of organ dysfunction in sepsis. For instance, Raghuet al[40]proposed a continuous state-space model for sepsis management in a twist beyond the more traditional development and use of discriminative classifiers.
Other studies have used Bayesian Networks and Random Forests[41] for assessing patient trajectories of septic and septic shock patients in the acute phase. A common trend between these initiatives is that they all pave the way to study patient trajectories in the ICU. Patient trajectory assessment includes studying the prevalence of each phenotype and their impact on other clinical outcomes, such as long-term survival (e.g., 100-d survival rate), vasopressor resistance, and days on organ support[38,39,42].
An accurate assessment of the organ dysfunction continuum is possible with the inclusion of biomarker data (e.g., complement cascade, platelet degranulation, acute inflammation response, negative regulation of endopeptidase activity, and blood coagulation), through the development of comprehensive, interpretable and mathematically rigorous models of knowledge representation through Deep Learning techniques such as Deep Reinforcement Learning and standard machine learning techniques based on graphical models[42]. These techniques will improve diagnosis,trajectory, and long-term survival prediction in sepsis and septic shock. Also, they could set the basis for the personalized treatment of organ dysfunction.
Available biomarkers at clinics
The reliability of clinical assessments in patients with sepsis is often limited, and there is a need to individualize decision-making processes based on objective data. The heterogeneity of patients with sepsis has led to the use of biomarkers for patient stratification according to prognosis and severity of illness, improving phenotyping,intensifying medical therapy in high-risk patients, guiding antimicrobial stewardship,and allocating hospital resources.
Procalcitonin (PCT) is the most widely studied biomarker and is helpful as an adjunctive clinical tool for predicting prognosis and supporting clinical decisions in sepsis[43]. In a previous study of patients with septic shock and high vasopressor requirements, patients who had PCT levels of > 2 ng/mL benefited from receiving adjuvant therapy with hydrocortisone, vitamin C, and thiamine to reduce the progression of organ dysfunction[44]. High initial levels of PCT (> 6 ng/mL) are helpful to predict progressive organ dysfunction and an increased risk of mortality[45]. Thus, this subgroup of patients may be considered for receiving personalized rescue therapies, as conventional treatment may be insufficient to improve prognosis.Interestingly, PCT non-clearance is a predictor of adverse outcomes and treatment failure[46-48]. In a large observational study, the inability to decrease PCT by more than 80% was a significant independent predictor of mortality[49]. This finding may aid in sepsis care, potential suitability of adjuvant treatments, and allocation of resources. Well-designed randomized controlled trials (RCTs) and meta-analyses have shown a mortality benefit when using PCT-guided algorithms for antimicrobial stewardship in sepsis[50-52].
Mid-region fragment of pro-adrenomedullin (MR-proADM) is a biomarker mainly produced by vascular endothelial cells. MR-pro-ADM directly reflects plasma levels of adrenomedullin, a potent vasodilator agent with metabolic and immune-modulating properties. MR-proADM levels increase in sepsis, and high plasma clearance at day 5 has been associated with better outcomes[53]. Furthermore, the role of this biomarker for the early identification of patients at higher risk of organ dysfunction has been recognized. In a recent study, the use of MR-proADM performed better in the prediction of mortality compared to lactate, PCT, C-reactive protein, and SOFA score[54]. Former studies have evaluated MR-proADM to predict ICU admission and the need for urgent treatment[55]. Thus, MR-pro-ADM is found beneficial to guide clinical decisions regarding the use of ICU and hospital resources.
The use of sepsis biomarkers is evolving as one of the most promising developments in precision medicine. Identifying additional reliable biomarkers in sepsis will significantly improve our understanding of this heterogeneous disease and help the medical community refine clinical assessments. Likewise, comprehensive clinical assessments should be the starting point for developing and studying clinically accurate biomarkers in sepsis[56,57].
Recent progress in several biomarker research areas, including the development of point-of-care testing technologies[58], will extend their application for diagnosis, risk stratification, molecular phenotyping, and monitoring therapeutic responses, leading to more personalized medicine at the bedside. Further clinical validation of current biomarkers should be sought in certain patients [e.g., renal dysfunction, receiving continuous renal replacement therapy (i.e.CRRT), trauma]. Point-of-care sepsis biomarkers have the potential to be a game-changer as their implementation becomes widely available.
ENDOTYPES AND SPEClFlC POTENTlAL TREATMENTS
Immunoglobulins
The pathogenesis of sepsis is associated with dysregulation of the innate and adaptive immune systems. The adaptive immune system’s underlying altered mechanism is the function of antibodies and immunoglobulins (Igs)[59]. Still, the SSC guidelines[4]make a weak recommendation for using Igs as a potential treatment in sepsis patients,given the low certainty of evidence derived from the main studies and a meta-analysis[60,61]. Although the previous studies have not assessed Igs’ baseline status as an inclusion criterion, it is reasonable to think that patients with hypogammaglobulinemia could benefit from Ig treatment.
The underlying mechanisms causing decreased levels of Igs in sepsis are not entirely clear. Still, impaired Ig production, vascular leakage secondary to endothelial dysfunction, an imbalance between IgG production and its utilization by the complement system, excessive catabolism, or reduced plasma cell Ig secretion may be involved. Also, patients with sepsis frequently have lymphopenia and quantitative or functional abnormalities within T cell and B cell populations[62].
Several studies have shown higher mortality in sepsis patients with hypogammaglobulinemia. Although the definition of hypogammaglobulinemia is variable, low levels of gammaglobulins can be defined as IgG below 500 mg/dL in individuals older than 5 years or 2 standard deviations below reference values for age[63-67]. Low plasma levels of IgG (hypo-IgG) is the most common deficiency, with a prevalence as high as 70%[68]. Hypo-IgG is associated with an increased risk of severe illness [higher acute physiology and chronic health evaluation II (i.e.APACHE II) score], a greater incidence of acute respiratory distress syndrome, and a longer duration of shock[69],especially on the day of diagnosis and the following 48 h[70]. Also, a synergistic role of IgG, IgM, and IgA in sepsis and septic shock has been described[66,71]. The combined presence of low levels of endogenous IgG, IgM, and IgA in plasma is associated with reduced survival in patients with sepsis or septic shock[72].
Some studies have reported that immunoglobulin formulations containing IgG did not improve mortality rates in patients with sepsis[60]. Conversely, Welteet al[73]demonstrated a clinically significant reduction of mortality risk in patients with pneumonia treated with intravenous Ig (IVIg). That study identified a population with a very high risk of mortality, namely patients with high levels of C-reactive protein and PCT, and hypo-IgM.
Polyvalent intravenous Igs represent a promising approach to modulate both the pro-and anti-inflammatory responses[74]. In adults, the use of IgM-enriched IVIg has shown favorable results[60,61,73-79]. IgM-IgA-enriched IVIg preparations are associated with a reduction in mortality[61,73,75,76]. A recent meta-analysis of 19 trials and > 1500 patients showed a significant reduction in mortality when using IgM- and IgA-enriched IVIg compared to human albumin solution or no treatment[80,81].However, the eligibility criteria for receiving polyvalent IVIg and the best treatment strategy should be well defined[77]. The administration of a single dose of polyclonal gammaglobulin of 1 or 2 g/kg is widely accepted (level of evidence 2C)[82]. Other strategies propose IgM and IgA-enriched polyclonal IVIg dose of 250 mg/kg/d by a 10-h infusion, for 3 consecutive days[83], or an infusion of 42 mg/kg body weight of IgM-enriched polyclonal IVIg once daily for 5 consecutive days[73]. In a retrospective study, 129 adult patients benefited from receiving IgM-IgA enriched IVIg, when the administration was performed within the first 23 h from admission[78].
The routine administration of IVIg in sepsis patients is not recommended, as stated in the 2016 SSC. However, patients with hypogammaglobulinemia could benefit from this treatment. Further studies are needed to clinically validate the most appropriate dose and administration regimen of IVIg in sepsis patients with hypogammaglobulinemia.
Endotoxin hemoadsorption
Endotoxin is a lipopolysaccharide (LPS) present in the outer membrane of Gramnegative bacteria and is one of the best examples of pathogen-associated molecular patterns (i.e.PAMPs). Its presence, together with that damage-associated molecular patterns (i.e.DAMPs) released by host injured cells, results in the elevation of proinflammatory and anti-inflammatory cytokines[84], activating the anti-infectious innate immune response and mediating the clinical syndrome of sepsis. LPS elicits its actions through a transmembrane protein, the TLR4, a type of pattern recognizing receptor expressed on innate immune system cells, in a process in which many important molecules are involved. In this process, the LPS-binding protein (i.e.LBP)transports circulating endotoxin and facilitates its recognition by the cell through receptor CD14. CD14 directs the LPS-LBP complex to TLR4, and the accessory protein myeloid differentiation 2 (MD2) associated with TLR4 on the cell surface is involved in the LPS-TLR4 union. Recognition of the LPS-LBP complex by these receptors transduces the endotoxin signal to the cell nucleus, leading to the expression of a complex network of inflammatory mediators. The presence of endotoxin activates changes in the expression of more than 300 genes, leading to the activation of macrophages, endothelial cells, neutrophils, and the coagulation cascade. It also triggers the release of a complex cascade of host-derived inflammatory mediators[85,86].
Endotoxin activity has emerged as a valuable marker of disease severity. The lipid-A domain of endotoxin induces most of the toxicity associated with LPS, characterized by fever, diarrhea, hemodynamic instability, multiple organ failure, and, ultimately,death[87]. A previous study highlighted the clinical relevance of circulating levels of LPS, showing a significant correlation between endotoxin levels and severity of septic shock, organ dysfunction, and mortality[86]. The prevalence of endotoxemia in patients with septic shock was high, and up to 82% of patients showing intermediate or high endotoxin activity[88]. Patients with endotoxemia also presented significantly higher lactate concentration and inotropic score.
In human illness, the measurement of endotoxin is notoriously difficult. The chromogenic limulus amebocyte lysate assay was the first diagnostic test developed. It was based on endotoxin’s ability to induce coagulation of proteins in the hemolymph of the horseshoe crab,Limulus polyphemus[89]. Since other microbial products,especially from fungi, can activate the limulus reaction, the assay is not specific for endotoxin. Since 2004, the endotoxemia measurement in humans has been made through the Endotoxin Activity Assay (EAA), a chemiluminescent rapid (30-min)assay described by Romaschin in 1998[90]. That test is based on the ability of an antibody to form an antibody-antigen complex in whole blood. This antibody targets the highly conserved lipid A epitope of endotoxin. It has a very high binding affinity,leading to very high sensitivity. In addition, the antibody does not cross-react with Gram-positive or fungal components, allowing for very high specificity. The results are expressed in EAA units, where < 0.39 is considered low, 0.40-0.59 intermediate,and ≥ 0.60 high. As this assay uses patient’s neutrophils as a readout system, it is impossible to store specimens for later assaying, and measurements must be performed within 3 h of obtaining the sample. The EAA is the only assay that is approved by the United States’ Food and Drug Administration for measuring endotoxin activity in whole blood.
Endotoxin has been considered as one of the therapeutic targets for the treatment of sepsis and septic shock. The possibility of eliminating endotoxin through blood purification techniques and, specifically, by hemoadsorption has been raised.Adsorption with a fiber column immobilized with polymyxin B (PMX) (Toraymyxin®;Toray, Tokyo, Japan), is one of the best-known endotoxin elimination therapies.Another possibility is the oXiris®hemofilter (Baxter, Meyzieu, France).
Four clinical trials have evaluated the efficacy of endotoxin hemoadsorption in septic shock. In a multicenter, open-label, pilot, randomized, controlled study conducted in Europe, 36 postsurgical patients with severe sepsis or septic shock secondary to intraabdominal infection were randomized to receive PMX treatment over 2 h (n= 17) or standard therapy (n= 19)[91]. There were no statistically significant differences in endotoxin levels from baseline to 6, 8 or 24 h after treatment between the two groups. Five of the eighteen (28%) patients in the control group and five of the seventeen (29%) patients in the PMX group died during the study period. The survival analysis showed no statistical significance between the two groups. There was also no statistically significant difference in the mean duration of ICU stay nor the number of ICU-free days between the two groups. However, patients treated with PMX demonstrated substantial increases in cardiac index and oxygen delivery index, and the need for CRRT after study entry was reduced. PMX was well tolerated and showed no significant side effects. Thus, that study showed the PMX cartridge to be safe and to have the potential to improve cardiac and renal dysfunction due to sepsis or septic shock. The early use of polymyxin B hemoperfusion in abdominal septic shock (i.e.EUPHAS) trial[92] evaluated hemoperfusion with PMX in a small sample of 64 patients with intraabdominal infection-related severe sepsis and septic shock. The design was oriented to assess hemodynamic improvement. The recovery of mean arterial pressure allowed for the reduction of vasoactive drugs in the PMX group.SOFA scores improved in the PMX group. Furthermore, a significant reduction in 28-d mortality was observed in the intervention group (32%) compared to the conventional treatment group (53%). The ABDOMIX trial[93] studied 243 patients with septic shock within 12 h after emergency surgery for secondary peritonitis due to organ perforation. The PMX hemoperfusion (i.e.PMX-HP) group (n= 119) received conventional therapy plus two sessions of PMX-HP. There were no significant differences in the SOFA score nor the 28-d mortality rate between PMX-HP and control groups(27.7%vs19.5%). The severity of the disease and mortality were moderate. Among the 220 sessions performed, a premature interruption was observed in 25 cases (11%),mainly during the first session and primarily due to circuit clotting. A total of two PMX-HP sessions were completed in only 81 of 119 patients (69.8%). Of note, plasma EAA levels were not measured in any RCTs previously discussed.
The Euphrates trial[94] is one of the RCTs with the largest sample of patients and features the highest scientific rigor. Among its main characteristics is the use of EAA as a predictive biomarker. This trial studied 450 critically ill patients with septic shock and an EAA level of 0.6 or higher. The intervention consisted of two PMX-HP treatments (90-120 min) plus standard therapy, completed within 24 h of enrollment (n= 224) or sham hemoperfusion plus standard therapy (n= 226). PMX-HP was not associated with a significant difference in 28-d mortality. However, Kleinet al[95]performed a post-hoc analysis of 194 patients with EAA between 0.6-0.89. A survival benefit was observed in patients who received therapy with PMX hemofilters. Montiet al[96] published the first study describing the use of PMX-HP as rescue therapy,involving 52 patients with refractory septic shock unresponsive to conventional therapy. The SOFA score was 10 (8-14) points and serum lactate level was 5.89 ± 4.04 mmol/L. All patients were on mechanical ventilation, and 90% were treated with corticosteroids. Rapid and early reversal of circulatory dysfunction and other organ failures were obtained. The overall 30-d mortality was lower (29%) than expected by the SAPS II score (47%).
Consequently, it seems reasonable that patients with refractory septic shock and severe multiorgan dysfunction, with adequate control of the focus and EAA 0.6-0.9 could be candidates for endotoxin hemoadsorption. The TIGRIS study[97] is ongoing,recruiting patients with SOFA score > 9 and EAA levels between 0.60 and 0.89. The results of that study will provide more information on the possible benefits of endotoxin hemoadsorption in patients with septic shock, high requirement for vasopressor support, and severe multiorgan dysfunction.
Cytokine hemoadsorption
Sepsis appears when the initially appropriate host response to infection becomes amplified and subsequently dysregulated, leading to an imbalance between proinflammatory and anti-inflammatory responses[98]. An excess of pro-inflammatory cytokines can lead to endothelial injury and SIRS. Severe cases can progress to disseminated intravascular coagulation and multiple organ failure that eventually leads to death[99].
A tightly regulated balance in the cytokine network is crucial for eliminating invading pathogens on the one hand and restricting excessive, tissue-damaging inflammation on the other. This network comprises pro-inflammatory cytokines[tumor necrosis factor-alpha (TNF-α), IL-1, IL-6, IL-12, interferon-gamma (IFN-γ) and macrophage migration inhibitory factor (MIF)], anti-inflammatory cytokines [IL-10,transforming growth factor-beta (TGF-β), and IL-4], and soluble inhibitors of proinflammatory cytokines[100], such as soluble TNF receptor (TNFR), IL-1 receptor antagonist (IL-1Ra), and IL-2 receptor antagonist (IL-1R2)[101,102]. In endothelial cells,TNF-α enhances the expression of adhesion molecules and increases integrin adhesiveness in neutrophils, promoting their extravasation into tissues[103,104]. TNFα and IL-1 are the main mediators of inflammation-induced activation of coagulation[105]. In addition, TNF-α and IL-1 amplify inflammatory cascades in an autocrine and paracrine manner by activating macrophages to secrete other pro-inflammatory cytokines, lipid mediators, and reactive oxygen and nitrogen species, leading to sepsisinduced organ dysfunction[98,106]. A key function of IL-6 is the induction of fever[107] and the mediation of the acute phase response[108,109]. The high concentration of IL-6 binds to the soluble form of the IL-6 receptor. This complex combines with the signal-transducing component glycoprotein 130 on the cells, including endothelial cells, to elicit IL-6 signal activation. Despite its pro-inflammatory properties, IL-6 also has been shown to promote anti-inflammatory responses. IL-6 inhibits the release of TNF-α and IL-1[110] and enhances the circulation levels of anti-inflammatory mediators[111-113]. IL-10 and TGF-β suppress the production of pro-inflammatory mediators in immune cells and stimulate the production of IL-1Ra and sTNFRs[114,115].
Several studies have suggested an association of IL-6 hypercytokinemia with organ dysfunction, response to treatment, and prognosis in sepsis. Kellumet al[116] found that 82% of patients with community-acquired pneumonia had a systemic elevation of cytokine levels. Furthermore, patients with higher levels of IL-6 and IL-10 had associated severe organ dysfunction[117,118] and higher mortality[116,118]. The association between high levels of IL-6 and IL-10 with organ dysfunction and mortality has been confirmed in other studies[117-120]. Patients who survive sepsis show a rapid decrease in IL-6 Levels, in contrast to the non-decreasing values or a slowly progressive decrease in non-survivors[119,120]. Thus, the reduction of IL-6 Levels is associated with a better prognosis[121], and IL-10 overproduction is the main predictor of severity and mortality[122,123].
Given the central role of increased systemic inflammation in the pathophysiology of sepsis-induced organ dysfunction, the development of therapies aimed at dampening the cytokine storm could help improve immune homeostasis. Extracorporeal blood purification therapies have been proposed as a strategy to improve the outcome of septic patients, attenuating the systemic expression of pro-inflammatory and antiinflammatory mediators and restoring immune homeostasis[116]. These include different cytokine hemoadsorption techniques. Currently, we have several devices for assessing cytokine adsorption; these include Cytosorb®(CytoSorbents Corporation,Monmouth Junction, NJ, United States), oXyris (Baxter, Meyzieu, France), Alteco LPS Adsorber (Alteco Medical AB, Lund, Sweden), HA 330 and 380 (Jafron Biomedical Co.,Zhuhai, GuangDong, China).
CytoSorb®is the most widely used cartridge, and our experience is greatest with it.It has been evaluated for various clinical conditions, such as SIRS after cardiopulmonary bypass, liver failure, and rhabdomyolysis-associated myoglobinemia[118-120 ]. In it, cytokines are adsorbed by polymer beads within a perfused cartridge,through extracorporeal circulation[117]. Cytosorb®can attenuate both the pro-inflammatory and anti-inflammatory responses, achieving a recovery of balance much earlier.
Several observational studies have suggested the clinical benefits of using Cytosorb®in septic shock to reduce vasopressor support and even achieve a mortality reduction.Frieseckeet al[124] studied 20 consecutive patients with refractory septic shock after 6 h of standard treatment and hypercytokinemia. Refractory septic shock was defined as a progressive shock despite full-standard therapy and lactate ≥ 2.9 mmol/L (or increased compared to baseline), and high noradrenaline requirements (> 0.3 mcg/kg/min). The mean IL-6 Levels were 25.523 ng/mL (range: 1052-491260 ng/mL). In that study, Cytosorb®application was found to be associated with a significant decrease in noradrenaline requirements and an increase in lactate clearance, which resulted in shock resolution in 13 patients. In another case series of 45 patients with septic shock treated with hemoadsorption, Paulet al[125] described a significant vasopressor dose reduction (i.e., norepinephrine by 51.4%, epinephrine by 69.4%, and vasopressin by 13.9%). Besides, a reduction in IL-6 Levels (by 52.3%) and lactate levels(by 39.4%) was observed in the survivors. A survival rate of 75% was reported in patients who received treatment within 24 h of admission to the ICU. Patients who received treatment within 24-48 h after admission to the ICU had a survival rate of 68%. In a retrospective study conducted by Brouweret al[126], Cytosorb®was associated with decreased 28-d all-cause mortality in patients with septic shock.
The scientific evidence on the clinical benefits of cytokine elimination derived from RCTs is scarce. Hawcharet al[127] performed a proof of concept, prospective,randomized pilot trial on the application of Cytosorb®in 20 patients with early-onset septic shock. A significant reduction in the need for vasopressor support was observed. In the control group, this change was not achieved with therapy. Rugget al[128] compared patients with septic shock who received CytoSorb®in addition to CRRT (n= 42)vsmatched controls (n= 42). Median catecholamine requirements approximately halved within 24 h after the initiation of Cytosorb®. In-hospital mortality was significantly lower in the CytoSorb®group (35.7%vs61.9%;P= 0.015).Derived from our current knowledge, we can attribute the benefits of cytokine hemoadsorption only to the elimination of cytokines in the subgroup of patients with very high hypercytokinemia and associated refractory septic shock. Further studies are needed to define the influence of hemadsorption in the elimination of other substances.
Cytokine hemoadsorption may have a role as rescue therapy in a particular subgroup of patients with refractory septic shock, hyperlactatemia, multiorgan failure,and very high hypercytokinemia. As such, appropriate and well-designed RCTs should be performed in patients with this clinical profile, to validate its benefits.
Immunoparalysis
More than 20 years ago, it was hypothesized that the early hyperinflammatory phase in sepsis was followed by a compensatory anti-inflammatory response to limit tissue damage[129]. In recent years, the therapeutic advances incorporated in sepsis treatment have facilitated a reduction in sepsis mortality, especially in early mortality derived from septic shock and severe multiorgan dysfunction. Some of the patients surviving the first few days evolve to a situation of chronic multiorgan dysfunction,dependent on mechanical ventilation and vasopressor therapy. This stage, known as sepsis-associated immunoparalysis, resembles the normal aging process of the immune system (immunosenescence), characterized by a general dysregulation of innate and adaptive immune responses. Monocytes and macrophages play a critical role in critically ill patients with severe infections. These cells are the front-line of the innate cellular response that initiates and promotes the adaptive immune response.
The human leukocyte antigen (HLA)-DR isotype is a major histocompatibility complex class II cell surface receptor encoded by the HLA complex and constitutively expressed on antigen-presenting cells (e.g., monocytes/macrophages, dendritic cells,and B lymphocytes). It is also inducible on T lymphocytes[130]. Decreased HLA-DR expression has been demonstrated in septic patients, at both the protein- and RNAlevels. There is also a relationship between circulating HLA-DR mRNA and HLA-DR expressionin vivo[131]. Various studiesin vitrohave shown that constitutive and IFN-γ inducible HLA-DR expression is predominantly regulated at the transcriptional level.The observed loss of HLA-DR expression in monocytes of septic patients implies a transcriptional regulationviaa decrease of its transactivator, specifically the class II transactivator (i.e., CIITA)[130].
Although no association has been found between the kinetics of monocytic(m)HLA-DR expression and primary infection sites or causative pathogens, it has been associated with severity. Patients with high SOFA scores have an associated low expression of mHLA-DR. The prognosis of patients with low mHLA-DR expression is poor compared to patients with a rapid increase in mHLA-DR expression, primarily because of the higher incidence of secondary infections and mortality rate[132]. The most reliable marker for monitoring the immune alterations in critically ill patients is the decreased mHLA-DR expression, measured by flow cytometry[133].
Immunoparalysis can be identified by studying the expression of HLA-DR in monocytes. Multiple studies have linked the low expression of mHLA-DR with the presence of more significant adverse effects and higher short and long-term mortality rates (at 7 d and 28 d) in sepsis and septic shock[134,135]. Measures of mHLA-DR levels can not only be used as a marker of monocyte functionality and severity of the disease but also to guide innovative clinical therapies based on restoring the immune system[135,136].
In patients with immunoparalysis, several immuno-adjuvant agents are under investigation. GM-CSF, IFN-g, anti-programmed death-ligand 1 (i.e., anti PDL-1), or IL-7 could have a role in treating sepsis-associated immunoparalysis. For instance,decreased mHLA-DR has been used to stratify patients for GM-CSF administration in a clinical trial, including a small sample of sepsis patients. This biomarker-guided GMCSF therapy was found to be safe and effective in restoring monocyte immunocompetence, shortening mechanical ventilation duration, and reducing ICU/hospital stay[135]. Another clinical trial tested the hypothesis that GM-CSF improves neutrophil phagocytosis in critically ill patients. They previously measured the neutrophil phagocytic capacity and included the subgroup of patients in whom phagocytosis was known to be impaired (to < 50%). The study showed that GM-CSF did not improve mean neutrophil phagocytosis but was safe and appeared to increase the proportion of patients with adequate phagocytosis[137]. Novel therapies targeting the restoration of monocyte immunocompetence are promising for improving outcomes in later stages of sepsis.
CONCLUSlON
The heterogeneity of sepsis is a complex and engaging feature of the disease that elicits novel strategies for improved patient classification. Thus, precision medicine creates an individualized approach on a case-by-case basis by identifying subgroups of sepsis patients with a high risk of adverse outcomes who may benefit from specific treatments or rescue therapies according to their particular characteristics (e.g.,genotypes or phenotypes). Of note, we urge the implementation of predictiveenrichment strategies for the design and development of future clinical trials to improve the certainty of scientific assessments.
Although some clinical tools are still being evaluated in the early stages of research,such as the omics technologies, precision medicine is becoming a reality that improves our clinical approaches when currently available tools are implemented in patients with sepsis, septic shock, and organic dysfunction. Further scientific contributions in this field will be essential to identify specific endotypes responding to targeted therapies and translate individualized treatments to the bedside.
 World Journal of Critical Care Medicine2022年1期
World Journal of Critical Care Medicine2022年1期
- World Journal of Critical Care Medicine的其它文章
- Acute exacerbation of interstitial lung disease in the intensive care unit
- Endotracheal intubation sedation in the intensive care unit
- Medico-legal risks associated to hand and wrist trauma
- Efficacy of remdesivir for hospitalized COVlD-19 patients with end stage renal disease
- Epidemiology of electrical burns and its impact on quality of life - the developing world scenario
